

Original Article - Year 2017 - Volume 32 -
Rhytidectomy with tunneling combined with liposuction and reduced detachment
Ritidoplastia com tunelização associada a lipoaspiração e descolamento reduzido
ABSTRACT
INTRODUCTION: Multiple facial rejuvenation techniques have been used to obtain satisfactory results with minimal complications. With the introduction of liposuction for facial surgery, treatment of the cervical region has improved. This study aimed to describe a technique using preceding liposuction combined with reduced detachment and plication of the superficial muscular aponeurotic system/platysma for treatment of facial aging.
METHODS: We retrospectively analyzed the results in 129 patients who underwent surgery between 2005 and 2015.
RESULTS: The patients reported satisfaction with the surgical technique, a low complication rate, and early return to work.
CONCLUSIONS: Rhytidectomy with tunneling combined with liposuction and selective detachment is effective, with good mobility of the overlying skin flap; the technique is safe and reproducible, and is an option for the treatment of facial aging.
Keywords: Rhytidoplasty; Postoperative complications; Rejuvenation; Skin aging; Surgical flaps.
RESUMO
INTRODUÇÃO: Várias técnicas de rejuvenescimento facial buscam encontrar resultados satisfatórios com mínimas complicações. Com a introdução da lipoaspiração, a cirurgia da face teve um grande benefício na região cervical. O objetivo deste estudo é demonstrar a técnica de tunelização associada a lipoaspiração prévia e descolamento reduzido da face e plicatura do SMAS/ platisma para tratamento do envelhecimento facial.
MÉTODOS: Foram analisados retrospectivamente os resultados obtidos com 129 pacientes operados entre 2005 e 2015, com a tática cirúrgica proposta, aqui demonstrada.
RESULTADOS: Os pacientes apresentaram boa satisfação com a tática cirúrgica utilizada, baixo índice de complicações e retorno rápido ao trabalho.
CONCLUSÕES: A ritidoplastia com tunelização associada a lipoaspiração e descolamento seletivo é efetiva, com boa mobilidade e segurança do retalho cutâneo suprajacente, reprodutível, sendo uma opção no tratamento do envelhecimento facial.
Palavras-chave: Ritidoplastia; Complicações pós-operatórias; Rejuvenescimento; Envelhecimento da pele; Retalhos cirúrgicos.
According to data from the International Society for Aesthetic Plastic Surgery, 23 million plastic surgeries were performed in 2014, Brazil being the market where most surgical procedures were performed. In 2015, in Brazil alone, 1.5 million plastic surgeries were performed.
The demand for both surgical and nonsurgical facial rejuvenation procedures has increased progressively, in association with increased population aging, as well as the incessant search for improvement of self-esteem and quality of life.
Recently, with the advent of bariatric surgery, patients with large weight loss followed by skin flaccidity in the facial region have perceived a decline in self-image and the appearance of early aging, contributing to further increases in the desire for facial rejuvenation surgery.
It is well known that aspects of facial aging vary greatly, with different degrees of flaccidity, necessitating individualized treatment. Consequently, multiple techniques have been devised, ranging from isolated procedures with small detachments to large detachments and combined treatment methods.
With the introduction of liposuction for facial surgery, treatment of the cervical region has improved, resulting in a better facial contour. It was observed that cannulation along the tension lines of the skin resulted in facial rejuvenation, even without aspiration1.
The present work aimed to describe tunneling with preceding facial liposuction and reduced detachment, combined with plication of the superficial muscular aponeurotic system (SMAS)/platysma, enabling good repositioning of the facial structures and extensive cutaneous resection without tension.
OBJECTIVE
To demonstrate the combination of preceding liposuction and reduced facial detachment, with plication of the SMAS/platysma for treatment of facial aging.
METHODS
A retrospective, longitudinal, descriptive, and uncontrolled study of 129 patients undergoing rhytidectomy from 2005 to 2015 at the Vera Cruz Hospital and a private clinic in Belo Horizonte, MG, Brazil, was performed. All patients underwent surgery by the author in his private practice, using a technique of tunneling and preceding facial liposuction with reduced detachment, combined with strong plication of the SMAS/platysma. Variations of lipoaspiration intensity, incision size, and combinations with blepharoplasty or ring procedures were performed, depending on the case.
Inclusion criteria: Patients with facial aging who underwent rhytidectomy by the author between 2005 and 2015, regardless of sex or age.
Exclusion criteria: patients with facial aging who underwent rhytidoplasty using another technique or cases in which the author was an assistant.
Exclusion criteria: patients who did not return for follow-up and those without postoperative photographs.
The parameters analyzed were sex, age, presence of comorbidities, primary/secondary surgery, type of anesthesia, procedure site, associated procedures, complications, patient satisfaction, and need for retouching.
The attached photographs were taken preoperatively and 2 months postoperatively. Patient follow-up was performed for 1 year to monitor scar maturation. The study followed the principles of Helsinki and all patients signed an informed consent form. Published pictures were by The patients authorized publication of their photographs.
Marking was performed in the operating room prior to surgery. Marking started in the temporal region at the hairline, and extended caudally in the preauricular and pretragal region, circumventing the earlobe posteriorly. At the level of the tragus, the line arced, continuing caudally in the hairline for 4 to 5 cm (Figure 1).
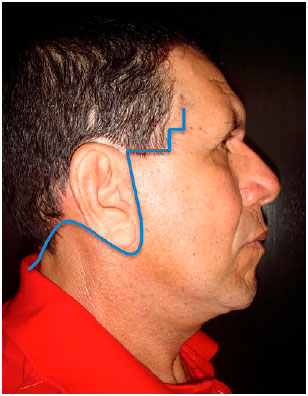
Figure 1. Schematic representation of preoperative marking.
Antibiotic prophylaxis was performed with 2 g of cephalothin. Clindamycin was used in patients allergic to cephalothin.
Prophylaxis for deep venous thrombosis was performed in all patients using stockings and intermittent compression. Enoxaparin was used in specific cases.
General and local anesthesia were used. Surgery was performed at the Vera Cruz Hospital and a private clinic in Belo Horizonte, MG.
Injection of ropivacaine and lidocaine combined with epinephrine at a concentration of 1:200,000 was used for local anesthesia. When general anesthesia was used, injection was performed after anesthetic induction.
The procedure began with liposuction of the infiltrated area, which corresponded to the area to be detached, comprising a half circle that tangentially lifted the malar area in a temporal direction and 1 cm in front of the angle of the mandible, extending in a cervical direction, as demonstrated in Figure 2. Liposuction varied according to the thickness of facial adipose tissue, and the cannula was only used for tunneling and preceding detachment of tissue in slender patients or those with slightly oily skin, thus avoiding fine-tuning of the skin flap to be detached.

Figure 2. Detail of the area to be detached and access incisions for liposuction.
It is important to note that cervical liposuction exceeds the delimited marking when necessary, up to the midline, for better definition of the neck and jaw line. Cutaneous detachment was restricted to the demarcated area, resulting in reduced detachment sufficient for SMAS plication. We used a 2.5 or 3 mm cannula, with access incisions at the earlobe and sideburns.
Next, the demarcated area was removed, at first with a scalpel, and then with scissors, in the supra-SMAS plane. Washing of the detached region was performed with physiological saline, and rigorous hemostasis was performed. Plicature was performed with interrupted 3-0 nylon sutures, with the knot facing the deep plane, using a J-shaped line marked with methylene blue, as shown in Figure 3.

Figure 3. J-shaped plicature area with traction vectors in the malar region, mandible, and cervical angle.
The traction vector is more vertical at the level of the malar prominence, going toward the zygomatic arch, whereas it is more oblique in the region of the mandible and cervical angle, creating stronger traction at these locations, to precisely delimit the contour of the jaw and neck. It should be noted that plication must follow the precept of "soft in hard," in order to trap the SMAS in fixed structures, such as Lore's fascia or the zygomatic arch, to ensure long-lasting results. When necessary, a purse-string suture was made anterior to the earlobe to prevent traction, as advocated by Hakme2.
Figure 4 shows repositioning of the SMAS and platysma after plication, and consequently the middle-inferior third of the face; the residual detachment area becomes very small, in order to ensure vascular safety for the adjacent skin flap. When necessary, a submental incision was made, with scissors detachment in the medial region, between the medial borders of the platysma, combined with lipectomy and medial plication with 4-0 mono nylon interrupted sutures.
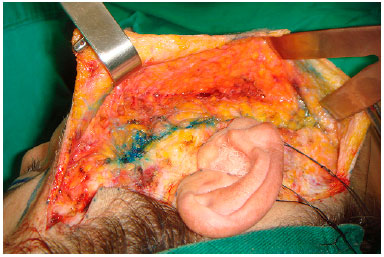
Figure 4. Residual bloody area after SMAS plication.
SMAS plication clearly shows cutaneous excess, without the need for excessive traction in these tissues, thereby facilitating demarcation and resection of the excess. Superior preauricular and retroauricular initial points of skin traction and repositioning were then tacked with 4-0 nylon, anterior to the curvature that descends to the hairline (Figure 5). From there, the demarcated skin was dried, as shown in Figure 6. It is possible to control the amount of skin removed, with or without minimum tension, in order to avoid future scar hypertrophy.
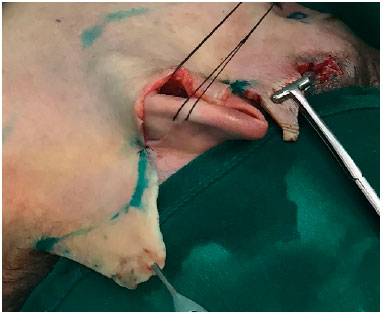
Figure 5. Initial traction points and demarcation of skin area to be resected.

Figure 6. Detached area and cutaneous area to be resected.
Figure 7 demonstrates tension less skin manipulation after resection. Subdermal 4-0 Monocryl sutures were placed and intradermal suturing was completed with the same thread.

Figure 7. Non-tensioned skin manipulation.
At the lobe level in the preauricular region, a triangular cutaneous flap was made to leave the ear loose, and to avoid local retraction (Figure 8).

Figure 8. Finished suture with triangular flap detail.
At the end, a "Pizzaiolo maneuver" is performed with a compress to drain accumulated fluids, and a compressive dressing is applied with open gauze and 15 cm crepe. Drains are not used.
The dressing is left in place until discharge, when the surgical wound is inspected and a new dressing is placed using elastic mesh for the face. Hospital discharge occurred on the same or next day. Painkillers, antiinflammatories, and enoxaparin were prescribed as needed.
Patients returned 3 to 5 days after surgery, especially when blepharoplasty was also performed. All sutures were removed at 14 days (usually in the retroauricular region). Patients returned to their usual activities at 7 to 14 days (10 on average) after surgery.
RESULTS
A total of 129 patients underwent rhytidoplasty between 2005 and 2015.
Figure 9 shows that most were 50 to 60 years old. The oldest was 82 years old, and the youngest was 36.
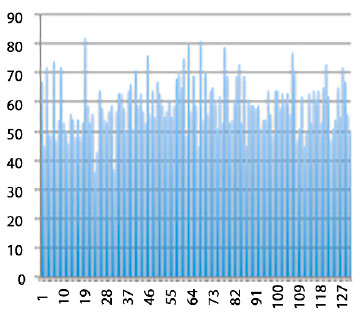
Figure 9. Patient age data.
Of 129 patients, 120 were women and 9 were men (Figure 10).
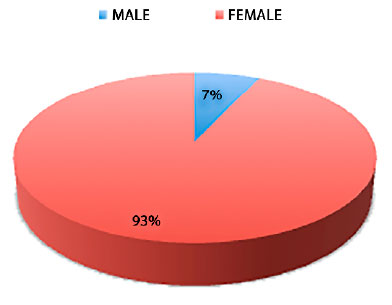
Figure 10. Patient distribution by sex.
A total of 105 were in good health, with no comorbidities; hypertension was present in 22 patients. These patients were advised of surgical risk, and required clearance by a cardiologist before surgery. Four patients who used tobacco were advised to stop smoking 30 days before surgery. None of the smokers had postoperative skin flap necrosis (Figure 11).
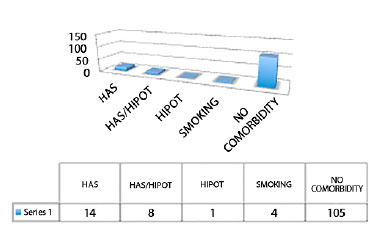
Figure 11. Presence of comorbidities and smoking.
A total of 114 patients who underwent rhytidoplasty also had eyelid surgery. In 15 cases, only rhytidoplasty was performed using the technique described.
In 8 patients, the facial rejuvenation procedure was performed for the second time (secondary rhytidectomy), while 121 had surgery for the first time (primary rhytidectomy). There were no cases of tertiary rhytidoplasty.
In 108 patients, general anesthesia was preferred by the anesthesiology and surgical teams. In 20 outpatient cases, local anesthesia with sedation was used (Figure 12).
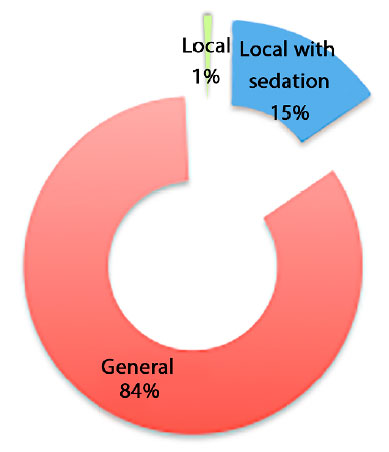
Figure 12. Type of anesthesia used.
Only one case was performed with local anesthetic alone, at the patient's request.
A total of 123 high-complexity cases underwent surgery at the Vera Cruz Hospital.
Frontal facelifts were not performed, as these are usually restricted to selected cases. However, ancillary postoperative procedures, including filling with hyaluronic acid and botulinum toxin injection, were necessary to obtain better results (Figure 13). Exfoliative skin treatments with acids and lasers were also not performed.
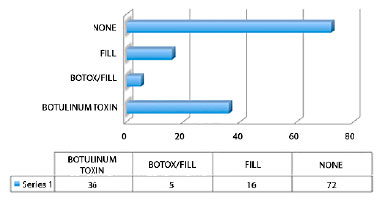
Figure 13. Complementary procedures in the postoperative period.
Complications included 3 small hematomas, with 1 drained at the bedside. Four cases developed hypertrophic scars, which we attributed to the initial learning curve, when we erroneously used excessive cutaneous traction. One case of neuropraxia resolved spontaneously within 30 days. Two cases of retroauricular epidermolysis were observed.
The complications were treated conservatively, with good patient satisfaction. No cases required retouching or reintervention.
The patients returned to their usual activities in 7 to 14 days (10 days on average).
Some patients who underwent this surgical technique are shown in Figures 14, 15 and 16.

Figure 14. A: Preoperative - primary rhytidoplasty with superior blepharoplasty. 51-year-old patient. Front view; B: Preoperative - primary rhytidectomy with superior blepharoplasty. Oblique view; C: Preoperative - primary rhytidectomy with superior blepharoplasty. Side view; D: Postoperative - primary rhytidectomy with superior blepharoplasty. Front view; E: Postoperative - primary rhytidoplasty with superior blepharoplasty. Oblique view; F: Postoperative - primary rhytidectomy with superior blepharoplasty. Side view.

Figure 15. A: Preoperative - primary rhytidectomy with upper and lower blepharoplasty. 64-year-old patient. Front view; B: Preoperative - primary rhytidectomy with upper and lower blepharoplasty. Oblique view; C: Preoperative - primary rhytidectomy with upper and lower blepharoplasty. Side view; D: Postoperative - primary rhytidectomy with upper and lower blepharoplasty. Front view; E: Postoperative - primary rhytidectomy with upper and lower blepharoplasty. Oblique view; F: Postoperative - primary rhytidectomy with upper and lower blepharoplasty. Side view.

Figure 16. A: Postoperative - primary rhytidoplasty. 63-year-old patient. Front view; B: Preoperative - primary rhytidoplasty. Oblique view; C: Preoperative - primary rhytidoplasty. Side view; D: Postoperative - primary rhytidoplasty. Front view; E: Postoperative - primary rhytidoplasty. Oblique view; F: Postoperative - primary rhytidoplasty. Side view.
DISCUSSION
Several changes result from facial aging; some are progressive and some are simultaneous, consisting mainly of a decrease in skin thickness and elasticity, a decrease in adhesion to adipose tissue, which gradually undergoes absorption, ptosis of the soft tissues, in addition to formation of skin folds in the lines of adhesion in the skin and areas of muscular insertion, producing typical wrinkles. Bone resorption and weakening of the orbital structures also occur, with protrusion of orbital fat.
The surgical approach will depend on these findings. Several surgical techniques aim to attenuate the effects of aging, using SMAS, subperiosteal, high SMAS, and subcutaneous detachments, among others, to achieve natural results and minimize complications. Some techniques achieve excellent results, but with a higher risk of nerve damage and longer recovery time, as in the rhytidectomy proposed by Hamra3,4.
Patients demand satisfactory results, with rapid recovery and absence of complications5. Aggressive surgery with excessive detachment will not necessarily achieve this end. The current trend toward less invasive and less aggressive techniques will reduce complications and enable earlier return to usual activities6-10.
These principles guided the surgical approach to rhytidoplasty:
• Initial tunneling of the face with liposuction cannulas, preceded by aspiration of fat when necessary;
• Reduced subcutaneous facial skin detachment, comprising a half circle that tangentially elevated the malar region in a temporal direction, and 1 cm in front of the angle of the mandible, directed in a cervical direction;
• Strong plication of SMAS/platysma and fixation of points in firm structures, preventing early relapse of SMAS flaccidity;
• Resection of skin with as little tension as possible, preventing scar hypertrophy.
Persistent trabeculae after skin tunneling show intact neurovascular connections, as demonstrated by Daher in his work on lipofacelifting11,12 and by Almeida et al.13. In 2005, Luz et al.14 described an interesting idea for flap detachment using numbers 1 to 6, bifaced dilators/detachers, with diameters varying between 1.5-20 mm, to promote stretching of the vessels with total detachment of the facial flap and reduction of bleeding based on the principle of early migration of coagulation factors and cellular elements. The skin is easily mobilized with traction, similar to that observed in more extensive dissections. We observed results in facial subcutaneous tissue similar to those in abdominal subcutaneous tissue during lipoabdominoplasty, with great mobility and preservation of perforators15,16.
This enables adequate cutaneous traction, with less detachment and better security for the skin flap, by preserving sensitive vessels and nerves. This technique can even be applied in smokers, although smoking should always be discouraged and the risks explained.
In our series, the rate of complications was low. In 129 operated cases, 3 small hematomas occurred; 1 was drained at the bedside, and 2 others were drained with retroauricular punctures in the office. These cases accounted for 2.32% of all cases, consistent with a report by Baker17, in which 3.5% of cases presented with hematomas.
Four cases of retroauricular hypertrophic scarring occurred, which we attributed to initial learning, when we mistakenly used exaggerated cutaneous traction. One case had frontal neuropraxia, possibly caused by the electric scalpel, with spontaneous resolution in 30 days. Despite the greater vascular safety of this technique, 2 cases of retroauricular epidermolysis were observed, attributed to elastic mesh compression and possible increased traction at the site. These were treated conservatively, with good resolution. In one case, the scar was hypertrophied, but the patient did not want correction.
Complications were treated conservatively, with good resolution. No cases required retouching or reintervention, showing the safety and good results obtained with the surgical methods used. There was little postoperative edema and early return to usual work activities.
Because we also train residents to use these surgical methods, we aimed for reproducibility, with a low rate of complications, ease of teaching, and education in safety for future colleagues in plastic surgery. In addition, the operative time was less than with conventional rhytidoplasty18-20.
CONCLUSION
A surgical approach using tunneling combined with facial liposuction and less detachment and plication of the SMAS/platysma is selective and effective, with great mobility and safety of the overlying skin flap. The aesthetic results showed low rates of complications and early return to usual work activities.
This method is therefore a good choice and is reproducible, for use in treatment of facial deformities caused by aging.
COLLABORATIONS
GCGG Performance of experiments and writing the manuscript; analysis and/or interpretation of data; conception and design of the study.
MGG Critical review of its contents; final approval of the manuscript.
REFERENCES
1. Matarasso HA, Aston SJ. The suction cannula: retractor in facial plasty. Plast Reconstr Surg. 1987;80(6):869-70. DOI: http://dx.doi.org/10.1097/00006534-198712000-00041
2. Hakme F. SMAS: platysma in cervico-facial rhytidectomy: experience and results. Rev Bras Cir. 1982;72:105-10.
3. Hamra ST. The zygorbicular dissection in composite rhytidectomy: an ideal midface plane. Plast Reconstr Surg. 1998;102(5):1646-57. PMID: 9774027 DOI: http://dx.doi.org/10.1097/00006534-199810000-00051
4. Psillakis JM, Rumley TO, Camargos A. Subperiosteal approach as an improved concept for correction of the aging face. Plast Reconstr Surg. 1988;82(3):383-94. PMID: 3406175 DOI: http://dx.doi.org/10.1097/00006534-198809000-00001
5. Tonnard P, Verpaele A. The MACS-lift short scar rhytidectomy. Aesthet Surg J. 2007;27(2):188-98. DOI: http://dx.doi.org/10.1016/j.asj.2007.01.008
6. Ferreira LM, Hochman B, Locali RF, Rosa-Oliveira LM. Astratigraphic approach to the superficial musculoaponeurotic system and its anatomic correlation with the superficial fascia.
Aesthetic Plast Surg. 2006;30(5):549-52. DOI: http://dx.doi.org/10.1007/s00266-005-0167-0
7. Castro CC, Aboudib JHC, Giaquinto MGC, Moreira MBL. Avaliação sobre Resultados Tardios em Ritidoplastia. Rev Bras Cir Plást. 2005;20(2):124-6.
8. Menezes MVA, Abla LEF, Dutra LB, Junqueira AE, Ferreira LM. Avaliação dos resultados do mini-lifting modificado: estudo prospectivo. Rev Bras Cir Plást. 2010;25(2):285-90.
9. Gomes Filho BS, Fleishmann Júnior HW, Caldellas AV, Colombo FG, Andrade AAM. Ritidoplastia com cicatriz periauricular. Rev Bras Cir Plást. 2009;24(4):488-96.
10. Zani R, Fadul R Jr, Da Rocha MA, Santos RA, Alves MC, Ferreira LM. Facial nerve in rhytidoplasty: anatomic study of its trajectory in the overlying skin and the most common sites of injury. Ann Plast Surg. 2003;51(3):236-42. PMID: 12966233 DOI: http://dx.doi.org/10.1097/01.SAP.0000063755.42122.5F
11. Daher M. Lipofacelift: plástica facial com descolamento mínimo da pele. Rev Bras Cir Plást. 2009;24(4):479-87.
12. Daher JC, Cosac OM, Domingues S. Face-lift: the importance of redefining facial contours through facial liposuction. Ann Plast Surg. 1988;21(1):1-10. DOI: http://dx.doi.org/10.1097/00000637-198807000-00001
13. Almeida ARH, Menezes JA, Araújo GKM, Mafra AVC. Utilização de plasma rico em plaquetas, plasma pobre em plaquetas e enxerto de gordura em ritidoplastias: análise de casos clínicos. Rev Bras Cir Plást. 2008;23(2):82-8.
14. da Luz DF, Wolfenson M, Figueiredo J, Didier JC. Full-face undermining using progressive dilators. Aesthetic Plast Surg. 2005;29(2):95-9. DOI: http://dx.doi.org/10.1007/s00266-003-0131-9
15. Saldanha OR. Ritidoplastia com descolamento seletivo. In: Luz D, ed. Técnica Dílson Luz. Tunelizações progressivas: princípios, aplicações e procedimentos complementares. Rio de Janeiro: Dilivros; 2010. p. 99-108.
16. Saldanha OR, Azevedo SFD, Saldanha Filho OR, Saldanha CB, Chaves LO. Ritidoplastia com descolamento composto. Rev Bras Cir Plást. 2010;25(1):135-40.
17. Baker D. Rhytidectomy with lateral SMASectomy. Facial Plast Surg. 2000;16(3):209-13. DOI: http://dx.doi.org/10.1055/s-2000-13591
18. Avelar J. Fat-suction of the submental and submandibular regions. Aesthetic Plast Surg. 1985;9(4):257-63. DOI: http://dx.doi.org/10.1007/BF01571044
19. Cardoso de Castro C, Aboudib JH Jr. Extensive cervical and lower face lipectomy: its importance and anatomical basis. Ann Plast Surg. 1980;4(5):370-5. DOI: http://dx.doi.org/10.1097/00000637-198005000-00003
20. de Souza Pinto EB. Importance of cervicomental complex treatment in rhytidoplasty. Aesthetic Plast Surg. 1981;5(1):69-75. DOI: http://dx.doi.org/10.1007/BF01981685
Hospital Vera Cruz, Belo Horizonte, MG, Brazil
Institution: Hospital Vera Cruz, Belo Horizonte, MG, Brazil
Corresponding author:
Guilherme de Castro Greco Guimarães
Rua Marechal Hermes, 200/301 - Bairro Gutierrez
Belo Horizonte, MG, Brazil - Zip Code 30441-028
E-mail: guilhermecastrogrecoguimaraes@gmail.com
Article received: October 14, 2016.
Article accepted: July 10, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter