

Articles - Year 2003 - Volume 18 -
Use of Bleomycin Sulfate in Treatment of Keloidal Scars
O Uso do Sulfato de Bleomicina no Tratamento de Cicatrizes Queloidianas
ABSTRACT
Keloidal scars may be clinically and/or surgically treated; howeven drugs or surqical procedures do not prevent or cure these scars. The author used intralesional injections of bleomycin as a new treatment. The histopathological examination peiformed before and after infiltrations demonstrates the beneficial effect of bleomycin, confirmed by the clinical progression of the lesions. The study was carried out with 15 patients treated at the Plastic Surgery Service of Clementino Fraga Filho Teaching Hospital - Universidade Federal do Rio de Janeiro, from February 1998 to March 2000.
Keywords: Keloids; bleomycin; healing
RESUMO
As cicatrizes queloidianas podem ser tratadas clínica e/ou cirurgicamente, mas nem o uso de fármacos nem os procedimentos cirúrgicos, até então, as previnem ou curam.
A autora usou injeções intralesionais de bleomicina como uma nova forma de tratamento. A análise histopatológica anterior e posterior às infiltrações demonstra o efeito benéfico do uso da bleomicina, confirmado através da evolução clínica das lesões.
A pesquisa foi realizada em 15 pacientes tratados no Serviço de Cirurgia Plástica do Hospital Universitário Clementino Fraga Filho - Universidade Federal do Rio de Janeiro, entre fevereiro de 1998 e março de 2000.
Palavras-chave: Quelóides; bleomicina; cicatrização
In the normal process of wound healing the collagen metabolism presents a balance between synthesis (through proline hydroxilase)and degradation (due to collagenase activity) phases(1).
This balance is altered in some individuals, resulting in proliferation of a fibrous tissue mass that occurs after injury in the dermis. Keloids are characterized by elevated and extended margins of the wounds; sometimes they have a vegetating or tumoral aspect, are mobile and not encapsulated. Their recurrence rate is high after resection and spontaneous regression is rare. Pruritus and pain are present in most cases. Ulcerations are less often observed, as well as small infected areas draining through small orifices. During the period of greater healing activity, the lesions tend to be hard, reddish or violaceous, and small blood vessels are observed in the surface. As the lesions progress, keloids become less tense and vascularized, but remain elevated and harder than normal tissue. They may appear up to one year after trauma, and there are cases of keloid formation from minimallesions (insect bite) or even non-apparent injury.
Although there are typical clinical manifestations of keloids, it is important to differentiate them from hypertrophic scars, which are also elevated, vascularized, reddish, hard, pruritic, painful and of early development(2-3).
Trussler & Bauer(4), in 1948, suggested the following distinctions: "hypertrophic scars are confined to the area of injury or skin incision, whereas keloids tend to invade the adjacent skin structures. Hypertrophic scars develop for several weeks or months and tend to regress later; keloids continue developing in a bizarre and nodular fashion and do not regress".
The ideal treatment for keloids has not been established yet. Multiple etiologic factors associated with appearance of keloids led to many therapeutical trials, as follows: intralesional infiltration of triamcinolone acetonide(5) and dexamethasone(6,7), topical hydrocortisone(5), radiotherapy(8), betatherapy(9), compression, simple excisional surgery ar associated with infiltration and/or radiotherapy, surgery associated with previous use of hyaluronidase, silicone cream or adhesive gel sheeting(10), laser(11), cryotherapy(12), use of alpha and gamma-interferon in intralesional injections, proline inhibitors, antigrowth factor, minoxidil, pentoxifylline, among others(7,8,13,14).
Bleomycin sulfate was presented by Bodokh & BfUfl(15),in 1996, as an alternative for keloids and hypertrophic scars, based on its action as a deoxyribonucleic acid (DNA) synthesis inhibitor.
This study reports our experience with intralesional infiltration of bleomycin sulfate in keloidal scars, aiming at inhibition of exaggerated skin fibroblast synthesis. Apart from clinical observation, histopathologic examination of alterations during treatment was performed.
METHODS
Fifteen patients seen at the Plastic Surgery Service of Clementino Fraga Filho Teaching Hospital, Universidade Federal do Rio de Janeiro, from February 1998 ta March 2000, were selected. Individuals aged under 14 years, pregnant or nursing women, patients suffering from self-aggressian or any other condition detected in the tests required were excluded.
Females were predominant, accounting for 60% of the patients, and were mestizos (73.3%) or black (26.7%). All individuals had presented the lesions for over one year. All patients complained of pruritus and 93.3% reported pain. Presternal regian and ear lobule were the areas most affected. Positive family history was observed in 26.7% of the patients.
The lesions were measured with a pachymeter and varied in volume; in that, the largest lesion measured 78 cm3.
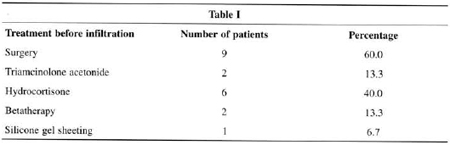
Previous treatments are displayed in Table I. Some patients were submitted to more than one treatment.
All patients were submitted to the following assessment: physical examination, laboratory tests (blood biochemistry, urine analysis) and chest X-ray. Specimens of keloids and healthy adjacent skin were collected for pathological examination. In very large keloids, biopsy was followed by intralesional resection to reduce the size of the lesion and allow better action of the drug.
Bleomycin sulfate solution was prepared by diluting bleomycin sulfate 15 U, 15 mg + sterile water, 5 ml + lidocaine solution 1% without adrenaline, 10 ml, thus producing 1 mg of bleomycin sulfate: 1 ml of solution. It was prepared by the Teaching Hospital Pharmacy just before its application. The volume obtained with one vial of bleomycin sulfate is enough to inject in 15 patients. The subjects were scheduled to be treated together in order not to store the prepared material.
The intralesional infiltration of bleomycin sulfate was initiated when the suture used for biopsy was removed, and then applied every week, up to seven infiltrations for each lesion, at a dose of 1mg/ml/infiltration session. The dose was injected using 1-ml syringes with 27.5 gauge (13 x 3.8) needles. The skin surrounding the lesion was punctured at an angle of approximately 30° to 45°, and the fluid was distributed in the area chosen. The same area was used in each session. Infiltration depth was limited to the dermis.
The patients were allowed to go back to daily activities after remaining a few minutes at the outpatient clinic for observation.
After completing the first phase of treatment, all patients were submitted to total or partial excision of the lesion and the specimen was sent for pathological examination by the following methods:
• Hematoxylin-eosin - to assess morphological alterations observed in dermis.
• Gomori stains - to observe details in collagen fiber alterations.
• Una-Tanzer Orcein - to observe elastic fibers in middle to lower dermal layers.
• Colloidal-iron staining - to assess presence and distribution of interstitial mucopolysaccharides.
• Picrosirius - to show collagen and reticular fibers.
RESULTS
The optical microscopy findings(7,16), observed in the specimens before bleomycin sulfate infiltrations, are grouped as follows in Table II & Figs. 1a and 2a.
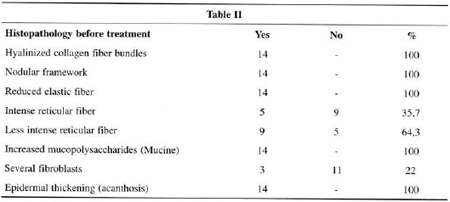
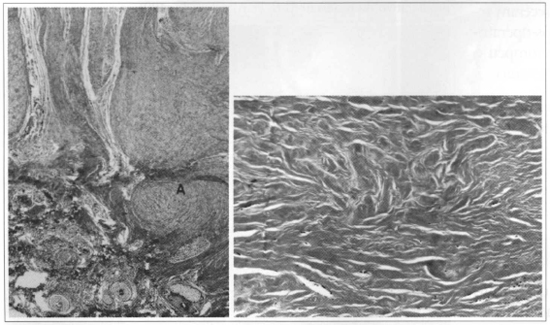
Fig. 1 - a) Before treatment, observe the nodular arrangement of collagen fibers (A). Gomori stains (x40). b) After use of bleomycin, note marked hypocellularity, hyalinization and disorganization of connective tissue in the central part of the keloid. Gomori stains (x100).
After infiltrations, the histopathological aspects were observed in Table III & Figs.1b and 2b.
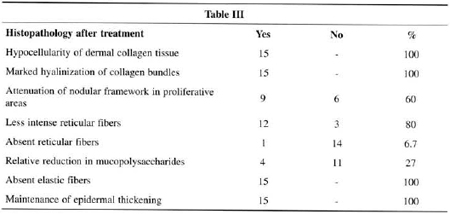
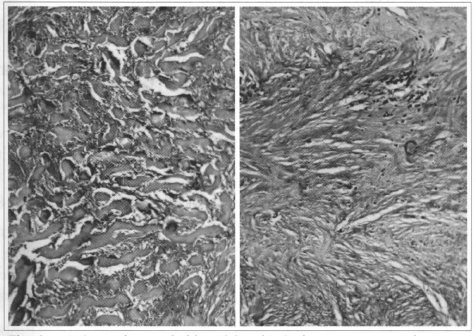
Fig. 2a - Before use of bleomycin. b) After treatment, observe marked reduction in mucopolysaccharides and modified fibrous tissue proliferarive partern. Colloidal iron staining (x400).
The maximum of seven applications of bleomycin sulfate was necessary to show reduced volume of the infiltrated area. In 7 patients (46.7%), volume reduction occurred in the fourth session. Fourteen patients were submitted to total resection of the lesions.
In a subjective analysis, all patients were encouraged by treatment, and reported decreased volume of the area infiltrated and recurrence control. The objective analysis was carried out by the author, who observed decreased volume of the lesion in all cases (100%). Reduced keloid texture was also observed in 100% of the cases, and occurred up to the fourth session. Eleven patients treated reported no pruritus and pain as of the first session (Figs. 3-6).
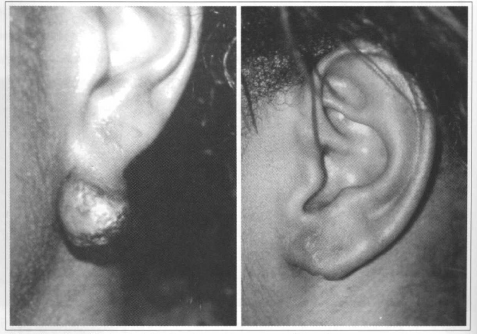
Fig. 3 - Ear lobule keloid after piercing for earrings: a) Before infiltration. b)Twelve months after infiltration with bleomycin and intralesional resection.
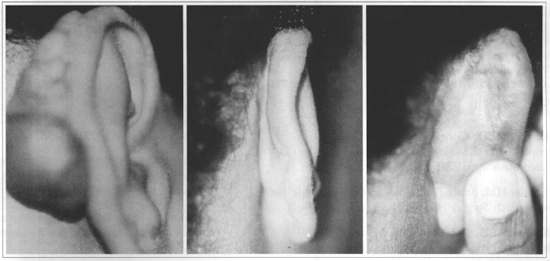
Fig. 4 - Retroauricular keloid in scar for bat car surgical correction: a) Before infiltration. b,c) Twelve months after infiltration with bleomycin and intralesional resection.
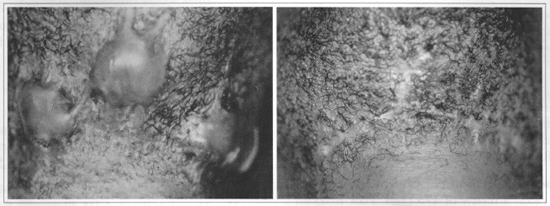
Fig. 5 - Submental keloid in lesions caused by shaving: a) Before infiltration. b) Twelve months after infiltration with bleomycin and intralesional resection.
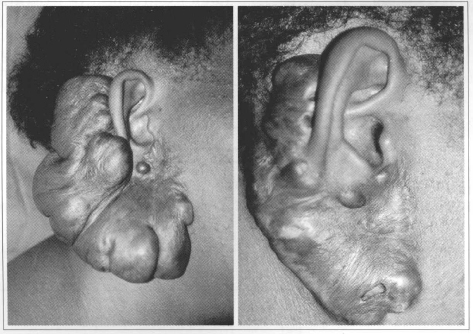
Fig. 6 - Extremely aggressive lesion after piercing for earrings. This patient was submitted only to infiltration with bleomycin; observe marked regression and softening of the lesion. a) Before treatment. b) After 6 infiltrations. No resection was performed. The scar observed in the lateral contour of the lesion refers to previous resection performed before infiltrations that relapsed.
The following complications were observed: skin reaction related to cytotoxicity of the compound used (17),epidermolysis (53.3%), hyperpigmentation (20%) and blistering (13%).
DISCUSSION
Poor quality scars may occur in any individual; however keloids are characteristic of certain patients and are not very common. They result from a complex combination of as yet not completely identified etiologic factors; and are usually not related to the surgical technique used or surgeon's skills(l8-20).
All techniques proposed to treat keloids present good or bad results. Some patients are resistant to any type of treatment available, whereas others benefit frorn some therapy or not. The usual keloid patient is submitted to several types of treatment until achieving, or not achieving, the best result; and this varies among individuals.
For the past 20 years, keloids have been treated at our Service using hydracortisone or triamcinolone infiltrations, betatherapy, surgery or combinations of several therapeutical methods. High recurrence rates have been observed.
The study by Bodokh(15), published in 1996 and using bleomycin sulfate infiltration seemed to be a new and interesting option(21,22).As compared with other therapies, cost proved to be lower by gathering patients in only one group and using one solution vial divided into 15 doses. Moreover, bleomycin sulfate is available at public hospitals.
Fifteen patients presenting a lesion for over one year were selected; 10 of whom had already been submitted to unsuccessful treatments.
It is not simple to carry out a study with this type of patient. They have been disappointed with several treatments, do not trust another therapy and are ready to give up if results are not promptly achieved or meet their expectations.
Out of 31 patients initially selected, 15 (48.3%) concluded the study. Among the dropout patients, 14 initiated treatment and abandoned between the third and fourth sessions because they expected more rapid results; and two patients did not agree with the prolonged period waiting for approval by the Research Ethics Committee, and were afraid of presenting alopecia and severe anemia as complications.
The following complications occurred during infiltration periods: hyperpigmentation, blistering and keloid epidermolysis. Bodokh reported the same complications in the original study(15).
Although the initial plan was not to completely excise all lesions, the favorable clinical progression with less pruritus and pain, as well as evident reduced volume, led to indication of surgical procedure. Patient's desire, encouraged by improved lesions, contributed to this end.
The histopathological findings of biopsies performed before the infiltrations with bleomycin sulfate demonstrated results similar to those reported by other authors(14,16,18). Therefore, granulation tissue collagen fibers are arranged in hyalin bundles in normal scar. Unlike, in keloids, they present a nodular partem until they become thick bundles, compacted and hyalinized. When the collagen condensation nodule is in the papillar dermis, the epidermis may be elevated. Mature keloids have markedly thick and hypereosinophilic collagen bundles, with few elastic fibers and structures.
In 9 (60%) patients, volume reduction of keloidal scar after bleomycin sulfate infiltrations coincided with the histopathological findings of modified nodular pattern, which is characteristic of these lesions and was observed, before treatment, in all 15 patients studied.
Hypocellularity especially identified by absent nuclei, marked hyalinization of collagen bundles, absent elastic and reticular fibers in 100% of the cases, reduced interstitial acid mucopolysaccharides, as well as modified proliferative pattern of fibrous tissue in nine cases, are morphological evidences of the major alteration produced in the structural aspect of the lesions after treatment. Moreover, they correlate with softening of hardened texture, usually observed in these lesions.
We performed control infiltrations in the areas manipulated by detachment to close the surgical wounds, in an attempt to inhibit reactivation of the events that promote hypertrophic scars.
Four (26.7%) patients relapsed - they had not come regularly to postoperative sessions; one of these patients discontinued treatment during pregnancy and breastfeeding.
The patients were followed-up for 15 months, up to March 2000. Although it is a short period to draw definite conclusions, the results obtained are encouraging and should foster further studies.
CONCLUSIONS
1. Intralesional infiltration with bleomycin sulfate to treat keloidal scars proved to be effective in reducing pruritus, pain, and primarily, lesion volume. The drug is well tolerated. A low recurrence rate corroborates this view.
2. Treatment enabled reduction of relapses (26.7%) in a 12-month period, as compared with other procedures the patients had been submitted to.
3. Smaller volume lesions presented better results.
4. Bulky lesions should be reduced before infiltration in order to achieve the same results with lower morbidity.
REFERENCES
1. Peacock EEJR. Inflamation and cellular response to injury in wound healing. 30 ed. Philadelphia: WB Saunders; 1984.
2. Datubo-Brown DD. Keloids: a review of the literature, Br J Plast Surg. 1990; 43:70-7.
3. Ketchum LD, Cohen IK, Masters FW. Hypertrophic scars and keloids: a collective review. Plast Reconstr Surg. 1974; 53:140-54.
4. Trussler HM, Bauer TB. Keloids and hypertrophic scars. Arch Surg. 1948; 57(4):539-52.
5. Ketchum LD, Robinson DW, Masters FW. Follow-up on treatment of hypertrophic scars and keloids with triamcinolone. Plast Reconstr Surg. 1971; 48:256-9.
6. Asboe-Hansen G, Brodthagen H, Zachariae L. Treatment of keloids with topical injections of hydrocortisone acetate. Arch Dermat & Syph.1956; 73: 162-5.
7. Colucci NRS. Estudo histopatológico do efeito da infiltração de bleomicina no tratamento das cicatrizes hipertróficas e queloidianas [Tese]. 2000. Faculdade de Medicina da Universidade Federal do Rio de Janeiro, Rio de Janeiro.
8. Alhady SM, Sivanananthrajah K. Keloids in various races: a review of 175 cases. Plast Reconstr Surg. 1969; 44(6):564-6.
9. Barron JN. Essai de prévention des cicatrices chéloidiennes par I'emploi des rayons bêta. Ann Chir Plast 1956; 32:29.
10. Gold MH. A conrroled clinical trial of topical silicone gel sheeting in the treatment of hypertrophic scars and keloids. J Am Acad Dermatol 1994; 30:506-7.
11. Henning JPH, Roskam Y, VanGemert MJC. Treatment of keloids and hypertrofic scars with an argon laser. Lasers in Surg. Med 1986; 6:72-5.
12. Muti E, Ponzio E. Cryotherapy in the treatment of keloids. Ann Plast Surg. 1983; 3:227-32.
13. Bloch EF, Hall MG, Denson MJ, Slay-Solomon V. General immune reactivity in keloid patients. Plast Reconstr Surg. 1984; 73(3):448-51.
14. Cosman B, Crikelair GF, Ju DMC, Gaulin JC, Lattes R. The surgical treatment of keloids. Plast Reconstr Surg. 1961; 27:335-58.
15. Bodokh I, P Brun. Traitement des chéloides par infiltrations de bléomycine. Ann Dermatol Venereol 1996; 123:791-4.
16. Hunter JAA, Finlay JB. Scanning electron microscopy of normal human scar tissue and keloids. Br J Surg. 1976; 63: 826-30.
17. Bennett JM, Reich SD. Bleomycin. Ann lntern Med. 1979; 90: 945-8.
18. Calnan JS, Copenhagen HJ. Autotransplantation of keloid in mano Brit J Surg. 1967; 54:330-5.
19. Glücksmann A. Local factors in the histogenesis of hypertrophic scars. Brit J Plast Surg. 1951; 4:88- 103.
20. Yagi Kl, Daffalla AA. Does an immune reaction to sebum in wounds cause keloid scars? Beneficial effect of desensitisation. Br J Plast Surg. 1979; 32:223-5.
21. Manz LA, Pelachyk JM. Bleomycin-lidocaine mixture reduces pain of intralesional injection in the treatment of recalcitrant verrucae. J Am Acad Dermatol. 1991; 25(3):524-6.
22. Vanhooteghem 0, Song M. Place de la bléomycine intralésionnelle dans le traitement des verrues. Ann Dermatol Venereol. 1996; 123:53-8.
I - Senior Lecturer of Universidade Federal do Rio de Janeiro (UFRJ).
II - Head Professor of UFRJ.
Study Performed at the Plastic Surgery Service of Clementino Fraga Filho Hospital,UFRJ. Synthesis of the Master's degree thesis by the main author.
Address for correspondence:
Nícia Rodrigues dos Santos Colucci, MD
Av.das Américas, 500 - bl. 4 - cob 320
22640-100 - Rio de Janeiro - RJ Brazil
e-mail: ncolucci@terra.com.br


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter