

Original Article - Year 2017 - Volume 32 -
Use of the back-folded dermaglandular inferior pedicle in mammary amputation: improving results
Uso do pedículo inferior não areolado na amputação mamária: aprimorando resultados
ABSTRACT
INTRODUCTION: Patients with gigantomastia have multiple physical and psychosocial symptoms. Various techniques have been proposed for their treatment. Described by Torek in 1922, mammary amputation was presented as a great alternative, but resulted in reduced mammillary functionality and loss of breast format. In 1975, Liacyr Ribeiro described the use of dermaglandular inferior pedicle as safety tissue to allow for mammary resection, to facilitate breast assembly and to improve projection. The author proposed to unite these two consolidated techniques with the intention of improving breast amputation outcomes.
METHODS: Eleven gigantomastia patients were operated on by means of the amputation technique using dermaglandular inferior pedicle.
RESULTS: The mean distance between the sternal notch and the nipple was 35.6 cm for the right breast and 35 cm for the left breast, with all measures ranging between 30 cm and 44 cm. Rise of the nipple-areola complex was in average 16.9 cm for the right breast and 16.4 cm for the left breast, varying from 12 to 25 cm. The amount of breast tissue resection per patient was, in average, 3559.5 grams, ranging from 1600 grams to 5890 grams. Hypopigmentation of the nipple-areola complex was present in three patients (27%). Dehiscence of the T was observed in two patients (18%). Partial non-integration of the graft occurred in three patients (27%), with loses estimated at 10%, 30% and 80% of the graft.
CONCLUSION: Associating mammary amputation with an inferior dermaglandular pedicle provides good remodeling and safe assembling of the breast, in addition to providing proper projection.
Keywords: Breast/abnormalities; Mammaplasty; Hyperthophy; Amputation.
RESUMO
INTRODUÇÃO: Pacientes com gigantomastia apresentam múltiplos sintomas físicos e psicossociais. Várias técnicas foram propostas para o seu tratamento. A amputação mamária, descrita por Torek em 1922, apresenta com excelente alternativa, porém com prejuízo na funcionalidade mamilar e no formato da mama. Liacyr Ribeiro, em 1975, descreveu o retalho inferior dermoglandular não areolado a fim de proporcionar tecido de segurança para ressecção mamária, facilitar a montagem da mama e melhorar sua projeção. Este trabalho propôs unir estas duas consagradas técnicas, visando aprimorar os resultados das amputações mamárias.
MÉTODOS: Foram operadas 11 pacientes com gigantomastia com prole definida, pela técnica de amputação mamária associada ao pedículo inferior não areolado.
RESULTADOS: Distância média da fúrcula esternal ao mamilo foi de 35,6 centímetros na mama direita e 35 centímetros na mama esquerda, variando de 30 a 44 centímetros. A ascensão do complexo areolomamilar foi em média de 16,9 centímetros na mama direita e 16,4 centímetros na mama esquerda, variando de 12 a 25 centímetros. A quantidade de ressecção média de tecido mamário por paciente foi de 3559,5 gramas, variando de 1600 a 5890 gramas. A hipopigmentação do complexo areolamamilar esteve presente em três (27%) pacientes. A deiscência do T foi observada em dois (18%) pacientes. A não integração parcial do enxerto ocorreu em três (27%) das pacientes, com perdas estimadas de 10%, 30% e 80% do enxerto.
CONCLUSÃO: A associação da amputação mamária com o pedículo dermoglandular inferior não areolado nos oferece um melhor remodelamento da mama, segurança na montagem desta, além de proporcionar uma adequada projeção da mesma.
Palavras-chave: Mama/anormalidades; Mamoplastia; Hipertrofia; Amputação.
Mammary hypertrophy is a disorder defined by hyper development of the mammary tissue. When habitual volume is excessive, it is called gigantomastia. There is no consensus around a proper definition for it, but the most commonly used one is when there is an excess of 1.5 kg of the tissue. This disorder causes various physical and psychosocial symptoms, which include mastalgia, pain and skin lesions in the bra supporting area, sub mammary infection caused by fungus or dermatitis, postural disorders, cervical pain, dorsal pain, in addition to damage by chronic traction of the 4th, 5th and 6th intercostal nerves1-5.
Various surgical techniques have been described with the main purpose of relieving the symptoms with reduced mammary volume, in addition to the aesthetic aspect of the result. Several papers mention Duncan6,7 as initiator, in 1669, of the first resection to treat gigantomastia. The first surgical report of an aesthetic breast reduction by hypertrophy is found in Dieffenbach's book in 18488.
One of the most relevant techniques to treat the great hypertrophies is mammary amputation with areolar graft, described with aesthetic purposes by Torek in 1922. It is a simple and effective technique that leads to great breast volume reduction and improvement of breast weight related symptoms. In contrast with its efficacy, it presents insufficient breast and areolar complex projection1,4,9-15.
In 1975, Liacyr Ribeiro described the non-areolar dermaglandular inferiorly pedicled flap, called pedicle number 1. This pedicle became an important alternative in breast surgery, offering its dermaglandular content to fill the upper pole of the breast, typically empty in patients with breast ptosis. In addition to shaping the upper pole. More than just shape to the upper pole, this flap appears as safety tissue in breast resections, reducing the bottoming out characteristic and providing more harmonious long lasting breast projection results16-18.
OBJECTIVE
This paper is intended to describe the use of the inferior pedicle in mammary amputation as a contribution to enhancing results.
METHODS
This study included female patients submitted to dermaglandular inferior pedicle mammary amputation surgeries between February 2015 and September 2016. All patients signed the Term of Free and Informed Consent, and the Helsinki principles were followed.
We selected 11 patients with the diagnosis of gigantomastia, who used 50+ bra sizes and had more than 30 cm between the sternal notch and the nipple, with mammary tissue resection estimated at more than 1,500g and defined offspring (either submitted to a definitive contraceptive method or being of advanced age), as well as patients with previous breast surgery that made impossible to use a vascular areolar flap.
The 11 patients subjected to surgery were in average 44.2 years old (26 to 58 years), and all of them had completed childbearing. Two of the patients had comorbidities, one of whom had thyroidopathy and the other one had arterial hypertension, both of which were controlled. Average surgical time was 3 hours and 27 minutes. The surgeries were performed at the General Edson Ramalho Military Police Hospital, in João Pessoa, PB, Brazil.
Surgical Technique
Patient marking was performed in orthostatic position. Point A was marked as projection of the inframammary fold. Points B and C were marked by means of a bi-digital maneuver pinch test between the lateral and medial borders of the nipple-areolar complex. AB and AC distances were both 10 cm. Marking of the inferior pedicle was performed in the following proportions: 10 cm base, 10 cm length, and 5 cm thickness (Figure 1).
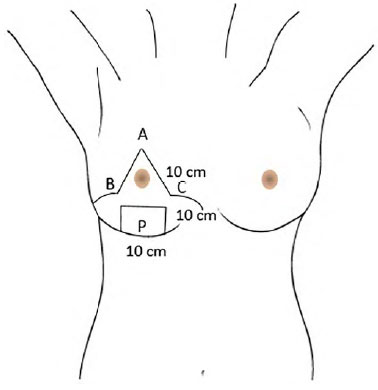
Figure 1. Pre-operative marking. A: Inframammary line projection; B and C: Points for vertical bi-digital pinching on the medial and lateral edges of the nipple-areola complex; P: Inferior dermaglandular flap.
After the epidural anesthesia, an aseptic and antiseptic technique was performed and sterile drapes were positioned. Breasts were infiltrated with a 0.9% saline solution and adrenaline in the proportion of 1:250.000. Resection was initiated by the areola as a thin graft, previously marked with a 3.5 areolar marker.
An incision was made from the upper marking to the pectoralis major fascia. A resection of the medial and lateral portions of the breast was performed to make the inferior dermaglandular flap. Mammary amputation was performed with a block resection of the mammary tissue (Figure 2). Liacyr's number 1 pedicle (Figure 3) was fixed to the fascia of the pectoralis major muscle with mononylon 2-0 suture at 5 points.

Figure 2. En bloc mammary amputation

Figure 3. Inferior dermaglandular flap (Liacyr Ribeiro's Pedicle 1).
The breast was sutured with mononylon 3-0 and monocryl 4-0, and the areola graft was stitched with simple MN-4-0 suture at the cardinal points and an MN-5-0 continuous suture. The 4-0 sutures were used as a Brown dressing (Figure 4). Drains were not used. The patient was maintained under prophylactic antibiotic therapy and routine pain medication. Hospital discharge was possible on post-op day 1. The patient was kept on weekly follow-up, and the Brown dressing was removed on post-op day 7.
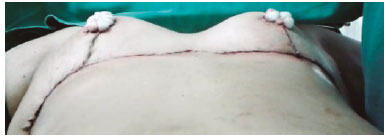
Figure 4. Final aspect with Brown dressing.
RESULTS
The average distance between the sternal notch and the nipple was 35.6 cm on the right breast and 35cm on the left breast, varying from 30 to 44cm (Figure 5). Rise of the nipple-areolar complex to its desired position was 16.9 cm on the right breast and 16.4 on the left breast, varying from 12 to 25 cm (Figure 6). The average weight of resected mammary tissue was 3559.5g per patient, varying from 1600g to 5890g (Figure 7).
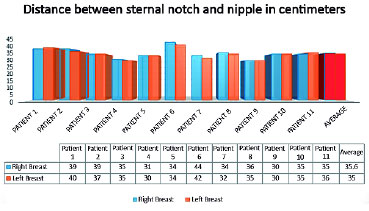
Figure 5. Distance between sternal notch and nipple, in centimeters.
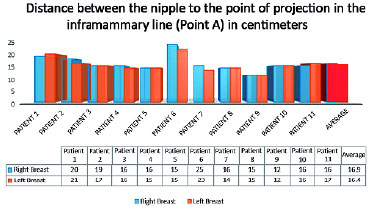
Figure 6. Distance between the nipple to the point of projection in the inframammary line (Point A), in centimeters.
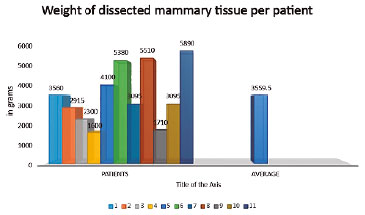
Figure 7. Weight of dissected mammary tissue per patient, in grams.
Post-op follow-up was scheduled for weeks 1, 2, 4, 12, 24, 48, and 72 (Figures 8 to 11).

Figure 8. Above: Pre-operative. Below: Post-operative at 18 months.

Figure 9. Above: Pre-operative. Below: Post-operative at 6 months.

Figure 10. Above: Pre-operative. Below: Post-operative at 8 months.

Figure 11. Above: Pre-operative. Below: Post-operative at 6 months.
The most common complication observed was hypopigmentation of the nipple-areolar complex in three (27%) of the patients. Dehiscence of the T was observed in two (18%) of the patients. Non-integration of the graft was observed in three (27%) of the patients, with losses estimated at 10%, 30% and 80% of the areolar graft. There were no cases of total loss of the areolar graft.
All patients reported high levels of aesthetic satisfaction and great improvements to their excessive breast weight related symptoms.
DISCUSSION
Gigantomastia patients have multiple signs and symptoms related to excessive breast weight. The main objective of the reductive breast surgery in these cases is to improve the conditions leading to these complaints. In this study, patients related great overall symptom relief, specially pain complaints, and aesthetic and QoL improvements.
Mammary amputation is a simple, fast and effective technique for the treatment of gigantomastia. It is indicated for patients who have excessive breasts volumes and present important complaints related to the breast volume, as well as patients with high risk of necrosis of the nipple-areola complex, with great distance between the sternal notch and the nipple-areola complex, and comorbidities that change breast vascularization as well as any previous surgery that hinders the use of an areolar vascular flap1-4,9,16.
McKissock suggests use of mammary amputation when more than 1 kg of breast tissue is going to be resected per breast and when the vertical distance of the pedicle is greater than 35 cm19,20. On the other hand, in addition to breast feeding and nipple sensitivity losses, this technique also presents poor aesthetic results due to slight breast projection10,12-15.
To promote greater projection and best breast remodeling with this technique, the authors used the inferior pedicle described by Liacyr Ribeiro in 1975. This alternative has become very important in breast surgeries, as it offers dermaglandular volume to fill the upper pole of the breast, which is typically empty in patients with breast ptosis and major hypertrophies.
In addition to upper breast contour reshaping, the flap presents a safe tissue alternative in breast resections and reduces the bottoming-out effect with more harmonious and long lasting results16-18.
In gigantomastia patients, the excessive breast tissue is disproportionally distributed across the breast. There is minimum tissue in the upper pole and a large volume below the inframammary fold, due to the high degree of ptosis and to breast weight (Figure 12). This observation led the author to associate the two consolidated breast surgery techniques, namely mammary amputation and use of the inferior pedicle.
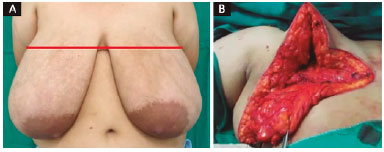
Figure 12. Unequal distribution of the mammary tissue across gigantomastias. A: We observe tissue predominance in the region below the inframammary line (red line); B: Intraoperative showing tissue scarcity in the upper breast pole.
We have thus sought, in amputation, to make an easier resection of the large amount of breast tissue and to provide a more versatile way to ascend the nipple-areolar complex, and, in the inferior pedicle, to offer more tissue for the upper pole, thus improving breast tissue reshaping and overall projection and affording more safety to tissue resection (Figure 13).

Figure 13. Difference in breast projections. Right breast using the dermaglandular flap for assembly. Yellow arrow shows Liacyr's Type 1 Pedicle not used for breast assembly.
CONCLUSION
For gigantomastia patients submitted to mammary amputation, the dermaglandular flap offers better breast reshaping, safety and assembling, in addition to improving overall breast projection.
COLLABORATIONS
WMM Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
SAPJ Analysis and/or interpretation of data; final approval of the manuscript; writing the manuscript or critical review of its contents.
DSFM Completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
REFERENCES
1. Thorek M. Possibilities in the reconstruction of the human form 1922. Aesthetic Plast Surg. 1989;13(1):55-8. PMID: 2658498 DOI: http://dx.doi.org/10.1007/BF01570326
2. Rees TD. An historical review of mammaplasty. Annals of Transact Fifth Intern Cong Plast S; Australia.
3. Thorek M. Plastic reconstruction of the breast and free transplantation of the nipple. J Int Coll Surg. 1946;9:124-24.
4. Pitanguy I, Degand M, Pelle Ceravollo M. et al. Estudo crítico e evolução da técnica de Pitanguy para redução mamária baseados num estudo de 1903 casos. Rev Bras Cir. 1979;69(11-12):357-76.
5. Glatt BS, Sarwer DB, O'Hara DE, Hamori C, Bucky LP, LaRossa D. A retrospective study of changes in physical symptoms and body image after reduction mammaplasty. Plast Reconstr Surg. 1999;103(1):76-82. DOI: http://dx.doi.org/10.1097/00006534-199901000-00013
6. Ferreira LM, Castilho HT, Duarte IS, Andrews JM. Cirurgia estética. In: Ferreira LM, ed. Manual de Cirurgia Plástica. São Paulo: Atheneu; 1995. p. 287-91.
7. Avelar JM, Gameiro CA. Nuevos conceptos en la mastoplastia. In: Avelar JM, Malbec EF, eds. Historia, ciência y arte en cirurgia estética. São Paulo: Editora Hipócrates; 1990. P. P.550-9.
8. Pitanguy I. Mamoplastias: estudo de 245 casos consecutivos e apresentação de técnica pessoal. Rev Bras Cir. 1961;42(4):201-20.
9. Pitanguy I. Contribuição à técnica do enxerto livre para correção das grandes hipertrofias mamárias. Plast. VII. 1963;2:75.
10. Hinderer UT. Plastias mamarias de reducción. Principios básicos. Tecnicas personales. In: Coiffman F, ed. Cirurgia plástica, reconstructiva y estética. 2ª ed. Barcelona: Nasson-Salvat; 1994. p. 3350-85.
11. Koger KE, Sunde D, Press BH, Hovey LM. Reduction mammaplasty for gigantomastia using inferiorly based pedicle and free nipple transplantation. Ann Plast Surg. 1994;33(5):561-4. PMID: 7857054 DOI: http://dx.doi.org/10.1097/00000637-199411000-00017
12. Misirlioglu A, Akoz T. Familial severe gigantomastia and reduction with the free nipple graft vertical mammoplasty technique: report of two cases. Aesthetic Plast Surg. 2005;29(3):205-9. DOI: http://dx.doi.org/10.1007/s00266-004-0134-1
13. Isken T, Sen C, Onyedi M, Izmirli H. A new application for increasing breast projection in free-nipple-graft reduction mammaplasty. Aesthetic Plast Surg. 2008;32(4):675-80. PMID: 18506509 DOI: http://dx.doi.org/10.1007/s00266-008-9185-z
14. Gorgu M, Ayhan M, Aytug Z, Aksungur E, Demirdover C. Maximizing breast projection with combined free nipple graft reduction mammaplasty and back-folded dermaglandular inferior pedicle. Breast J. 2007;13(3):226-32. DOI: http://dx.doi.org/10.1111/j.1524-4741.2007.00414.x
15. Casas LA, Byun MY, Depoli PA. Maximizing breast projection after free-nipple-graft reduction mammaplasty. Plast Reconstr Surg. 2001;107(4):955-60. DOI: http://dx.doi.org/10.1097/00006534-200104010-00008
16. Ribeiro L. Cirurgia Plástica da Mama. Rio de Janeiro: Medsi; 1989.
17. Ribeiro L. A new technique for reduction mammaplasty. Plast Reconstr Surg 1975;55(3):330-4. DOI: http://dx.doi.org/10.1097/00006534-197555030-00010
18. Ribeiro L, Accorsi A Jr, Buss A, Marcal-Pessoa M. Creation and evolution of 30 years of the inferior pedicle in reduction mammaplasties. Plast Reconstr Surg. 2002;110(3):960-70. PMID: 12172167 DOI: http://dx.doi.org/10.1097/00006534-200209010-00038
19. McKissock P. Color Atlas of Mammaplasty. New York: Thieme Medical Publishers; 1991. p. 47-78.
20. McKissock PK. Reduction mammaplasty with a vertical dermal flap. Plast Reconstr Surg. 1972;49(3):245-52. PMID: 4551235 DOI: http://dx.doi.org/10.1097/00006534-197203000-00001
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Hospital Militar General Edson Ramalho, João Pessoa, PB, Brazil
Institution: Hospital Militar General Edson Ramalho, João Pessoa, PB, Brazil.
Corresponding author:
Wellerson Marcos Mattioli
Rua Eugênio Lucena Neiva, SN - Tambiá
João Pessoa, PB, Brazil - Zip Code 58020-782
E-mail: wmmattioli@gmail.com
Article received: November 24, 2016.
Article accepted: July 9, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter