

Original Article - Year 2017 - Volume 32 -
Surgical treatment of involutional lower lid entropy
Tratamento cirúrgico do entrópio palpebral inferior involucional
ABSTRACT
INTRODUCTION: Entropion is defined as an internal rotation of the eyelid margin. The contact of the eyelid skin and eyelashes with the eye may result in irritating symptoms, corneal abrasions, and scars. The purpose of this study is to present the effectiveness of the technique described by Lessa in the treatment of involutional entropion.
METHODS: We underwent correction of involutional entropion on 13 lower eyelids. We used the Lessa technique, in which a subciliary incision was made, a skin flap was dissected from the orbicularis oculi, a muscle strip was resected, and a skin-septum-skin suture was made. The procedure was associated with lateral support.
RESULTS: There were 11 patients (5 men and 6 women) with a mean age of 76.72 years (69 to 84 years), totaling 13 eyelids, as two patients had bilateral pathology. Eight patients (9 eyelids) used muscular suspension technique. In one patient, the tarsal suspension was performed, and in two patients (three eyelids), we used the tarsal flap. The mean operative time (for eyelid) of patients undergoing muscle suspension was 36.55 min, while that in patient undergoing canthoplasty was 56 min. No patient had recurrence, and one patient developed ectropion.
CONCLUSION: The technique described by Lessa proved to be effective since there was no recurrence.
Keywords: Entropy; Eyelid diseases; Reconstructive surgical procedures
RESUMO
INTRODUÇÃO: O entrópio é definido como uma rotação interna da margem palpebral. O contato dos cílios e da pele palpebral com o globo ocular pode resultar em sintomas irritativos, abrasões e cicatrizes corneanas. Este trabalho tem o objetivo de apresentar a eficácia da técnica descrita por Lessa no tratamento do entrópio involucional.
MÉTODOS: Foram submetidos à correção do entrópio involucional 13 pálpebras inferiores de 11 pacientes. Utilizou-se a técnica de Lessa, em que é realizada uma incisão subciliar, descolamento subcutâneo, ressecção de faixa muscular e sutura pele-septo-pele, associada a um procedimento de suporte lateral.
RESULTADOS: Foram operados 11 pacientes (5 homens e 6 mulheres), com média de idade de 76,72 anos, (69 até 84 anos), totalizando 13 pálpebras, pois dois pacientes apresentavam a afecção bilateralmente. Em oito pacientes (9 pálpebras) usou-se a suspensão muscular. Em um paciente, a suspensão tarsal, e em dois (três pálpebras) o retalho tarsal. O tempo cirúrgico médio (por pálpebra) dos pacientes submetidos à suspensão muscular foi de 36,55 minutos, enquanto nos submetidos à cantoplastia foi de 56 minutos. Nenhum paciente apresentou recidiva e um paciente apresentou ectrópio.
CONCLUSÃO: A técnica descrita por Lessa mostrou-se eficaz, pois não houve nenhum caso de recidiva.
Palavras-chave: Entrópio; Doenças palpebrais; Procedimentos cirúrgicos reconstrutivos.
Entropion is characterized by the inversion of the palpebral margin. Contact of the skin and eyelashes with the eyeball may result in irritating symptoms, possible abrasion, scarring of the cornea, and even decreased visual acuity. The majority of patients with entropion present with acute or recurrent onset of symptoms of foreign body sensation, burning, laceration, and photophobia1.
There are four types of entropion reported: involutional or senile, congenital, spastic acute, and cicatricial2. Involutional is the most common type and most often affects the lower eyelids of the elderly1 (Figure 1). Its etiology is related to the following degenerative changes: 1) variable degrees of enophthalmos due to the absorption of orbital fat that reduces the pressure of the eyeball against the superior margin of the tarsus; 2) sagging structures supporting the tarsus, such as orbital septum, retractors, and aponeurosis of the lower oblique muscle; 3) migration and hyperactivity of the superior portion of the pre-septal orbicularis muscle over the pre-tarsal muscle and inferior tarsus3.
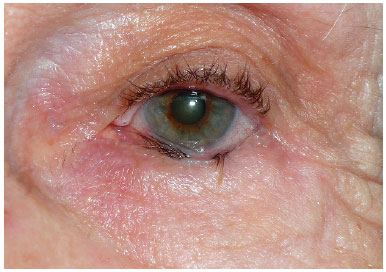
Figure 1. Patient with involutional entropion.
Surgery is the only effective and definitive treatment1. The use of sutures for the treatment of entropion dates back to the times of ancient Greece. However, the first published accounts were made by Snellen and Hotz in the nineteenth century. Currently, there are several techniques described for the treatment of entropion. In 1977, Lessa described a method for the surgical correction of involutional entropion, which consisted of a modified technique of Jones, Reeh, and Tsujimura4,5. In 2011, the author added to the technique described a support procedure for the lateral corner, which could be a canthoplasty or canthopexy3.
OBJECTIVE
This paper aims to present the author's experience with the technique described by Lessa in the surgical treatment of patients with involutional entropion, evaluating their efficacy.
METHODS
This is a clinical, uncontrolled, retrospective, descriptive, interventional study in which 13 lower eyelids were operated by the author in 11 patients with a diagnosis of involutional entropion in the Federal Hospital of Lagoa. The study began on January 2012 and ended on April 2013 and included patients with involutional entropion of the lower eyelids, of both sexes. Patient consent terms were provided prior to surgery, and the work followed the legal procedures in accordance with the principles of the Declaration of Helsinki.
The exclusion criteria are as follows: previous eyelid surgeries and pathologies that could simulate entropion, such as trichiasis, distichiasis, and epidermis. In the preoperative evaluation, the degree of horizontal flaccidity was evaluated by the snap-back test6, which evaluates the time the eyelid returns in contact with the eyeball when pulled down. The normal is the immediate return.
In patients with moderate lower palpebral flaccidity (slow return), muscle suppression was described by Mladick7. In those with severe palpebral flaccidity (very slow or absent return), chondroplasty was performed. In patients of large palpebral disproportions, the tarsal flap described by Anderson3,8,9 was indicated for fixation and shortening of the lower tarsus, whereas in patients who did not present with this disproportion, the tarsal suspension was chosen, and the lower tarsus was attached to the Whitnall tubercle without horizontal shortening of the palpebral margin.
The patients were placed in the dorsal decubitus position. The anesthesia used was sedation plus local infiltration with 1% lidocaine solution plus adrenaline in the ratio 1:100,000.
Description of the technique was as follows: 1) subciliary incision 2 mm from the palpebral margin, progressing up to approximately 3 mm from the tear point (Figures 2A and B); 2) dissection of a flap of skin, exposing the orbicularis muscle followed by resection of a band of this, approximately 3 mm wide, throughout the palpebral extension, precisely in the transition from the pre-tarsal portion to the pre-septal of the orbicularis muscle, leaving the orbital septum exposed (Figures 3A and B); 3) upper traction of the skin flap with excess tissue resection; 4) skin-septum-skin suture, with three silk sutures 6-0, observing the modification of the palpebral position (at this moment, it is important to check if there was no excessive eversion, avoiding the formation of an ectropion (Figures 4A and B); 5) muscle suspension canthopexy or lateral cankerplasty, depending on the previous evaluation with snap-back test6 (in the muscle suspension technique, the lateral end of the pre-tarsal orbicularis muscle is attached to the lateral periosteum of the orbit at a point slightly above the medial canthus, and in cases of cankerplasty, the tarsal flap or tarsal suspension is made); 6) cutaneous synthesis by continuous suture, using nylon 6-0, and placement of microporous tapes laterally to the corner, diagonally arranged (Figures 5A and B).
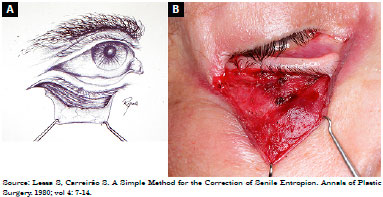
Figure 2. A: Subciliary incision and cutaneous detachment; B: Subciliary incision and cutaneous detachment.
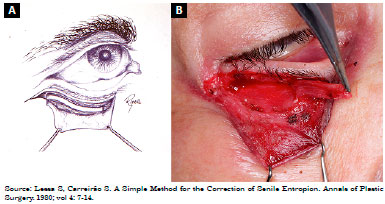
Figure 3. A: Resection of muscle band; B: Resection of muscle band.
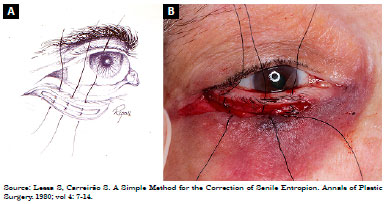
Figure 4. A: Skin-septum-skin suture; B: Skin-septum-skin suture.
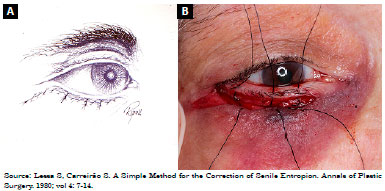
Figure 5. A: Skin synthesis; B: Skin synthesis.
In the postoperative period, ocular lubricant, analgesics, and cold compresses were prescribed on the eyelids. The patients were instructed to sleep with the headboard elevated, not to make physical effort and not to touch the bandage. The removal of sutures was done within 1 week and, in cases of canthoplasty, within 14 days, for the removal of lateral suture. The microporous tapes were changed within 1 week and stayed for another 7 days. The outpatient review was performed, within 1 and 2 weeks and 1, 3, 6, 12, and 18 months. Complications, recurrences, and improvement of ocular complaints were evaluated in all return visits.
RESULTS
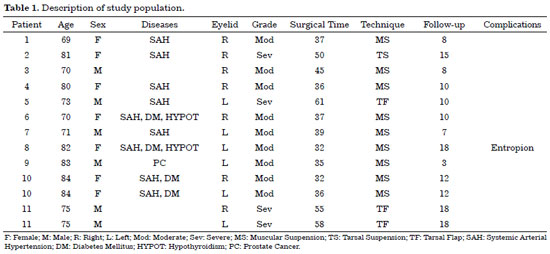
Eleven patients (5 men and 6 women) were operated, with a mean age of 76.72 years (69 to 84 years), totaling 13 eyelids. Two patients had both lower eyelids affected, while 5 had only the right and 4 had only the left. The comorbidities present are described in Table 1. The preoperative complaints were ocular irritation, pruritus, burning, and tearing.
All patients underwent entropion correction using the Lessa4 technique associated with some lateral support procedure. In eight patients (9 eyelids), muscle suspension was used; in one, tarsal suspension; and, in two (three eyelids), tarsal flap. The mean surgical time (per eyelid) of the patients submitted to muscle suspension was 36.55 min, while, in patients who underwent chondroplasty, it was 56 min. There were no intercurrences in the first 24 h.
In the first postoperative week, one patient, who underwent muscular suspension, presented an ectropion. As there was no improvement of the condition with local massages in 6 months, it was reoperated and submitted to ectropion correction with tarsal flap. The minimum time of outpatient follow-up was 3 months and the maximum 18 months. Table 1 shows the patients included in the study. Figures 6 to 8 show pre- and postoperative photographs of the three lateral support techniques used.
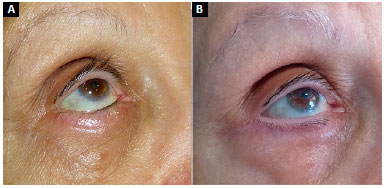
Figure 6. A: Muscle suspension; B: Muscle suspension.
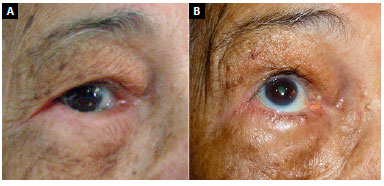
Figure 7. A: Tarsal suspension; B: Tarsal suspension.
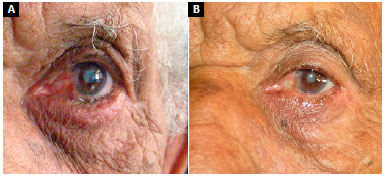
Figure 8. A: Tarsal flap; B: Tarsal flap.
DISCUSSION
The most common type of entropion is the involutional type that usually occurs in the elderly. Its cause is related to the reduction of the palpebral tone, devaluation, and superior deviation of the pre-septal orbicularis muscle over the pre-tarsal muscle and the disinsertion or weakening of the structures that support the tarsus.
Histologically, there is degeneration of the collagen and elastosis of the tarsal plaque with increased adipose tissue at the distal end of the tarsus, subacute inflammation, and keratinization of the tarsal conjunctiva, as well as focal degeneration, fibrosis, and elastosis of the pre-tarsal portion of the orbicularis muscle. Fragmentation of tarsal collagen and increased adipose tissue in the distal portion of the tarsus probably contribute to the development of age-related entropion10. Previous studies show the relation of histopathological findings to the development of involutional entropion. Alterations of collagen, elastic fibers, and increase of adipose tissue in the distal tarsus were observed11.
The main component of fibroconnective tissue in young adult tarsus is collagen fibers. With aging, there are significant changes of these fibers. In entropion, there is septal atrophy and thinning of the tarsus10.
Surgery is the only definitive treatment for entropion. Nonsurgical interventions, such as the administration of botulinum toxin12, eyelash epilation and the attachment of adhesive tapes, tracing the palpebral margin downward, constitute palliative and temporary treatments. CO2 laser was described as an alternative treatment for very elderly patients with comorbidities13.
Local anesthesia associated with sedation was chosen because it allows the surgeon to evaluate the effectiveness of the procedure intraoperatively. The cooperation of the patient in the ocular opening helps to show the eyelid position, avoiding an overcorrection or undercorrection. In addition, the use of local anesthesia with vasoconstrictor reduces local bleeding, allowing a better identification of anatomical structures. However, some authors prefer the use of general anesthesia because it offers greater patient immobility and better control of blood pressure14.
Historically, several surgical techniques have already been described for the treatment of involutional entropion; however, many have relapses, especially when used alone. Thus, it was verified that the combination of more than one technique decreases the incidence of relapses, since it treats more than one pathological alteration1. Ziegler described the vertical shortening of the skin and muscle; Fox, Schimek, and Bick worked on the horizontal fixation of the eyelid at the lower tarsal border; Wies, Jones, and Wheeler approached the fibers of the orbicularis muscle, while Jones worked on the fixation of the inferior retractors15.
The technique described by Lessa, which we used in this study, is an association of three techniques, where a more complete treatment of entropion is achieved, since it acts on the pre-septal orbicularis muscle on the pre-tarsal muscle, horizontal flaccidity, and structures which support the tarsus. The subciliary incision used in blepharoplasties is a modification of Jones et al.'s technique16,17, which uses a lower ciliary margin incision. The positioning of the scar parallel to the ciliary margin prevents eyelid edema that occurs when using low incisions3.
This technique is a relatively fast procedure and should always be associated with a lateral support technique. The meticulous preoperative physical examination, associated to the snap-back test, is of paramount importance for the correct choice of the cornerplasty or canthopexy. This reduces surgical time and is less aggressive because there is no sagging. However, it should be very well indicated and used only in cases in which there is no severe sagging, thus avoiding relapses.
In this study, there were no recurrences until the present moment. Among the complications, the most common is entropion recurrence, which can be diminished through the association of more than one technique and especially when it acts on each causal factor1. Using a technique alone, the rate of relapse is 14 to 31%, whereas, when there is an association of two techniques directed to the treatment of two causes, the index falls to 2 to 13%14.
Other complications reported in the literature are ectropion, hematoma, eyelid margin necrosis, loss of eyelashes, and infection1. In our study, the incidence of complications was 11.11% in the group of patients who underwent muscular corner joints, referring to a case of ectropion, identified in the first postoperative week. This complication may be justified by the undetermined preoperative assessment of the degree of sagging, where probably the use of cankerplasty might have provided a more successful outcome, or perhaps by excessive pulling of the lower eyelid during skin-septum-skin suturing. In the group submitted to canthoplasty, no complications were evident. Another author also refers to a case of ectropion, but it occurred 3 months after surgery17.
Thus, an adequate preoperative assessment associated with more than one technique focused on the causes of entropion undoubtedly increases the chances of having a successful procedure.
CONCLUSION
The procedure used in this study proved to be effective in the treatment of involutional entropion in our series and postoperative follow-up, since there were no cases of relapse.
The technique described by Lessa presents simplicity of execution and good reproducibility, requiring a short surgical time, with a low rate of complications.
COLLABORATIONS
RLCF Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
SL Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
REFERENCES
1. Kronish JW. Entrópio. In: Chen WP. Cirurgia Plástica Oftalmológica - Princípios e Prática. Rio de Janeiro: Revinter; 2005. p. 41-53.
2. Altieri M, Iester M, Harman F, Bertagno R, Capris P, Venzano D, et al. Comparison of three techniques for repair of involutional lower lid entropion: a three-year follow-up study. Ophthalmologica. 2003;217(4):265-72. PMID: 12792132 DOI: http://dx.doi.org/10.1159/000070633
3. Lessa S. Entrópio palpebral. In: Carreirão S, Carneiro Jr LV. Cirurgia Plástica para Formação do Especialista. Rio de Janeiro: Atheneu Rio; 2011. p. 431-4.
4. Lessa S, Carreirão S. A simple method for the correction of senile entropion. Ann Plast Surg. 1980;4(1):7-13. DOI: http://dx.doi.org/10.1097/00000637-198001000-00003
5. Jones LT, Reeh MJ, Tsujimura JK. Senile entropion. Am J Ophthalmol. 1963;55:463. DOI: http://dx.doi.org/10.1016/0002-9394(63)93537-2
6. Iyengar SS, Dresner SC. Entropion. In: Black EH, Nesi FA, Gladstone G, Levine MR, Calvano CJ, eds. Smith and Nesi's Ophthalmic Plastic and Reconstructive Surgery. 3rd ed. New York: Springer; 2012. p. 311-5.
7. Mladick RA. The muscle-suspension lower blepharoplasty. Plast Reconstr Surg. 1979;64(2):171-5. PMID: 451075 DOI: http://dx.doi.org/10.1097/00006534-197908000-00006
8. Anderson RL, Gordy DD. The tarsal strip procedure. Arch Ophthalmol. 1979;97(11):2192-6. DOI: http://dx.doi.org/10.1001/archopht.1979.01020020510021
9. Iliff NT. An easy approach to entropion surgery. Ann Ophthalmol. 1976;8(11):1343-6.
10. Kocaoglu FA, Katircioglu YA, Tok OY, Pulat H, Ornek F. The histopathology of involutional ectropion and entropion. Can J Ophthalmol. 2009;44(6):677-9. PMID: 20029486 DOI: http://dx.doi.org/10.3129/i09-152
11. Damasceno RW, Heindl LM, Hofmann-Rummelt C, Belfort R, Schlötzer-Schrehardt U, Kruse FE, et al. Pathogenesis of involutional ectropion and entropion: the involvement of matrix metalloproteinases in elastic fiber degradation. Orbit. 2011;30(3):132-9. DOI: http://dx.doi.org/10.3109/01676830.2011.569049
12. Deka A, Saikia SP. Botulinum toxin for lower lid entropion correction. Orbit. 2011;30(1):40-2. DOI: http://dx.doi.org/10.3109/01676830.2010.544443
13. Babuccu O. An alternative approach for involutional entropion: a preliminary study. Lasers Med Sci. 2012;27(5):1009-12. DOI: http://dx.doi.org/10.1007/s10103-011-1036-5
14. Morano FG, Amâncio Junior M, Brejon R, Esper CR, Farias JCM. Entrópio senil da pálpebra inferior: cirurgia baseada na etiopatogenia. Rev Bras Cir Plást. 2010;25(2):231-7.
15. Involutional Entropion and Ectropion. In: Codner MA, McCord CD Jr, eds. Eyelid & Periorbital Surgery. St. Louis: Quality Medical Publishing; 2008. p. 627-35.
16. Fox SA. Ophthalmic plastic surgery. 4th ed. New York: Grune & Stratton; 1970.
17. Nakauchi K, Mimura O. Combination of a modified Hotz procedure with the Jones procedure decreases the recurrence of involutional entropion. Clin Ophthalmol. 2012;6:1819-22. DOI: http://dx.doi.org/10.2147/OPTH.S36819
1. Hospital Federal da Lagoa, Rio de Janeiro, RJ, Brazil
2. Universidade Estadual do Rio de Janeiro, Rio de Janeiro, RJ, Brazil
Institution: Hospital Federal da Lagoa, Rio de Janeiro, RJ, Brazil.
Corresponding author:
Renata Lowndes Corrêa Francalacci
Rua Visconde de Pirajá, 623/803 - Ipanema
Rio de Janeiro, RJ, Brazil - Zip Code 22410-003
E-mail: renatafrancalacci@gmail.com
Article received: May 10, 2017.
Article accepted: September 23, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter