

Original Article - Year 2017 - Volume 32 -
Surgical treatment of bromhidrosis
Tratamento cirúrgico da bromidrose
ABSTRACT
INTRODUCTION: Bromhidrosis or osmidrosis causes many patients to seek specialized medical treatment. Removal of the sweat glands from the axillary region through excision and complementary liposuction is a minor, technically simple procedure, with few complications. The objective of this study is to review the role of surgery in bromhidrosis, complications of treatment, and the degree of patient satisfaction.
METHOD: Thirty-two patients underwent liposuction and removal of axillary tissue under local anesthesia and sedation. The patients were followed up for at least 6 months postoperatively, to evaluate the outcome and possible complications. The Client Satisfaction Questionnaire was completed after 6 months.
RESULTS: After 6 months of follow-up, there were few complications and the questionnaire revealed a high degree of satisfaction.
CONCLUSION: In addition to being easily performed, the procedure was safe, with few complications.
Keywords: Sweat gland diseases; Treatment; Reconstructive surgical procedures; Sweat glands; Sweat.
RESUMO
INTRODUÇÃO: A bromidrose ou osmidrose é um problema que leva inúmeros pacientes a procurar tratamento médico especializado. A remoção das glândulas sudoríparas da região axilar por meio de exérese e lipoaspiração complementar é um procedimento de pequeno porte, tecnicamente simples e com poucas complicações. O objetivo deste trabalho é mostrar a aplicação da cirurgia neste problema, suas complicações e o grau de satisfação dos pacientes.
MÉTODO: Trinta e dois pacientes foram submetidos à lipoaspiração e retirada dos tecidos da axila, sob anestesia local e sedação. Acompanhou-se por no mínimo 6 meses estes pacientes no pós-operatório, avaliando a evolução e possíveis complicações e aplicou-se o questionário CSQ-8 para o grau de satisfação no sexto mês.
RESULTADOS: Após 6 meses de acompanhamento, poucas foram as complicações e as respostas ao questionário demonstraram alto grau de satisfação.
CONCLUSÃO: Além de ser facilmente exequível, o procedimento se mostrou seguro e com poucas complicações.
Palavras-chave: Doenças das glândulas sudoríparas; Tratamento; Procedimentos cirúrgicos reconstrutivos; Glândulas sudoríparas; Suor.
Bromhidrosis, also known as osmidrosis, is the presence of strong and unpleasant body odor, despite proper hygiene. It is largely due to secretion by the apocrine glands, but may also be caused by metabolic diseases, food, drugs, or toxic materials, and is also associated with hyperhidrosis1. Bacteria and debris release volatile components with unpleasant odors, and decomposition products are also contributory. Bromhidrosis is a health problem that affects personal life, work, and interpersonal relationships2.
Human secretory glands are divided into two types: eccrine and apocrine. The eccrine glands are distributed over the surface of the body and are involved in thermoregulation by producing sweat. The apocrine glands release secretions into hair follicles, and have a distribution limited to the axilla, anogenital region, and breasts. They do not participate in thermoregulation and are responsible for the characteristic odor of pheromones. They are located deep in the dermis or upper region of the hypodermis.
Like the sebaceous glands, the odoriferous (apocrine) sweat glands are stimulated by sex hormones and become functional at puberty. The secretion contains proteins, carbohydrates, lipids, and ammonia, as well as pheromones, which are involved in sexual attraction. Initially odorless, it acquires an acrid or musky odor in response to bacterial decomposition3.
In a healthy adult, the axillary apocrine glands are the greatest contributors to body odor. Apocrine secretions are sterile and odorless when they reach the surface of the body. However, bacteria begin to degrade the secretions, yielding fatty acids and ammonia as the odiferous products of decomposition. It is believed that odor is associated with growth of bacterial species, possibly Corynebacterium4.
Excessive eccrine secretion may favor apocrine production and contribute to bromhidrosis. In certain circumstances, odorless eccrine secretion becomes unpleasant, usually occurring after eating certain foods, such as garlic, onions, spices, alcohol, or certain medications. Other theories postulate that eccrine secretion softens keratin, allowing some bacteria to degrade proteins and produce unpleasant odors1.
The use of deodorants and antiperspirants to control odor produced by the apocrine glands has an estimated cost of 400 million dollars annually in the USA. There are no data on the prevalence of bromhidrosis in the general population. Although it affects individuals of all ethnicities, it is believed to be more common in dark-skinned individuals (Africans have larger apocrine glands). There is male predominance, reflecting the existence of more active apocrine glands. Bromhidrosis with apocrine predominance appears after puberty. In contrast, eccrine bromhidrosis predominates in childhood1.
Physical examination of individuals with axillary (apocrine) bromhidrosis is usually normal. However, since eccrine bromhidrosis is caused by bacterial degradation of macerated keratin materials, a thick layer of moist keratin may be found on occasion5. Some diseases may be associated with hyperhidrosis or bacterial overgrowth (obesity, diabetes mellitus, hidradenitis suppurativa).
The differential diagnosis of bromhidrosis should consider associated disorders such as organic brain lesions (olfactory hallucinations may be related to neurological diseases) and psychiatric disorders (paranoid disorders, schizophrenia, phobias, and dysmorphic disorders)1.
Management involves treating the underlying pathogenic mechanism.
Hygienic measures - Patients are advised to maintain proper hygiene, based on the use of antibacterial soaps and antiperspirants, by decreasing the bacterial flora of the skin. Underarm hygiene can be maintained during the day using alcohol wipes. Contrary to belief, antiperspirants with aluminum, zirconium, or zinc salts have not shown this action in the apocrine glands, but are effective in the eccrine glands. In a patient with hyperhidrosis, it is vital to keep the skin dry. Treatments that decrease local moisture may be beneficial for both apocrine and eccrine bromhidrosis.
Dietary treatment - Avoiding certain foods and beverages (garlic, spices, alcohol) that may be contributing factors can improve this clinical condition.
Medical treatment - Before starting specific therapies for bromhidrosis, the existence of a treatable underlying organic disorder should be ruled out. Topical antibiotics that act to control the growth of bacteria are an important therapy with rewarding results1.
Surgical treatment for bromhidrosis is limited because of the risks of morbidity inherent in these procedures. Surgery aims to reduce secretions and the number of apocrine glands by aspiration and/or direct removal. Current techniques include aspiration of glandular content, complete excision of tissue, or a combination of both; liposuction is only complement to excision, since it cannot treat the entire area affected by bromhidrosis. These procedures are associated with the following complications: skin necrosis, dehiscence, hematoma, and keloid formation.
Superficial liposuction is a less traumatic technique, and is performed under local anesthesia with minimal incisions. According to the literature, the relapse rate is approximately 40% when used alone, and achieves more than 90% success when used to complement tissue excision6,7. Skin and subcutaneous excision removes all tissue in order to eliminate skin and cellular attachments. However, it is more invasive, cannot treat the entire affected region, and is often complemented by liposuction7.
OBJECTIVE
The aim of this study was to evaluate the use of bromhidrosis surgery, its risks and complications, and the degree of patient satisfaction with the combined technique of liposuction and excision of subcutaneous tissue. All patients were followed up for at least 6 months and completed a validated Client Satisfaction Questionnaire (CSQ-8).
METHOD
A retrospective observational study was performed between February 2011 and October 2014 at the Ruben Berta Hospital, São Paulo, SP, Brazil, with patients of both sexes undergoing combined liposuction and excision of axillary sweat glands.
All patients signed an informed consent form approved by the Ruben Berta Hospital, and consented to participate in data collection for scientific work.
The inclusion criteria for bromhidrosis surgery were failure of nonsurgical treatment and clinical confirmation of bromhidrosis.
The treatment was explained to the patients, and all possible complications of the surgical procedure, such as extensive and unaesthetic scarring, hardening of the region, hematoma, infection, and local paresthesia were discussed, in addition to possible failure of surgical treatment.
The CSQ-8 (translated into Portuguese to subjectively assess the degree of patient satisfaction8) was applied in the late postoperative period, after a minimum of 6 months.
The CSQ-8 is a closed-ended questionnaire, with responses scored from 1-4, and a total score of 8-32. We also asked if "there was improvement in quality of life after surgery," with possible responses of (1): definitely not, (2): no, I do not think so, (3): yes, I think so, and (4): yes, definitely; this produced an additional score from 1 to 4.
Any complications noted by the examiner/surgeon, such as hematoma, infection, unaesthetic scarring, and movement limitation were also assessed.
Operative technique
Before surgery, the patient was marked after use of the starch-iodine staining test (Minor test). Iodine was applied to the axillae, followed by corn starch, with increased color development in the presence of a higher concentration of glands. Starch in contact with iodine and water from sweating appears purple, thus delimiting the region with excess sweat and the area to be lipoaspirated and resected (Figure 1).

Figure 1. Minor test (starch-iodine).
The procedures were performed with an anesthetist's supervision, under tumescent local anesthesia with sedation, and the patient was discharged after 12 hours of observation. A 0.9% physiological solution was prepared, with an epinephrine concentration of 1:500,000 in 500 ml and addition of 20 ml of 2% lidocaine. Each axilla was infiltrated with 100-150 ml. A 0.5-cm incision was made in the anterior axillary pillar, with a second 0.5-cm incision at the middle third of the medial upper the arm.
Straight, multi-perforated 15 cm × 4 mm cannulas were used. The subcutaneous tissue was aspirated with the 4-mm cannula, always following the demarcation shown by the test and not lipoaspirating the area to be removed in the flap. Deep aspiration requires caution to avoid injuring key structures, such as the brachial plexus, lymph nodes, and vessels.
After superficial liposuction, the demarcated region was incised, and the skin and subcutaneous tissue of the axillae was removed in strips or in a star shape (Figure 2), followed by suturing with subcutaneous 4-0 monofilament nylon and skin closure with 4-0 Monocryl.

Figure 2. Resection of skin and subcutaneous tissue.
Compression dressings were removed after 3 to 5 days in a doctor's office. No drains were placed (Figures 3 to 5).
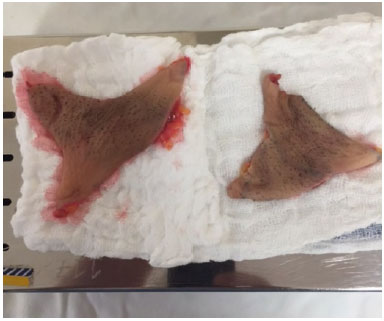
Figure 3. Excised tissue.

Figure 4. Final appearance after skin closure.

Figure 5. Major complication of skin dehiscence.
Antibiotics and analgesics were prescribed, and patients were instructed in postoperative care. Follow-up was performed at 3-5, 21, 60, and 180 days; the CSQ-8 was completed at 6 months8.
Statistical analysis
Data from analysis of the questionnaire were shown as absolute and relative frequencies. Numerical variables were expressed as mean, standard deviation, and 95% confidence interval (CI). The association between categorical variables was analyzed using Fisher's exact test, and p values less than 0.05 were considered significant.
RESULTS
Medical records of 32 patients who underwent combined liposuction and en bloc excision of axillary tissue were analyzed. Of these, 20 (62.5%) were females and 12 (37.5%) were males. The mean age was 29 years, with a standard deviation of 6.1 (range: 18-42 years; 95% CI: 26.8-31.2).
Postoperative complications occurred in 31.3% (n = 10), with ecchymosis in 60%, keloid formation in 30%, and wound dehiscence in 10%. However, none of the patients reported recurrence of sweating and odor.
The CSQ-8 verified satisfaction with the results of combined liposuction and en bloc excision of axillary tissue at least 6 months after the procedure. The results showed a high degree of satisfaction, with a mean CSQ-8 score of 31.8, and a standard deviation of 0.54 (median of 32 and maximum of 32).
Figure 6 shows the overall satisfaction among patients with a postoperative complication. The CSQ-8 scores in patients without complications showed that 100% were definitely satisfied; patients with some postoperative adverse event had a lower score, but over 90% still reported satisfaction (CSQ-8 score above 30).
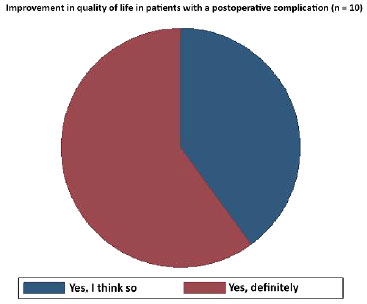
Figure 6. Improvement in quality of life in patients with complications.
Among the 10 patients with complications, 4 had a CSQ-8 score less than 32; of 3 patients with keloid scarring, 1 had a score of 30 and 2 had a score of 31, and 1 patient with wound dehiscence had a score of 30. The presence of dehiscence suggests a possible association with client satisfaction (Fisher's p = 0.063), despite the small sample size.
We observed that 100% of the study sample described the service received as excellent. Only 1 patient (3.2%) reported less than complete satisfaction; however, 96.8% indicated that they had definitely received the care they expected.
Almost all patients (93.7%, n = 30) indicated their needs were met by the care given, and 6.3% (n = 2) said most of their needs were met. All patients reported that the treatment was effective, with 96.9% describing treatment as very effective, and only 3.1% (n = 1) describing treatment as slightly effective.
All patients said they would recommend the service to friends and/or colleagues and would definitely return if needed.
Of the 32 patients, 28 (87.5%) said their quality of life was definitely better, and 4 (12.5%) said it was probably better (Figure 7).
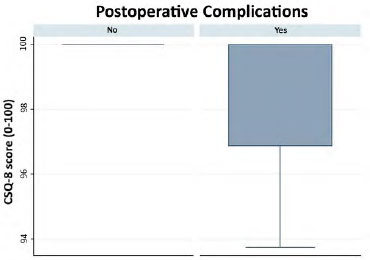
Figure 7. Frequency distribution of improvement in quality of life (4 - Yes, definitely: 60%; 3 - Yes, I think so: 40%) among patients with postoperative complications (ecchymosis, keloids, and dehiscence) (n = 10).
The presence of complications was statistically associated with a lower degree of satisfaction, which is relevant to the quality of life (Fisher's p = 0.006). The 4 patients who reported an effect on improvement in the quality of life had keloids (75%) or dehiscence (25%) (Figure 6).
The 6 patients who developed postoperative bruising were treated conservatively with topical agents and lymphatic drainage, and all improved within 15 days. Three patients developed axillary keloids, and were treated with intralesional 2% triamcinolone, with partial improvement and patient satisfaction.
The most serious complication was a small dehiscence in 1 patient, which responded to local dressing application, without need for surgery. No cases had limitation of movement or infection.
No patient reported recurrence of unpleasant odor, and all were very satisfied with the outcome.
In short, we verified that the procedure was effective in improving the quality of life, and was even effective for those with keloid development and postoperative wound dehiscence. The sample showed high satisfaction, and 100% described the service received as excellent.
DISCUSSION
The choice of treatment for bromhidrosis depends on a discussion between the surgeon and patient, because less invasive techniques leave smaller scars , but there is a greater chance of recurrence; a more aggressive technique combining liposuction with excision has a risk of unaesthetic scarring, but the rate of recurrence is lower.
According to Lee et al.3, surgical treatment for bromhidrosis is well accepted by patients, and improves the quality of life in those who have failed various nonsurgical treatments; these patients have often withdrawn from their social circle and work, with associated psychological consequences.
As demonstrated in the present study, the ideal patient for treatment with liposuction and excision of axillary tissue has had previous unsuccessful nonsurgical treatment, and is often unable to perform routine activities7.
Resolution of axillary bromhidrosis requires removal and destruction of apocrine axillary glands, and only surgical treatment will destroy this tissue.
A desirable outcome requires a minimal axillary scar, rapid healing, few complications, a short period of convalescence, and a low relapse rate, i.e., a merger of aesthetics and functionality.
We believe that the combined treatment of liposuction and en bloc resection of skin and subcutaneous tissue achieved all goals, with few complications and a high degree of satisfaction.
To minimize the area to be resected, we perform a starch-iodine test, which stains the region with the highest concentration of sweat glands.
This is a technique that plastic surgeons can easily perform; the surgery yields great satisfaction with few complications, and improves the quality of life.
CONCLUSION
The surgical treatment of bromhidrosis is feasible, with a low rate of complications, a high degree of patient satisfaction, and good outcomes when performed by trained plastic surgeons.
Further studies on the pathogenesis and prevalence of this disorder are needed. We will continue to follow-up with our patients, to evaluate improvement using our technique.
COLLABORATIONS
AK Final approval of the manuscript.
REFERENCES
1. Cruz Arnés M, Saá Requejo CM, Calvo Cebrián A, Henares García P, Hernández Álvarez LF, García Gutiérrez G. Bromhidrosis. Med Gen. 2005;77:591-5.
2. Dornelas MT, Machado DC, Gonçalves ALCP, Mauês GL, Correa MPD. Tratamento da hiperidrose axillar com lipoaspiração. Rev Bras Cir Plást. 2008;23(3):145-48.
3. Lee D, Cho SH, Kim YC, Park JH, Lee SS, Park SW. Tumescent liposuction with dermal curettage for treatment of axillary osmidrosis and hyperhidrosis. Dermatol Surg. 2006;32(4):505-11.
4. Park YJ, Shin MS. What is the best method for treating osmidrosis? Ann Plast Surg. 2001;47(3):303-9. PMID: 11562036 DOI: http://dx.doi.org/10.1097/00000637-200109000-00014
5. Fiorelli RKA, Elliot GL, Alvarenga RMP, Morard MRS, Almeida CR, Fiorelli SKA, et al. Avaliação do Impacto na Qualidade de Vida de Pacientes Portadores de Hiperidrose Primária Submetidos à Simpatectomia Videotoracoscópica. Meta Aval. 2011;3(7):1-24.
6. Bechara FG, Sand M, Sand D, Altmeyer P, Hoffmann K. Surgical treatment of axillary hyperhidrosis: a study comparing liposuction cannulas with a suction-curettage cannula. Ann Plast Surg. 2006;56(6):654-7. PMID: 16721080 DOI: http://dx.doi.org/10.1097/01.sap.0000205771.40918.b3
7. Gontijo GT, Gualberto GV, Madureira NAB. Atualização no tratamento de hiperidrose axillar. Surg Cosmet Dermatol. 2011;3(2):147-51.
8. Larsen DL, Attkisson CC, Hargreaves WA, Nguyen TD. Assessment of client/patient satisfaction: development of a general scale. Eval Program Plann. 1979;2(3):197-207. DOI: http://dx.doi.org/10.1016/0149-7189(79)90094-6
Secretaria de Justiça e Cidadania de São Paulo, São Paulo, SP, Brazil
Institution: Hospital Ruben Berta, São Paulo, SP, Brazil.
Corresponding author:
Alexandre Kataoka
Av. Paulista, 2494 cj 14
São Paulo, SP, Brazil - Zip Code 01310-300
E-mail: email@domain_name_here.com
Article received: April 14, 2016.
Article accepted: June 6, 2016.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter