

Original Article - Year 2017 - Volume 32 -
Assessment of the quality of life and self-esteem of mastectomized patients submitted or not to breast reconstruction
Avaliação precoce da qualidade de vida e autoestima de pacientes mastectomizadas submetidas ou não à reconstrução mamária
ABSTRACT
INTRODUCTION: After diagnosis and treatment of breast cancer, some women go through physical, social, and emotional changes that often have an impact on their quality of life and self-esteem. This study aimed to assess the quality of life and self-esteem of mastectomized patients with or without breast reconstruction a month after surgery.
METHODS: The study consisted of 89 patients aged ≥ 30 years with or without breast reconstruction. They were recruited from the Plastic Surgery and Mastology clinic of São Paulo Hospital and Pérola Byington Hospital. Group 1 (n = 30) consisted of mastectomized patients without breast reconstruction; group 2 (n = 29) consisted of mastectomized patients with breast reconstruction; and group 3 (n = 30) consisted of patients without changes in the breasts. The EORTC QLQ-C30 and Rosenberg Self-Esteem Scale UNIFESP/EPM instruments, which are validated in Brazil, were used to assess their quality of life.
RESULTS: There were no observed effects in the quality of life and self-esteem of the patients who underwent mastectomy with or without breast reconstruction a month after surgery.
CONCLUSION: The women with mastectomy with or without breast reconstruction a month after surgery showed no changes in their quality of life and self-esteem when compared among themselves and to women with no cancer history. It is necessary that this assessment, employing the EORTC QLQ-C30 and QLQ-BR23 questionnaires, be performed from the time of breast cancer diagnosis until after breast reconstruction to identify the stage when the quality of life and self-esteem are affected.
Keywords: Neoplasms of the breast; Self-image; Breast augmentation; Mastectomy; Quality of life.
RESUMO
INTRODUÇÃO: Após o diagnóstico e tratamento do câncer de mama, algumas mulheres passam por alterações físicas, sociais e emocionais que repercutem muitas vezes na qualidade de vida e na autoestima. O objetivo é avaliar a qualidade de vida e autoestima de pacientes mastectomizadas submetidas ou não à reconstrução mamária após um mês de cirurgia.
MÉTODOS: A casuística foi composta por 89 pacientes, com idade igual ou superior a 30 anos, submetidas ou não à reconstrução mamária, e oriundas dos ambulatórios de Cirurgia Plástica e Mastologia do Hospital São Paulo e do Hospital Pérola Byington. O grupo 1 (n = 30) composto pelas pacientes mastectomizadas sem reconstrução mamária; o grupo 2 (n = 29) mastectomizadas com reconstrução mamária; e o grupo 3 (n = 30) pacientes sem alterações nas mamas. Para a avaliação da qualidade de vida, foram aplicados os instrumentos validados para uso no Brasil EORTC QLQ-C30 e Escala de Autoestima de Rosenberg UNIFESP/EPM.
RESULTADOS: Não foram observadas repercussões na qualidade de vida e autoestima das pacientes submetidas à mastectomia com ou sem a reconstrução mamária após um mês de cirurgia.
CONCLUSÃO: Mulheres mastectomizadas com ou sem reconstrução mamária após um mês da cirurgia não apresentaram repercussões na qualidade de vida e na autoestima, quando comparadas entre si, bem como comparadas às mulheres sem história de câncer. É necessário que este tipo de avaliação, por meio dos questionários EORTC QLQ-C30 e QLQ-BR23, seja realizado no momento do diagnóstico do câncer de mama até o momento da pós-reconstrução mamária, com a finalidade de identificar em que fase se instalam as repercussões na qualidade de vida e autoestima.
Palavras-chave: Neoplasias da mama; Autoimagem; Mamoplastia; Mastectomia; Qualidade de vida.
Breast cancer is the second most frequent type of cancer in the world and is the most common among women, accounting for approximately 25% of new cases each year. In Brazil, 57,960 new cases of breast cancer were expected in 2016, with an estimated risk of 57 cases in every 100,000 women1.
Considering the changes and effects that this disease and its treatment may cause, all breast cancer-related studies must be considered. Prevention, patient rehabilitation by the various professionals involved, physical and psychological damage repair, and its influence on the quality of life and self-esteem should be taken into account. In addition, if breast cancer is associated with mastectomy, then there will be loss of the ability to perform tasks, as well as lowering of self-esteem, causing reduction in quality of life2,3.
The term "quality of life" was introduced for the first time by the President of the United States, Lyndon Johnson, in 1964; he stated that goals cannot be measured by the balance sheet of banks. They can only be measured by the quality of life that it provides for people4. An important component of quality of life is self-esteem, defined as the feeling, consideration that a person has for themselves, how much they love themselves, i.e., how they see themselves, and what they think of themselves. Being self-conscious of their own appearance may affect their self-confidence and self-esteem5.
The interest for the study of quality of life and self-esteem has grown in Brazil and worldwide. Nevertheless, standardization of instruments to assess quality of life in the early postoperative period of a month after mastectomy with or without breast reconstruction and its impact on quality of life and self-esteem have not been found in the literature.
This finding stimulated the current study, because patients seeking dermatological physiotherapy could not precisely answer when they noticed that negative feelings had taken space in their thoughts and how much these had influenced their quality of life and self-esteem during physiotherapeutic assessments.
The importance of knowing the period when the new reality influences a patient's quality of life and self-esteem after mastectomy with or without breast reconstruction was considered for both patients with breast cancer and the multidisciplinary team. Further, understanding how these data could be used to monitor their treatment and healing process, compare different stages of a patient's evolution, facilitate clinical decision-making, and employ the most adequate therapy, as well as determine the kind of family, social, labor, and medical care that should be adopted is important.
This survey was conducted using the Rosenberg Scale UNIFESP/EPM, since it is a validated instrument in Brazil that assesses self-esteem. However, there is no standard tool yet for assessing the quality of life of patients with breast cancer. Thus, the European Organization for Research and Breast Cancer Treatment-Specific Quality of Life Questionnaire (EORTC QLQ-C30) was selected because it is an instrument that specifically assesses the quality of life of patients with cancer and is validated worldwide.
OBJECTIVE
To evaluate the quality of life and self-esteem of mastectomized patients with and without breast reconstruction a month after surgery.
METHODS
This was a primary, observational, cross-sectional, comparative, and analytical study. This study was approved by the Ethics and Research Committee of the Federal University of São Paulo under number 188.615, as well as the Ethics and Research Committee of Pérola Byington Hospital under number 054/11.
Data from 90 female patients were analyzed, and 89 patients were included in the period between August 2013 and August 2015. All patients who underwent mastectomy were evaluated a month after the surgery at the Plastic Surgery Clinic of São Paulo Hospital of UNIFESP-EPM, Pérola Byington Hospital, and the Brazilian Institute of Cancer Control.
The patients were classified into three groups. Group 1 (n = 30) consisted of mastectomized patients without breast reconstruction; group 2 (n = 29) consisted of mastectomized patients with breast reconstruction; and group 3 (n = 30) consisted of patients without breast changes. The patients signed the Informed Consent Form and answered the Rosenberg UNIFESP/EPM and EORTC QLQ-C30 questionnaires in a single session.
Assessment of eligibility for participation in the study was based on the following criteria: 1) Inclusion: female sex, mastectomy with or without breast reconstruction a month prior to the study, and age ≥ 30 years; 2) Exclusion: refusal to participate in the study, presenting double answers in the questionnaires, radiotherapy and chemotherapy treatment, and history of conservative breast surgery, such as sectorectomy and quadrantectomy.
RESULTS
To meet the proposed objective, a statistical analysis of the demographic data, self-esteem, and EORTC QLQ-C30 questionnaire results was performed by calculating the mean and standard deviation (SD). ANOVA was employed to compare the between-group means. The Chi-square test was employed to verify the associations between two categorical variables; alternatively, the Fisher's exact test was employed in a small number of casuistry cases. The Cronbach's alpha assessed the internal consistencies of the EORTC QLQ-C30 and Rosenberg UNIFESP/EPM scale items.
A significance level of 5% was adopted for all statistical tests.
Regarding the descriptive analysis of the sample, the study investigated 89 patients aged 50.3 years on average (SD = 11.0 years). A minimum age of 31 years and a maximum age of 74 years were observed. With regard to the level of education, the majority of group 1 subjects (60.0%) and 61.5% of group 2 subjects had finished high school, while 33.3% of group 3 subjects were mostly composed of volunteers who finished higher education.
Regarding marital status, 63.3% of group 1 subjects, 44.8% of group 2 subjects, and 66.7% of group 3 subjects were married. Further, 20% of group 1 subjects, 24.1% of group 2 subjects, and 10.0% of group 3 subjects were single. Divorced women accounted for 0.0% in group 1, 20.7% in group 2, and 13.3% in group 3. Widows accounted for 16.7% in group 1, 10.3% in group 2, and 10% in group 3.
With regard to the affected breasts, 50.0% of group 1 subjects (mastectomized patients without breast reconstruction) had an affected left breast, while 48.3% of group 2 subjects (mastectomized patients with breast reconstruction) had an affected right breast. Both breasts were affected in 3.3% of group 1 subjects and 6.9% of group 2 subjects.
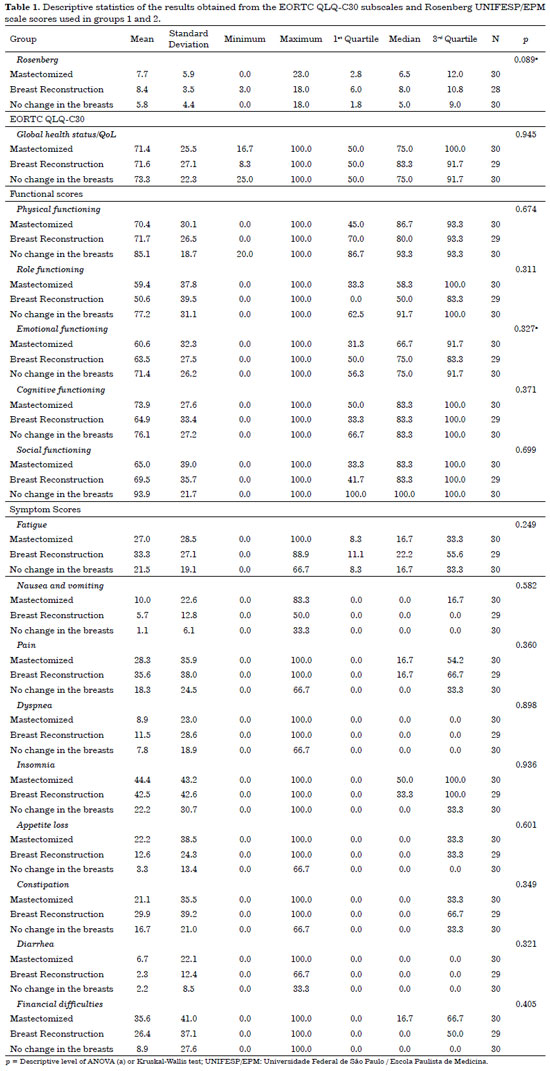
Table 1 shows the descriptive statistics of the results obtained from the EORTC QLQ-C30 subscales and Rosenberg UNIFESP/EPM scores used in groups 1 and 2; in addition, it shows that there is no difference in the means per group for the Rosenberg UNIFESP/EPM scores or EORTC QLQ-C30 subscales.
DISCUSSION
To date, cancer diagnosis is still perceived as an important event, considering that the diagnosis creates a negative impact on the patients' lives. Breast cancer may cause feelings, such as fear of mutilation, social prejudices, fear of death, depression, and social devaluation6. The effects on quality of life and self-esteem are other important factors determined after diagnosis and treatment.
In the beginning of the 20th century, the idea of cancer as a death sentence was modified with medical advances on understanding the oncological disease. The discovery of new treatments has paved the way to healing possibilities and began transforming the disease landscape, thus bringing hope of greater survival for many cases7.
Patient assessment for both group 1 (mastectomy without reconstruction breast) and group 2 (mastectomy with breast reconstruction) was performed a month after surgery, because that is when the recovery phase had not settled yet, with the purpose of evaluating whether there were repercussions on the quality of life and self-esteem.
This postoperative time is consistent with that from other studies that evaluated the quality of life of mastectomized women with and without breast reconstruction at the time of intervention, a month later, and six months after surgery8. In another study corroborating these findings, the authors reviewed the literature on the quality of life of patients who underwent mastectomy, compared with those who underwent conservative surgery in a period between 1 month and 2 years after surgery9. In a study by Furlan et al.10, the quality of life and self-esteem of mastectomized patients with and without breast reconstruction were also evaluated a month after surgery.
The average age of the subjects in the current study was 50.3 years (SD = 11.0 years). In group 1 (mastectomy without reconstruction breast), the subjects were aged 54.9 ± 12 years; in group 2 (mastectomy with breast reconstruction), the subjects were aged 50.9 ± 10.2 years; and in group 3 (without change in the breasts), the subjects were aged 45.0 ± 8.5 years. These data were consistent with the following literature findings. The mastectomized patients were aged 52.0 ± 13.98 years on average; in the mastectomy with breast reconstruction group, the subjects were aged 48.27 ± 10.48 years10. In another study, the mastectomized patients without breast reconstruction were aged 50.5 ± 7.4 years on an average11.
With regard to the level of education in this study, there was an association between schooling and their group (p < 0.001). Group 3 (without breast changes) had a greater higher education percentage (33.3% of the subjects) than the other groups; 45.3% of groups 1 and 2 finished high school.
In a study by Furlan et al.10, most of the mastectomized patients without breast reconstruction (45.5% of the subjects) finished high school, while the mastectomized patients with breast reconstruction mostly consisted of volunteers who finished high school, accounting for 45.5% of the subjects. The only volunteer who finished university (9.1%) was included in the mastectomy with breast reconstruction group. According to Veiga et al.11, 45 patients, i.e., 77.6% of the mastectomized patient group, had received basic education only (up to 8 years).
In this study, there were no associations between marital status and the group (p = 0.101). However, 58.4% of the patients of both groups were married. Both in group 1 (mastectomy without reconstruction breast) and group 2 (mastectomy with breast reconstruction), there was 31.5% of commitment to both sides of the breasts. No statistical difference was found.
Furlan et al.10 found a prevalence of 63.6% of impairments in the left breast in the mastectomy without breast reconstruction group and 54.5% in the mastectomy with breast reconstruction group. In this study, the EORTC QLQ-C30 questionnaire was used to assess the quality of life of the patients with cancer, and the Rosenberg Self-Esteem Scale UNIFESP/EPM was used to assess their self-esteem. Both questionnaires were validated and translated into Portuguese.
Similarly, Vieira et al.12 stated that the SF-36 instrument was a general quality-of-life questionnaire not exclusive to patients with cancer. Conversely, the EORTC QLQ-C30 questionnaire evaluated the quality of life of patients with cancer in general. In another research study, the lack of consensus on the use of questionnaires to assess quality of life was demonstrated, reporting that some researchers used instruments made by themselves9.
More recent studies have been correlating health with quality of life, which is a new stage to be reached because historically, the results of various treatments on this disease have been primarily measured in terms of cure, morbidity, and mortality3; nonetheless, the effects on quality of life and self-esteem of patients a month after surgery were not identified because they were believed to worsen in these indexes, especially in group 1 patients (without mastectomy breast reconstruction).
However, this was not the result obtained. This result could be justified by the fact that the patients are still involved with disease treatment and relief due to lumpectomy, especially when facing the "death sentence." Moreover, if patients are more focused on the disease treatment and less focused on their personal image, the psychological repercussions will not be observed. In addition, it is believed that these patients have not had the real perception of the effect on their personal image yet, i.e., the positive or negative impact that the surgery may have promoted both after mastectomy or breast reconstruction.
In this study, no changes were found in the quality of life of the patients after breast reconstruction a month after surgery because it is thought that some factors could have influenced the results: (a) overcoming the period of diagnosis to "death"; (b) the hypothesis that at this stage, there was no time for a patient to adapt to her self-image yet, which is one of the aspects of self-esteem. The perception of appearance remains unaltered because of the signs and symptoms presented by the patients; and (c) normal incongruity between physical reality of appearance (the way a patient is seen by others) and the perception of appearance (the way a patient judges her appearance), both regarding the body in general and the breast specifically.
Avelar et al.13 stated that the quality of life of patients with breast cancer tends to improve in the first weeks after surgery; however, it is essential that these patients be monitored and evaluated during the postoperative treatment period to verify the evolution of signs and symptoms, especially anxiety and depression.
In this study, the effects on the quality of life and self-esteem of the patients were not observed after using the EORTC QLQ-C30 and Rosenberg Self-Esteem Scale UNIFESP/EPM questionnaires. It must be pointed out that the 1-month postoperative period is very recent, with the appearance of important signs, such as edema, and expected functional limitations. A patient may receive guidance from the plastic surgeon not to make sudden movements or those above 90º with the upper limbs, for instance.
Another limiting factor is the pain arising from the procedure itself, difficulty of finding an appropriate sleep position, and other physical limitations. Furlan et al.10 evaluated 22 mastectomized volunteers with and without breast reconstruction a month after surgery. Greater emotional vulnerability was found in the group without breast reconstruction.
In their study, Veiga et al.14 found that breast reconstruction after mastectomy promoted positive changes in the participants' quality of life 3, 6, and 12 months after surgery. The authors also found that patients submitted to mastectomy followed by breast reconstruction at least a year before research may display improvements in quality of life.
Using a questionnaire specifically designed to assess quality of life instead of using a generic questionnaire would be interesting. Veiga et al.14 used the SF-36 questionnaire. This study recommends that EORTC be used, because it is specifically designed to assess the quality of life of patients with cancer.
Quality of life tends to improve over time, and instruments should be used at different stages after intervention to monitor possible changes. Furthermore, evidence has suggested that the most delicate time to assess quality of life is the first few months after surgery9.
Therefore, this study evaluated the patients in the immediate postoperative period (1 month) to design a profile for these patients and verify when the possible psychological changes occurred. It is important to consider the difficulties in scheduling the return of the study patients in the following months owing to their various limitations. Nonetheless, the importance of this mapping lies in the viability of planning better treatment and rehabilitation for the patients and their illness with the team of doctors, physical therapists, nurses, caregivers, and family, etc.
Self-esteem is directly related to psychological and physical issues, confirming the importance of having positive feelings about oneself in several experiences. In addition, a high self-esteem during the period of diagnosis, treatment, and follow-up of breast cancer could positively influence these patients' quality of life, favoring their physical, psychological, and emotional well-being15.
A sense of bodily integrity is essential to human beings, and mastectomy leads to loss of the ability to perform daily tasks and lowering of self-esteem, contributing to a decline in their quality of life3. In this study, perception of positive or negative aspects was not identified by the instruments used. The patients stated that their biggest concern was the disease, but not their new body reality and that God had made them go through this situation as a way of learning.
They emphasized that religious practices could affect their perception of life, which may help them cope with cancer. Although this study did not aim at investigating issues concerning beliefs and spirituality and no validated questionnaire was used to assess these issues, it was considered important to devote due attention to these parameters because it is at the time of human frailty that people seek a superior Being, respecting each patient's belief.
Rohani et al.16 investigated 254 patients with breast cancer in relation to quality of life and religious aspects. They used the EORTC QLQ-C30 questionnaire, Questionnaire of Antonovsky's Sense of Coherence, Spiritual Perspective of Scale, and Religious Scale instruments in the pre-diagnosis phase and 6 months after the diagnosis of breast cancer. They concluded that pre-diagnosis assessments could identify patients with risks of worsening quality of life and that religious aspects could exert a positive or negative influence in these patients' quality of life.
Another study found that patients with a history of breast cancer had better religiosity and spirituality levels, which were positively correlated with their quality of life17.
Issues relating to appearance and behavioral patterns are linked to the media and society and would be determined by the individuals themselves5. In this study, there were no negative repercussions in self-esteem in the 1-month postoperative period of the groups.
However, monitoring these patients at the outpatient clinic for a period between 18 and 24 months after mastectomy with or without breast reconstruction would be interesting. This could be conducted with the purpose of identifying when the changes in the self-esteem or quality of life occur. The physical therapist's role and performance are considered, focusing on the period when rehabilitation should be conducted. Further, the various available therapies that could favor patients' recovery in general are to be considered, encompassing body image improvement, self-esteem, quality of life, functionality, and adaptation to a new reality.
Veiga et al.14 reported that breast reconstruction should be offered to all patients after mastectomy if positive effects on the quality of life are found. During diagnosis, treatment, and breast cancer follow-up, a high self-esteem will positively favor quality of life and influence physical, psychological, and emotional well-being15.
Conducting studies with effective interventions to support health professionals' practice, guaranteeing qualified care and consequently improving the quality of life of patients with cancer is of paramount importance18. In this study, there were no significant changes in the 1-month postoperative period in group 2 (mastectomy with breast reconstruction) compared with group 1 (without mastectomy breast reconstruction). Certainly, the diagnosis of cancer is still associated with the fear of death; another important factor mentioned by the patients was the context of faith and hope in God that strengthened and helped them face all challenges.
Based on this study, it seems relevant that assessing self-esteem and quality of life of patients submitted to surgery to treat breast cancer should be conducted more efficiently by health professionals and researchers at several periods of coping with cancer. Its diagnosis, together with medical, surgical, and psychological treatment, and its physiotherapeutic rehabilitation must be dealt with. Moreover, the difficulty of identifying whether the patients already had changes in their personal image, self-esteem, and quality of life at the time of diagnosis or whether the effects would arise after lumpectomy or breast reconstruction should be considered as well.
Studies conducted in 2009, which reported consistent findings, highlighted the importance of conducting further research correlating the patients' functional capacity owing to the difficulty in assessing if a function is preserved in the postoperative period or if evaluation parameters in the preoperative stage; this information would be relevant to enable doctors to measure their patients' perceived health and assess the benefit of their intervention. This would make the treatment more objective, considering that the patient would be treated by a multidisciplinary team, promoting greater diagnostic accuracy for referral to specific professionals. Thus, this would contribute to an increasingly better evolution regarding quality of life and self-esteem19.
According to the statistical analysis performed in this study, several functional and symptomatic EORTC QLQ-C30 questionnaire subscales revealed that groups 1 and 2 showed no significant effects in their quality of life when compared with those in the immediate postoperative period.
Nevertheless, when the scale of symptoms "Did you feel angry easily?" was analyzed alone, group 2 (mastectomy with breast reconstruction) subjects had a higher percentage of "moderately" responses (20.7% of the subjects), while group 1 (without mastectomy breast reconstruction) had the lowest percentage (10.0% of the subjects). Group 3 subjects (without breast changes) had a higher percentage of "little" responses (43.3% of the subjects). This might have occurred because the group had 63.3% of the patients attending higher education, in which the degree of demand and stress was even greater.
These findings are in accordance with a statement by Oliveira et al.8 stating that patients in the first month after mastectomy with or without breast reconstruction have a reduced independence index, which may cause irritability.
In this scale of symptoms in this study, the patients were asked if "they felt weak and had no appetite"; 20.7% of group 2 subjects (mastectomy with breast reconstruction) answered moderately, and 93.3% of group 3 subjects (without changes of breasts) answered they did not lack appetite.
This suggests that group 2 (mastectomy with breast reconstruction) was in the first postoperative month. Therefore, limitations were evident owing to the major surgery performed, and in this phase, patients need physiotherapeutic guidelines regarding adaptation to daily living activities (DLAs), as well as guidelines for their caregivers and family. Thus, DLAs will be gradually resumed, and the patients will feel more motivated and eat better, without displaying weakness symptoms.
Another factor observed in this study included the question "Has your physical condition or the medical treatment interfered in your family life?" Group 3 (without breast changes) had a higher percentage of "no" answers (90.0% of the subjects) than the other groups because they consisted of healthy subjects, i.e., without changes in the breasts. Group 1 (mastectomized without breast reconstruction) had the highest percentages of "little" responses (20.0% of the subjects) and "very " responses (26.7% of the subjects) among the groups.
These results possibly arose from the limitations of the surgical intervention and care imposed on the patients in the first months. According to Rondelo et al.20, reconstructive plastic surgeries are not supposed to make an individual happier or sadder but to assist them with their physical and emotional aspects.
In this study, the patients were asked, "Has your physical condition or medical treatment interfered in your social activities?" Group 2 subjects (mastectomy with breast reconstruction) had a higher percentage of "moderately" responses (31.0% of the subjects) than the other groups. However, group 3 subjects (without breast change) had a higher percentage of negative responses (93.3% of the subjects), because they did not undergo any surgical intervention.
Conversely, research conducted by the WHOQOL-100 at the date of hospitalization a month after breast reconstruction surgery and 6 months later did not identify changes in areas related to physical, social, and environmental changes at the three periods of assessment8. Another study performed in the pre- and postoperative periods 3 and 6 months by the Health Assessment Questionnaire aimed at evaluating functional capacity at the first time of surgery after breast reconstruction in 36 patients.
They concluded that there was a decrease in the functional capacity of the patients submitted to late breast reconstruction with TRAM. These findings were relevant and acceptable owing to the occurrence of important anatomical manipulations resulting from breast reconstruction. Further, they could cause discomfort or physical adaptations, as well as transient or definitive postural changes, considering each patient's individuality and emotional fragility19.
In the question "Has your physical condition or the medical treatment brought financial difficulties?", group 1 (without mastectomy breast reconstruction) subjects had a lower percentage of "no" responses (50.0% of the subjects) than the other groups. It is believed that the presence of this factor comes from the treatment offered in the Unified Health System (SUS). Conversely, group 3 (without breast change) subjects had a higher percentage of negative responses (90.0% of them), since all of them were actively employed.
This result corroborates the findings of Sawada et al.21, although their study employs another methodological approach. The authors found that despite the complexity and cost of the treatment, this fact did not bring significant financial difficulties in the patients with cancer, and the SUS service had provided full treatment coverage.
Alternatively, prospective studies should be performed using the EORTC QLQ-C30 questionnaire and QLQ-C30 BR23-specific module to assess the quality of life of patients with breast cancer, as well as the Spiritual Perspective of Scale, Religious Scale, and Personal Image, Depression, and Anxiety instrument. These cover items from the time of diagnosis until the last surgical intervention and even after patient discharge to analyze the existence of a psychological change or image disturbance in the pre-diagnosis of breast cancer, as well as the presence of symptoms and side effects related to different treatment modalities, negatively or positively impacting body image, sexuality, spirituality, religiosity, and prospects at all stages of the treatment proposed by the multidisciplinary team.
CONCLUSION
The mastectomized women with or without breast reconstruction a month after surgery displayed no changes in their quality of life and self-esteem when compared among themselves and to women with no cancer history. It is necessary that this assessment, employing the EORTC QLQ-C30 and QLQ-BR23 questionnaires, be performed from the time of breast cancer diagnosis until after breast reconstruction to identify at the stage at which the quality of life and self-esteem are affected.
COLLABORATIONS
VLA Writing the manuscript or critical review of its contents.
MSN Final approval of the manuscript.
LEFA Final approval of the manuscript.
CJRO Final approval of the manuscript.
LMF Final approval of the manuscript.
REFERENCES
1. Brasil. Ministério da Saúde. Inca: Instituto Nacional do Câncer. Tipos de Câncer. [acesso 2017 Abr 27]. Disponível em: http://www2.inca.gov.br/wps/wcm/connect/tiposdecancer/site/home/mama
2. Manuel J, Kokuba EN, Sabino Neto M, Santos AS, Ferreira LM. Perfil de pacientes submetidas à reconstrução mamária tardia atendidas em hospital universitário do município de São Paulo. Saúde Coletiva. 2010;7(39):82-6.
3. Sabino Neto M, Moreira JR, Resende V, Ferreira LM. Nível de atividade física em mulheres mastectomizadas e submetidas a reconstrução mamária. Rev Bras Cir Plást. 2012;27(4):556-61. DOI: http://dx.doi.org/10.1590/S1983-51752012000400015
4. Fleck MPA, Leal OF, Louzada S, Xavier M, Chachamovich E, Vieira G, et al. Desenvolvimento da versão em português do instrumento de avaliação de qualidade de vida da OMS (WHOQOL-100). Rev Bras Psiquiat. 1999;21(1):19-28. DOI: http://dx.doi.org/10.1590/S1516-44461999000100006
5. Dini GM, Quaresma MR, Ferreira LM. Adaptação Cultural e Validação da Versão Brasileira da Escala de Auto-estima de Rosenberg. Rev Bras Cir Plást. 2004;19(1):47-52.
6. Makluf ASD, Dias RC, Barra AA. Avaliação da qualidade de vida em mulheres com câncer da mama. Rev Bras Cancerol. 2006;52(1):49-58.
7. Carvalho MM. Psico-oncologia: história, características e desafios. Psicol USP. 2002;13(1):151-66. DOI: http://dx.doi.org/10.1590/S0103-65642002000100008
8. Oliveira RR, Morais SS, Sarian LO. Efeitos da reconstrução mamária imediata sobre a qualidade de vida de mulheres mastectomizadas. Rev Bras Ginecol Obstet. 2010;32(12):602-8. DOI: http://dx.doi.org/10.1590/S0100-72032010001200007
9. Majewshi JM, Lopes ADF, Davoglio T, Leite JCC. Qualidade de vida em mulheres submetidas à mastectomia comparada com aquelas que se submeteram à cirurgia conservadora: uma revisão de literatura. Ciênc Saúde Coletiva. 2012;17(3):707-16. DOI: http://dx.doi.org/10.1590/S1413-81232012000300017
10. Furlan VLA, Sabino Neto M, Abla LEF, Oliveira CJR, Lima AC, Ruiz BRO, et al. Qualidade de vida e autoestima de pacientes mastectomizadas submetidas ou não a reconstrução mamária. Rev Bras Cir Plást. 2013;28(2):264-9. DOI: http://dx.doi.org/10.1590/S1983-51752013000200016
11. Veiga DF, Campos FSM, Ribeiro LM, Archangelo Junior I, Veiga Filho J, Juliano Y, et al. Mastectomy versus conservative surgical treatment: the impact on the quality of life of women with breast cancer. Rev Bras Saúde Matern Infant. 2010;10(1):51-7. DOI: http://dx.doi.org/10.1590/S1519-38292010000100005
12. Vieira RAC, Silva FCB, Biller G, Silva JJ, Paiva CE, Sarri AJ. Instrumentos de avaliação quantitativa e qualitativa das sequelas relacionadas ao tratamento do câncer de mama. Rev Bras Mastologia. 2016;26(3):126-32. DOI: http://dx.doi.org/10.5327/Z201600030008RBM
13. Avelar AMA, Derchain SFM, Camargo CPP, Lourenço LS, Sarian LOZ, Yoshida A. Qualidade de vida, ansiedade e depressão em mulheres com câncer de mama antes e após a cirurgia. Rev Ciênc Méd. 2006;15(1):11-20.
14. Veiga DF, Sabino Neto M, Ferreira LM, Garcia EB, Veiga Filho J, Novo NF, et al. Quality of life outcomes after pedicled TRAM flap delayed breast reconstruction. Br J Plast Surg. 2004;57(3):252-7. PMID: 15006527 DOI: http://dx.doi.org/10.1016/j.bjps.2003.12.029
15. Gomes NS, Soares MBO, Silva SR. Autoestima e qualidade de vida de mulheres submetidas à cirurgia oncológica de mama. REME Rev Min Enferm. 2015;19(2):120-6.
16. Rohani C, Abedi HA, Omranipour R, Langius-Eklöf A. Health-related quality of life and the predictive role of sense of coherence, spirituality and religious coping in a sample of Iranian women with breast cancer: a prospective study with comparative design. Health Qual Life Outcomes. 2015;13:40. DOI: http://dx.doi.org/10.1186/s12955-015-0229-1
17. Wildes KA, Miller AR, de Majors SS, Ramirez AG. The religiosity/spirituality of Latina breast cancer survivors and influence on health-related quality of life. Psychooncology. 2009;18(8):831-40. DOI: http://dx.doi.org/10.1002/pon.1475
18. Zandonai AP, Cardozo FMC, Nieto ING, Sawada NO. Qualidade de vida nos pacientes oncológicos: revisão integrativa da literatura latino-americana. Rev Eletr Enferm. 2010;12(3):554-61.
19. Kobayashi LA, Aquino MS, Garcia BE, Sabino NETO M, Ferreira LM. Capacidade funcional após reconstrução mamária tardia com retalho TRAM pediculado. ACM Arq Catarin Med. 2009;38(1):64-6.
20. Rondelo JC, Di Martino M, Mermerian T, Veiga DF, Abla LEF, Gebrin LH, et al. Qualidade de vida em pacientes submetidas à reconstrução de mama com retalho miocutâneo transverso do reto abdominal. Rev Bras Cir Plást. 2014;29(1):79-83.
21. Sawada NO, Nicolussi AC, Okino L, Cardozo FMC, Zago MMF. Avaliação da qualidade de vida de pacientes com câncer submetidos a quimioterapia. Rev Esc Enferm USP. 2009;43(3):581-7. DOI: http://dx.doi.org/10.1590/S0080-62342009000300012
1. Universidade Federal de São Paulo, São Paulo, SP, Brazil
2. Universidade Anhembi Morumbi, São Paulo, SP, Brazil
Institution: Universidade Federal de São Paulo, São Paulo, SP, Brazil.
Corresponding author:
Vanessa Lacerda Alves
Rua Santa Izabel, 555, Bloco A, Apto 61 - Vila Augusta
Guarulhos SP, Brazil Zip Code 07023-022
E-mail: vanessa.lacerda@yahoo.com.br
Article received: October 25, 2016.
Article accepted: April 23, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter