

Original Article - Year 2017 - Volume 32 -
Breast augmentation: correlation between surgical planning and complication rates after surgery
Mamoplastia de aumento: correlação entre o planejamento cirúrgico e as taxas de complicações pós-operatórias
ABSTRACT
INTRODUCTION: Breast implants remain a very popular option both for aesthetic and reconstructive plastic surgeries. A number of factors can affect the results of breast implant surgeries. The adequate planning on incision placement, need to associate mastopexy, insertion plane, and implant model increase the likelihood of adequate outcomes and reduce the need for secondary surgical treatment. This study describes the experience of a Plastic Surgery Service at the Hospital de Clínicas de Porto Alegre from 2011 to 2016 by correlating surgical planning with complication rates and surgical reintervention.
METHODS: A retrospective cohort that analyzed patients who underwent breast implants at the Hospital de Clínicas de Porto Alegre between 2011 and 2016, and included only cases of aesthetic breast augmentation, associated or not with mastopexy. All patients had their records analyzed, and after that an interview by phone was conducted to complement the information of the questionnaire. The analyzed was concluded with an appointment with a plastic surgeon of the service who examined the patient and confirmed the data collected for the questionnaire. No patients was evaluated by the assistant surgeon in last examination.
RESULTS: There was no significant difference between variation in surgical planning and incidence of complications.
CONCLUSION: Still, no consensus exists regarding the best access route and plan for the breast implant. Further studies are necessary to compare the different routines of each service. Currently, best results are still based on routine systematization, precise surgical dissection and minimal contamination.
Keywords: Mammoplasty; Postoperative complications; Breast implantation.
RESUMO
INTRODUÇÃO: Os implantes mamários continuam sendo uma opção muito popular tanto para pacientes de cirurgia plástica estética quanto reconstrutora. Existem múltiplos fatores que podem afetar os resultados de cirurgias com implante mamário. Um adequado planejamento sobre o posicionamento da incisão, necessidade de associar mastopexia, plano de inserção e modelo do implante aumentam a probabilidade de resultados adequados e minimizam a necessidade de tratamento cirúrgico secundário. Estudo realizado para descrever a experiência do serviço de Cirurgia Plástica do Hospital de Clínicas de Porto Alegre entre 2011 e 2016 correlacionando o planejamento cirúrgico realizado com as taxas de complicações e reintervenção cirúrgica.
MÉTODOS: Coorte retrospectiva que analisou os pacientes submetidos a implantes mamários no Hospital de Clínicas de Porto Alegre entre 2011 e 2016, sendo incluídos somente casos de mamoplastia de aumento estética, associada ou não à mastopexia. Todos os pacientes tiveram seu prontuário analisado; posteriormente, realizou-se uma ligação telefônica para complementar as informações do questionário. Finalizou-se com uma consulta com um cirurgião plástico do serviço, que examinou a paciente e confirmou os dados coletados para o questionário, não sendo em nenhum caso o cirurgião assistente.
RESULTADOS: Não há diferença significativa entre a variação no planejamento cirúrgico e a incidência de complicações.
CONCLUSÃO: Ainda não há consenso quanto à melhor via de acesso e plano do implante mamário, sendo necessários estudos comparando as diferentes rotinas de cada serviço. No momento os melhores resultados ainda são baseados numa rotina sistematizada, dissecção cirúrgica precisa e contaminação mínima.
Palavras-chave: Mamoplastia; Complicações pós-operatórias; Implante mamário.
Breast implants are still a popular choice for both patients of aesthetic and reconstructive plastic surgery. Breast augmentation had a 64% increase in the number of procedures performed since 2000, and it became one of the most performed aesthetic surgery in the world.
In Brazil, this is the second most common aesthetic surgery with 185,042 augmentation mammoplasties carried out in 20141. Several studies have described both complication rates as the reoperation rates this population2-4. There are multiple factors that can affect the results of surgery with breast implant including: selection of patients, effective guiding the patient, planning for implant localization, incision location, choose of implant, surgical technique and postoperative care.
The inefficiency in any step in the treatment may result in an increased rate of complications and surgical reoperations5. Proper analysis of the physical characteristics of the patient, chest size and possible asymmetries, with the participation of the patient in the choice of the prosthesis are the most important factors in selecting the implant volume6.
The knowledge about the position of the implant and aseptic handling concepts contribute to good results and minimize the need for surgical secondary treatment7.
Patient's satisfaction is high with this procedure, despite significant reoperation rates to treat capsular contracture, asymmetry, scar revision or other complications8.
As for surgical technique options to perform mammoplasty augmentation, there are three main decisions: the access route, anatomical plan, and type of implant used. The most popular access routes are the inframammary incision, periareolar, axillary and mastopexy associated with the inclusion of prosthesis. Regarding the plan used, the options currently accepted are subglandular, subfascial, submuscular and dual plane. Regarding the type of prosthesis, there are numerous variations. The two shapes available are anatomical and round. However, no consensus exists on what standard approach to adopt in mammoplasties augmentation, and they differ from the conducts described in the literature4,9-11.
OBJECTIVE
This study correlated surgical planning with complication rates and surgical reintervention of breast augmentation.
METHODS
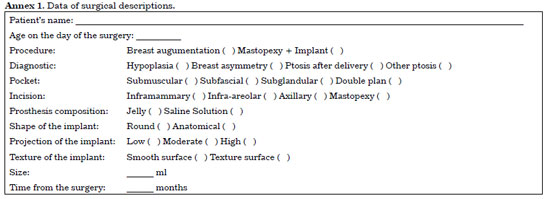
This retrospective cohort study analyzed patients who underwent breast implantation at the Hospital de Clínicas/Porto Alegre between 2011 and 2016. We included only cases of aesthetic breast augmentation associated or not with mastopexy. All patients had their records reviewed, data confirmed by phone and recorded on the evaluation form (Annexs 1 and 2). The analysis was concluded with an appointment with a plastic surgeon of the service to define score of Baker12 and Stony Brook Scar Evaluation Scale13. No patients was evaluated by the assistant surgeon in last examination.
The Stony Brook Scar Evaluation Scale13 was used for objective assessment of the quality of late scar.
Exclusion criteria were: breast tuberous, congenital deformity of the thorax, reconstructive surgery, revision surgery or non-attendance at the evaluation of the surgeon to update the data and define the scores.
All data were typed in a Microsoft Excel 2013 spreadsheet file. We considered that all isolated augmentation mammoplasties were performed with inframammary incision or infra-areolar approach, and all implant-associated mastopexy were performed with inverted T-incision. The access route techniques were correlated, as well as the dissection plans performed and the shape of the prosthesis chosen, comparing the surgical planning with the outcomes of complications and reinterventions. To analyze better the rates of major complications, reintervention and the Stony Brook Scar Evaluation Scale, data were classified by breast; total of 100 breasts.
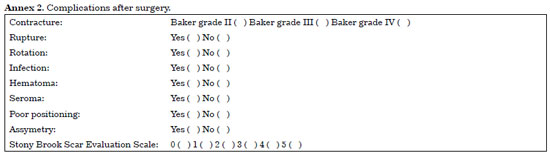
For statistical analysis, we used the Statistical Package for Social Studies (SPSS) (IBM Corp. Released 2012; SPSS Statistics for Windows, Version 21.0 Armonk, NY: IBM Corp.). As major postoperative complications, we analyzed capsular contracture by Baker's scale, rupture, rotation, infection, extrusion, hematoma, seroma, pain, malposition and asymmetry. The characteristics of the scar were evaluated according to the Stony Brook Scar Evaluation Scale.
Preoperative Evaluation
All patients perform preoperative exams; blood count, chest X-rays, thrombin time, activated partial thromboplastin time, electrocardiogram. Women younger than 40 years underwent breast ultrasound or mammogram if any risk factor existed or if it was not done during patient last screening tests. Other exams were requested depend on comorbidities presented by the patient.
The volume of the prosthesis is chosen according to the measures of patient's base of breast and then discussed to the same size possibilities within limits that respect the mammary platform. The anatomical plane is chosen as the "pinch test" of patient if less than 2 cm, a double plan is chosen, and if larger than 2 cm a subglandular or subfascial is chosen. The access routes and implant shape are discussed with the patients and decided with them.
Surgical technique - access route
Before surgical marking, an inspection was carried out in the breast, anterior chest and spine in order to identify asymmetries and different heights of breast folds. The sternal midline was evident and a possible detachment area. During anesthetic induction , the antibiotic prophylaxis was done using 2 grams of cefazolin intravenously.
An incision in the mammary fold of 4 cm long with detachment 1 cm below was done to proper accommodate the prosthesis in order to avoid unsightly scars with the use of swimsuits. After detachment as planned in preoperative, the cavity was irrigated with 150 ml of saline soluction. The surgeon exchanges the gloves before proper placing the implant. Subsequently, a three-plane suture is carried out subcutaneous and subdermal with Monocryl 3.0; and intradermal with Monocryl 4.0.
In all cases we used molds to define the volume to be used. Drains were not used. Dressings used were made of micropore and sterile gauze. The patients were under observation with fixed medications, opioids, nonsteroidal anti-inflammatory drugs.
Patients were discharged 12 hours after the procedure, and instructed to take a shower only 48 hours after the surgery. Patients were followed-up every week, the dressing with micropore was maintained to define the preoperative marking for 7 days. The patient was instructed to wear a compression bra for 2 weeks.
Mastopexy associated with breast implant: Marking using A, B and C points. The Schwartzmann maneuver and de-epithelialization were done. A thin lower flap pedicle for prosthesis protection was created. In cases where there is manipulation of the mammary gland, the prosthesis was washed with solution as recommended by Adams et al.14, excepted the use of Bacitracin, which is not be available in the country. The de-epithelialization was carried out before test the molds (Figure 1).
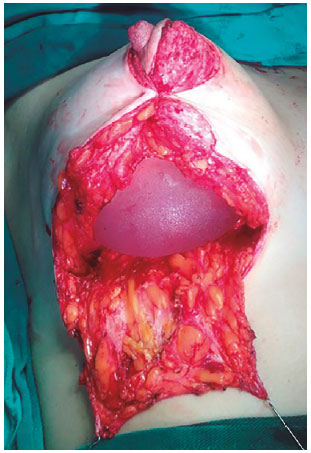
Figure 1. Mastopexy with breast implantation. Inferior pedicle for protection.
Surgical technique - breast implant planning
Breast implant planning was done based on description of the literature.
RESULTS
A retrospective cohort study was carried out based on intention-to-treat approach of 50 women who underwent breast augmentation or mastopexy associated with the implant between 2011 and 2016. Patients were selected based on inclusion and exclusion criteria of previously described treatment. For better analysis, data were classified by breast; a total of 100 breasts. Patients' age ranged from 17 years to 56 years,mean age was 36 years, a standard deviation of 10 years and a median of 36 years.
Only one patient (2%) become pregnant after plastic surgery, but no significant repercussions occurred in results. Of 6% of smokers in our sample, 33% "underwent a surgical reintervention. No rupture or rotation of the breast implant was observed. The mean volume of implants was 270 ml. Isolated mammoplasty was performed in 55% of cases (Figures 2 and 3) and mastopexy associated with implantation in 45% of cases (Figure 4).

Figure 2. Isolated breast augmentation, incision in the mammary sulcus, subglandular plane, round implant, high projection.
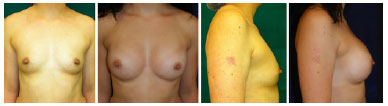
Figure 3. Isolatet breast augmentation, incision in the mammary sulcus, douple plan, round implant, high projection.

Figure 4. Maxtopexy associated with breast implant, inverted T incision, subglandular plan, round implant, high projection.
Patients' mean age who underwent breast augmentation was approximately 35 years, while the mean age of patients who choose to perform mastopexy associated with the implant was 39 years, with a standard deviation of 10 years in both sections.
In all cases of breast augmentation associated with mastopexy the T inverted technique was used. Patients who performed isolated breast implant, in 85% the access was via inframammary, while 15% the access was via inferior areolar. Of nine patients who underwent surgical reintervention, 5 underwent bilateral surgical reintervention (55%) and only four patients underwent unilateral surgery (45%).
When data were stratified by surgery (Figure 5), we observed that 57% of reinterventions were performed in the mastopexy associated with a prosthesis implant. In the breast augmentation group, 11% had reintervention, compared with 18% of the breasts in the mastopexy group associated with implant. Difference was not statistically significant by chi-squared test (p = 0.487).
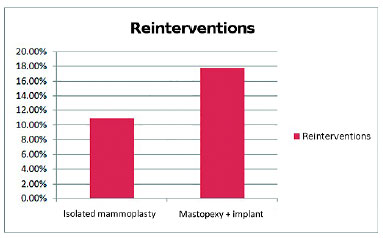
Figure 5. Percentage of reinterventions according to surgery.
Surgical reintervention was carried out in 14% of cases. Causes of reintervention were hematoma in 1% of cases, seroma 4%, asymmetry 4%, bad positioning of the prosthesis in 2% and capsular contracture in 3% breasts. The most prevalent complication was performed in 14% of patients from the implant group and in 9% of patients who underwent mastopexy associated with breast implant.
The association of dissection plan and surgical technique showed that breast augmentation by itself were similar to double plan indications (45%) and subglandular (44%). In the mastopexy associated with implant, the subglandular dissection plane was predominant (71%). Concerning correlation between dissection plane and reintervention rate (Figure 6), the subglandular plane was chosen in 56%, and required surgical reintervention in 14% of cases.
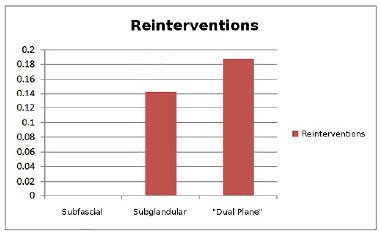
Figure 6. Percentage of reinterventions according dissection plan.
Double plan technique was performed in 32% of cases, and 19% of cases were reoperated. Subfascial plane was performed in 12% of cases and no of them required surgical reintervention. The chi-square test did not show statistical significance in the association between dissection plane and complications.
The analysis of associations between breast implant shape and reintervention rates (Figure 7) indicated the use of rounding prosthesis in 86%, which required surgical reintervention in 16% of cases. In cases with anatomical implants (14%), none required surgical reintervention. There was no statistical significance in the association between breast implant and reinterventions using the chi-square test.
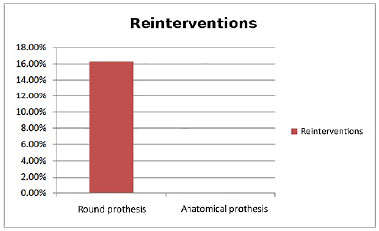
Figure 7. Percentage of complications and reinterventions for each breast according to shape of breast prosthesis.
Correlation between the procedure and the late aesthetic quality of the scar was assessed using a Stony Brook Scar Evaluation Scale, as mentioned above. In the breast group, 14% had grade 2, 25% grade 3, 32% grade 4 and 29% grade 5. In breast group associated with breast implant no patient had grade 1, 16% had grade 2, 30% grade 3, 13 % grade 4 and 40% grade 5 (Figure 8).
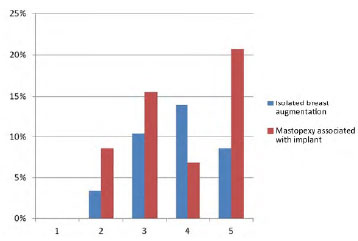
Figure 8. Percentage of breasts in Stony Brook Scar Evaluation Scale according to procedure.
No statistical significance was found in the analysis of the Stony Brook Scar Evaluation Scale in association with procedures, diagnosis, access route, dissection plane, composition, shape and texture of the prosthesis using the chi-square test. No statistical significance was found in the analysis of the Stony Brook Scar Evaluation Scale associated with age, body mass index (BMI), size from breast implant and time (in days) to return to daily life activities and practical life activities by the Kolmogorov-Smirnov and Shapiro-Wilk tests.
DISCUSSION
The study analyzed the effect of the surgical plan on postoperative complications rates and need of surgical reintervention in breast augmentation. It is important to perform the appropriate surgical technique to reduce complications and reoperations in mammoplasty. Complications such as capsular contracture, improper positioning and extrusion are directly related with the technical precision in which the primary procedure is done.
This study was designed to analyze specifically the effect of the surgical plan on postoperative outcome. Based on the experience of the Plastic Surgery Service of the Hospital de Clínicas de Porto Alegre. When implant placement plans were evaluated along with reoperation rates, there were different positions in the literature. Tebbetts15 establishes a pattern of breast augmentation by reporting a 0% reoperation rate in 50 consecutive patients followed by 3 years.
However, other authors did not achieve the same results, Stutman et al.4 obtained a reoperation rate of 18% in the subglandular plan and 14% in double plan.Pereira & Sterodimas16 reported 2% in the subglandular plan, 6% in the double plan and 0% in subfascial. Brown17 described 7.2% in the subglandular and 4% in the subfascial. Montandon18 analyzed 546 patients and described a greater risk of general complications in submuscular (16%) than in subglandular (8%).
In this series of patients in cases that performed subglandular plan, the surgical reintervention rate was 14% and in cases of double plan this rate was 19%. In terms of prosthesis shape used, Tavares-Filho19 proposed an algorithm to define the choice of round or anatomical implant, this algorith describes a higher reoperation rate in anatomical 6.2% than in the round 3.7% implants. However, in this study, the surgical reintervention rate was 16% in the round implants and no case was needed when the anatomical implants were chosen.
Regarding the comparison of access routes and postoperative outcomes, there is also no consensus in the literature. Stutman et al.4 did not found significant difference between the access routes and the outcomes in sample including 612 patients, however, the mammary sulcus presented a greater risk for extrusion, and the surgical reoperation rate was 24% for mammary sulcus and 13% in the periareolar route.
Authors who describe a single access route in their routine reported a lower reoperation rate. Wiener11 reported only 3% of reoperation cases by the mammary sulcus. Han et al.20, however, described 6% of reoperations in patients who underwent mammoplasty augmentation via the infra-areolar approach. Codner et al.2 in a retrospective analysis of 15 years on mastopexy associated with silicone implant founded a reoperation rate of 26%.
Almeida et al.21 in the description of a safety technique to perform mastopexy with implant reported 12% of major complications. Montandon18 reported a higher risk of major complications in breast augmentation associated with mastopexy (16%) than in the isolated implant (7%).
In this series, 11% of isolated breast augmentation cases were surgical reintervation, against 18% of the breasts implant-associated mastopexy group. In the evaluation of results we obtained rates similar to the large series, mainly in the studies of large centers with residency training.
As for the subfascial plane and anatomical shape implants because our sample is small, the validity of the results can be questioned. We obtained less satisfactory results regarding the late outcome of postoperative scar quality, being only 61% grade 4 or 5 in the Stony Brook Scar Evaluation Scale in the isolated breast augmentation and 53% in the breast augmentation associated with mastopexy, which motivated us to review the routine of the service.
There is still no consensus regarding the best access route and plan of breast implant, requiring studies to compare different routines of each service. Currently, the best results are still based on a systematized routine, precise surgical dissection and minimal contamination.
CONCLUSION
We conclude that no significant difference exist between the variation in surgical planning and the incidence of postoperative complications or need of reintervention in surgeries carried out between 2011 and 2016 in Hospital das Clínicas de Porto Alegre.
COLLABORATIONS
JM Analysis and/or interpretation of data; statistical analyses; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
ACPO Analysis and/or interpretation of data; final approval of the manuscript; writing the manuscript or critical review of its contents.
EL Statistical analyses; completion of surgeries and/or experiments.
JB Completion of surgeries and/or experiments.
CPP Analysis and/or interpretation of data; Writing the manuscript or critical review of its contents.
DD Completion of surgeries and/or experiments.
JH Completion of surgeries and/or experiments.
MVMC Final approval of the manuscript; conception and design of the study; writing the manuscript or critical review of its contents.
REFERENCES
1. International Survey on Aesthetic/Cosmetic (ISAPS) [homepage na internet]. Procedures Performed in 2014 [acesso 2016 Jul 5]. Disponível em: http://www.isaps.org/Media/Default/global-statistics/2015 ISAPS Results.pdf
2. Codner MA, Mejia JD, Locke MB, Mahoney A, Thiels C, Nahai FR, et al. A 15 year experience with primary breast augmentation. Plast Reconstr Surg. 2011;127(3):1300-10. PMID: 21364430 DOI: http://dx.doi.org/10.1097/PRS.0b013e318205f41b
3. Hammond DC, Migliori MM, Caplin DA, Garcia ME, Phillips CA. Mentor Contour Profile Gel implants: clinical outcomes at 6 years. Plast Reconstr Surg. 2012;129(6):1381-91. PMID: 22327894
4. Stutman RL, Codner M, Mahoney A, Amei A. Comparison of breast augmentation incisions and common complications. Aesthetic Plast Surg. 2012;36(5):1096-104. PMID: 22653141
5. Somogyi RB, Brown MH. Outcomes in primary breast augmentation: a single surgeon's review of 1539 consecutive cases. Plast Reconstr Surg. 2015;135(1):87-97. PMID: 25539298
6. Murphy DK, Beckstrand M, Sarwer DB. A prospective, multicenter study of psychosocial outcomes after augmentation with natrelle silicone-filled breast implants. Ann Plast Surg. 2009;62(2):118-21. PMID: 19158517
7. Spear SL, Murphy DK, Slicton A, Walker PS; Inamed Silicone Breast Implant U.S. Study Group. Inamed silicone breast implant core study results at 6 years. Plast Reconstr Surg. 2007;120(7 Suppl 1):8S-16S.
8. Sarwer DB. The psychological aspects of cosmetic breast augmentation. Plast Reconstr Surg. 2007;120(7 Suppl.1):110S-117S.
9. Momeni A, Padron NT, Föhn M, Bannasch H, Borges J, Ryu SM, et al. Safety, complications, and satisfaction of patients undergoing submuscular breast augmentation via the inframammary and endoscopic transaxillary approach. Aesthetic Plast Surg. 2005;29(6):558-64. DOI: http://dx.doi.org/10.1007/s00266-005-0095-z
10. Jacobson JM, Gatti ME, Schaffner AD, Hill LM, Spear SL. Effect of incision choice on outcomes in primary breast augmentation. Aesthet Surg J. 2012;32(4):456-62. DOI: http://dx.doi.org/10.1177/1090820X12444267
11. Wiener TC. Relationship of incision choice to capsular contracture. Aesthetic Plast Surg. 2008;32(2):303-6. PMID: 17994260 DOI: http://dx.doi.org/10.1007/s00266-007-9061-2
12. Spear SL, Baker JL Jr. Classification of capsular contracture after prosthetic breast reconstruction. Plast Reconstr Surg. 1995;96(5):1119-23. DOI: http://dx.doi.org/10.1097/00006534-199510000-00018
13. Singer AJ, Arora B, Dagum A, Valentine S, Hollander JE. Development and validation of a novel scar evaluation scale. Plast Reconstr Surg. 2007;120(7):1892-7. DOI: http://dx.doi.org/10.1097/01.prs.0000287275.15511.10
14. Adams WP Jr, Rios JL, Smith SJ. Enhancing patient outcomes in aesthetic and reconstructive breast surgery using triple antibiotic breast irrigation: six-year prospective clinical study. Plast Reconstr Surg. 2006;117(1):30-6. PMID: 16404244
15. Tebbetts JB. Achieving a zero percent reoperation rate at 3 years in a 50-consecutive case augmentation mammaplasty premarket approval study. Plast Reconstr Surg. 2006;118(6):1453-7.
16. Pereira LH, Sterodimas A. Transaxillary breast augmentation: a prospective comparison of subglandular, subfascial, and submuscular implant insertion. Aesthetic Plast Surg. 2009;33(5):752-9. PMID: 19597863 DOI: http://dx.doi.org/10.1007/s00266-009-9389-x
17. Brown T. Subfascial breast augmentation: is there any advantage over the submammary plane? Aesthetic Plast Surg. 2012;36(3):566-9. DOI: http://dx.doi.org/10.1007/s00266-011-9840-7
18. Montandon RE. Estudo de complicações em próteses mamárias: avaliação de 546 casos em oito anos. Rev Bras Cir Plást. 2014;29(3):352-60.
19. Tavares-Filho JM, Franco D, Franco T. Implante mamário redondo versus anatômico: algoritmo para escolha da forma adequada. Rev Bras Cir Plást. 2015;30(3):413-22.
20. Han HH, Kim KK, Lee KH, Park D, Rhie JW, Ahn ST, et al. Transareolar-perinipple (areolar omega) zigzag incision for augmentation mammaplasty. Plast Reconstr Surg. 2015;135(3):517e-725e. DOI: http://dx.doi.org/10.1097/PRS.0000000000000967
21. Almeida ARH, Araújo GKM, Mafra AVC, Pimenta PS, Fabrini HS. Augmentation mastoplasty with silicone implant associated with mastopexy through an initial periareolar approach (safety pocket). Rev Bras Cir Plást. 2012;27(4):569-75. DOI: http://dx.doi.org/10.1590/S1983-51752012000400017
1. Hospital de Clínicas de Porto Alegre, Porto Alegre, RS, Brazil
2. Universidade Federal do Rio Grande do Sul, Porto Alegre, RS, Brazil
3. Universidade de Barcelona, Espanha
Institution: Hospital de Clínicas de Porto Alegre, Universidade Federal do Rio Grande do Sul, Porto Alegre, RS, Brazil.
Corresponding author:
João Maximiliano
Rua Ramiro Barcellos, 2350
Porto Alegre, RS, Brazil - Zip Code 90035-903
E-mail: jmaximilianopm@gmail.com
Article received: November 4, 2016.
Article accepted: July 9, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter