

Original Article - Year 2017 - Volume 32 -
Postoperative control of liposuction pain
Controle da dor no pós-operatório de lipoaspiração
ABSTRACT
INTRODUCTION: Pain control is essential in any surgical event. Liposuction is, in general, accompanied by complaints of post-operative pain, which raises the discussion about the best way to prevent and treat it. Accordingly, studies indicate that the analgesia should begin before any painful stimulus is triggered in order to reduce or prevent the pain preemptively. The approach of the various pain pathways, with a combination of different classes of drugs or utilization of spinal block or epidural/general anesthesia can also contribute to pain management.
METHODS: A descriptive, prospective, interventional cohort type study was conducted with patients undergoing plastic surgery involving liposuction. The standard anesthetic procedure consisted of an association between general and spinal anesthesia. The assessment of pain, carried out 6 and 18 hours after the end of the surgery, used unidimensional scales. The absence of pain or the presence of mild pain was considered a satisfactory result.
RESULTS: Fifty female patients were evaluated, with an average of 35 years of age. No intense pain was found at any time during the study. Satisfactory results accounted for 94% and 92% of the patients in the assessment at 6 and 18 hours post-surgery, respectively (p < 0.001).
CONCLUSIONS: Intravenous anesthesia combined with spinal anesthesia, in body contouring surgery, was able to satisfactorily control pain in the immediate postoperative period in most cases (>90%). In this study, liposuction was revealed to be a type of surgery with manageable pain.
Keywords: Analgesia; Lipectomy; General anesthesia; Spinal anesthesia; Pain, postoperative.
RESUMO
INTRODUÇÃO: O controle da dor é essencial em qualquer evento cirúrgico. A lipoaspiração cursa, em geral, com queixas de dor pós-operatória, o que levanta a discussão acerca da melhor maneira de preveni-la e tratá-la. Dessa forma, estudos indicam que a analgesia deveria começar antes que qualquer estímulo doloroso seja deflagrado a fim de reduzir ou prevenir a dor preemptivamente. A abordagem nas diversas vias álgicas, com combinação de diferentes classes de fármacos ou associação dos bloqueios raquimedular ou epidural com anestesia geral, também pode contribuir para o manejo da dor.
MÉTODOS: Estudo descritivo, prospectivo, intervencionista, tipo Coorte, com pacientes submetidas à cirurgia plástica envolvendo lipoaspiração. O procedimento anestésico padrão consistiu na associação de anestesia geral e subaracnóidea. O escalonamento da dor, realizado 6 e 18 horas após o término da cirurgia, utilizou escalas unidimensionais. A ausência de dor ou a presença de dor leve foram consideradas como resultado satisfatório.
RESULTADOS: Foram avaliadas 50 pacientes do sexo feminino, com média de 35 anos de idade. Não foi encontrada dor severa em qualquer momento do estudo. Os resultados satisfatórios representaram 94% e 92% das pacientes na avaliação das 6 e 18 horas do pós-operatório, respectivamente (p < 0,001).
CONCLUSÕES: A anestesia geral venosa combinada com raquianestesia, em cirurgia de contorno corporal, foi capaz de controlar satisfatoriamente a dor no pós-operatório imediato na maioria dos casos (>90%). A lipoaspiração mostrou ser cirurgia de dor controlável nesta casuística.
Palavras-chave: Analgesia; Lipectomia; Anestesia geral; Raquianestesia; Dor pós-operatória.
Postoperative pain control is an essential part of any surgical procedure. Liposuction alone or in association with other surgeries, such as abdominoplasty or breast prostheses, is usually associated with common complaints of pain in clinical practice. In the case of body contouring surgery, patients frequently fear the procedure because of previous reports of high levels of pain1.
Liposuction, the most common aesthetic intervention in Brazil, has also been recognized as the procedure most associated with persistence of intense postoperative pain2. Inadequate pain management can lead to cardiovascular, respiratory, gastrointestinal, urinary, neuroendocrine, metabolic, and psychological changes. Effective pain control, on the other hand, is able to significantly reduce patient morbidity and mortality, as it provides physical and psychological comfort, inhibits nociceptive reflexes, and allows adequate breathing and early mobilization3.
Several studies, such as that of Garcia et al.4, indicate that the correct analgesia should begin even before any painful stimulus is triggered. Thus, there would be a reduction or prevention of pain following a preemptive approach. Another way to manage post-operative pain is an approach through the various pain pathways, either through the combination of different techniques, or the association of spinal or epidural blocks with general anesthesia5.
This association of anesthetic techniques may benefit the patient. The combination of general anesthesia and spinal anesthesia in liposuction is herein proposed. Such a combination can reduce the intensity of postoperative pain, providing safety by keeping the airway protected upon intubation and also comfort by allowing controlled hypnosis6. It is thus mandatory to evaluate the strategies for the prevention and treatment of post-operative pain after liposuction.
OBJECTIVE
As there is a scarcity of studies that evaluate postoperative pain in plastic surgery and liposuction, the objective of the present study was to evaluate the postoperative pain control in liposuction specifically with patients operated under general anesthesia combined with spinal anesthesia.
METHODS
A descriptive, prospective, interventional cohort type study, developed at the Hospital São Lucas in Aracaju, SE, was conducted in order to assess the level of pain in the immediate postoperative period in 50 patients subjected to body contouring plastic surgery between June 30, 2011 and November 30, 2013.
The study was approved by the Research Ethics Committee, according to Brazilian National Health Council (CNS) Resolution 196/96. The participants, after being informed and instructed on the actions to be performed, signed an Informed Consent Form (ICF) after oral and written clarifications.
Inclusion Criteria
• Female;
• Age range between 18 and 60 years;
• Indication for body contouring plastic surgery involving liposuction.
Criteria for non-inclusion
• Chronic Diseases - hypertension, diabetes mellitus, or other associated conditions;
• Smokers or ex-smokers for less than one year;
• Patients with cognitive dysfunction or psychiatric illness;
• Patients who did not sign the informed consent form.
Exclusion Criteria
• Patients who chose to leave the study.
All patients were submitted to the same anesthetic standard procedure: total venous general anesthesia associated with spinal block, noninvasive blood pressure monitoring, central temperature (nasopharyngeal assessment) monitoring, continuous pulse oximetry, cardioscopy, and capnography.
The standard anesthetic procedure consisted of: pre-anesthetic medication (midazolam 15 mg, oral); spinal anesthesia through puncture located at L3-L4 and blockade with hyperbaric bupivacaine 10 mg, fentanyl 20 mcg and morphine 80 mg; then, general anesthesia with lidocaine 1 mg/kg, propofol 1-3 mcg/ml, remifentanil 0.05-0.3 mcg/kg/min, fentanyl 2-4 mcg/kg, cisatracurium 0.1 mg / kg. Postoperative analgesia consisted of 2 g 6/6h (EV) sodium dipyrone, ketoprofen 100 mg 8/8h (EV), morphine 2 mg 4/4h (EV) and SOS (2 ml every 15 minutes, maximum of 3 doses).
All patients were operated on by the same surgical team and subjected to the super wet liposuction technique - a technique that was recognized and endorsed in the scientific field, besides being routinely performed in body contour plastic surgeries.
All patients followed the safety protocol:
• Surgeries were performed in a tertiary hospital with an intensive care unit (ICU);
• Prevention of hypothermia was done with the use of thermal blanket, infiltration of warm solutions and monitoring by means of nasopharyngeal thermometer (temperature > 35.6º C);
• Prevention of thromboembolism was done by pneumatic compression and compression stockings, in addition to the use of enoxaparin (40 mg, subcutaneously once a day) until 10 days after the surgery, respiratory and motor physiotherapy;
• Clarification of the procedures, their risks and complications, was done in consultation as well as in printed informational text;
• ICF was completed;
• The rates of abandonment, withdrawal, or exclusion of patients from this study were compiled in another protocol for further evaluation.
The data were obtained through the completion of the clinical visit protocol, from patients' anamnesis, and physical examinations performed 6 and 18 hours post-surgery.
Protocol for the assessment of pain
The visual analogue scale (VAS) and the numerical scale (Figures 1 and 2) were used for the quantitative evaluation of pain. Patients were questioned six and 18 hours post-surgery:

Figure 1. Sir Harold Gillies (right, sitting in the surgical room, Queen's Hospital, Sidcup (courtesy of Dr. Andrew Bamji, Gillies Archivist, BAPRAS).
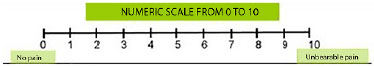
Figure 2. Plastic surgery Surgical Room, Queen's Hospital, Sidcup (courtesy of Dr. Andrew Bamji, Gillies Archivist, BAPRAS).
• 0 - No pain
• 1 to 3 - Mild pain
• 4 to 7 - Moderate pain
• 8 to 10 - Intense pain
The results were interpreted as either:
• Satisfactory: absence of pain or mild pain (score 0-3)
• Unsatisfactory: moderate to intense pain (score 4-10)
A descriptive analysis was performed using the absolute and relative frequencies for categorical variables, and central tendency measures and variability for numerical variables. Inferential analysis was performed using the 95% confidence intervals. As the variables studied were categorical, a statistical analysis of these results was carried out by the chi-square association test, with a significance level of 5%. The statistical programs SPSS version 22.0.0 (Windows) and R version 3.0.2 (Windows) were used for the analysis of the data.
RESULTS
Fifty patients who would undergo liposuction were prospectively evaluated. All of them were female. The patients' age ranged from 24 to 54 years, with a mean age of 35 years (95% CI: 33-38 years).
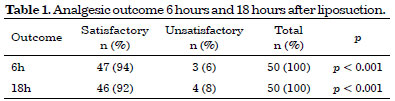
With regard to the level of postoperative pain, no intense pain was found throughout the study at any moment of pain assessment. Satisfactory results (score of 0-3) represented 94% (47/50) of the patients in the evaluation performed six hours post-surgery (p < 0.001). In the 18-hour evaluation, a satisfactory result was observed in 92% (46/50) of the cases (p < 0.001) (Table 1).
Two pain assessments were performed with each patient included in the study, for a total of 100 pain assessments. These assessments were performed 6 and 18 hours postoperatively. A total of 14% (14/100) presented mild pain and only 7% (7/100) reported moderate pain (Table 2).
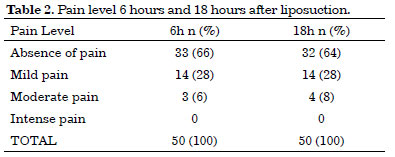
The highest intensity indicated in the scales was 5 points. However, a mean score of 0.78 (95% CI: 0.43 to 1.13) at six hours post-surgery and 0.92 (95% CI: 0.52 to 1.32) at 18 hours post-surgery were recorded (p = 0.424).
DISCUSSION
Pain is a frequently observed phenomenon after surgery, and liposuction is cited as one of the aesthetic interventions most associated with the persistence of postoperative pain. The effects of acute pain on the body cause diverse changes, which can and should be avoided by appropriate analgesia so as not to cause unnecessary suffering and risks to the patient2,7. However, there is still a scarcity of scientific studies on pain in plastic surgery.
The anesthetic plan in liposuction has an important role. The choice of anesthetic should ensure patient safety and comfort in the management of pain. The literature reports that liposuction can be performed under four anesthetic techniques: local anesthesia with or without sedation, regional anesthesia (epidural anesthesia or spinal anesthesia) with or without sedation, and general anesthesia. Each technique has advantages and limitations. The choice of the best technique should take into account the characteristics of the patient, the length and duration of the surgery, and the preference and experience of both the surgeon and anesthesiologist8.
Although epidural anesthesia is widely used in liposuction and has higher analgesic quality compared to local anesthesia, extensive epidural block is often associated with hypotension and should be limited to patients with good cardiac reserve9. On the other hand, the use of opioids in the subarachnoid space, in spinal anesthesia, provides the benefit of good analgesia in the first 24 hours postoperatively, in addition to anesthesia and quality muscle relaxation8 with safety.
General anesthesia is recommended for high-volume liposuction because it ensures rapid patient recovery using propofol10 and maintains a protected airway through orotracheal intubation. However, analgesia only lasts a short duration due to the characteristics of the opioids used, such as fentanyl or remifentanil8. It is nevertheless an option when there is a need for a change in position, which is common in liposuction. This, however, predisposes to greater respiratory and hemodynamic changes due to high blockade and prolonged sedation.
With the understanding of the pathophysiology of acute pain, the difficulty of using a single drug or intervention broad enough in its action in order to be properly effective was recognized. This limitation becomes more evident with moderate or intense pain11 and persistence of unwanted pain levels in the postoperative period.
Thus, in controlling pain, it is important to use multiple anesthetic drugs or procedures; this is the multimodal approach. The association of analgesic drugs with different mechanisms of action allows one to use lower doses to obtain good pain control with minimal adverse effects. The synergistic effect of these drugs produces more efficient analgesia by addressing the pain through all its mechanisms, aside from reducing the adverse effects due to the possibility of reducing the dose or changing the analgesic11.
With this perspective, the technique used in this study, which was general anesthesia combined with subarachnoid blockade allowed the use of lower doses of local anesthetics with a reduction of side effects12. Safety was also noted by keeping the airway protected and patient comfort was provided by allowing a controlled hypnosis plan, which avoided unnecessary arousal during the surgery. In addition, it significantly reduced the intensity of postoperative pain5, as demonstrated in the present study, with satisfactory results (> 90%) in relation to pain as well as the absence of major ventilatory or hemodynamic changes in 50 patients.
The wide variation in pain sensitivity among individuals or even with the same patient varies at different time points13. This phenomenon makes it difficult to conduct pain assessment studies. To address this, pain ratings were recorded systematically, by protocol and using specific scales for the characterization and measurement of pain. The results would subsequently contribute to the improvement in the management of painful symptoms6,14. This study used the numeric visual scale and the visual analogue scale, since these unidimensional scales are the most common in surgical procedures15.
The age of the patients ranged between 24 and 54 years of age, with an average of 35 years (95% CI: 33 to 38 years), in line with epidemiological data concerning patients who seek the aesthetic surgery service2,16.
The selection of the sample for this study comprised only female patients. This is due to the influence of gender on the prevalence of pain17,18 and also due to the fact that liposuction is mostly performed in women2,19. In addition, it has been demonstrated that women complain more about pain and have a longer recovery than men after liposuction, with similar final results20.
Two pain assessments were performed at six and 18 hours after liposuction for each patient included in the study, resulting to 100 pain assessments. 14% (14/100) presented mild pain and only 7% (7 / 100) moderate pain. There were no reports of strong or intense pain, scores of 6 and 8, respectively, on the pain assessment scales, in contrast to published data1.
It is worth mentioning that, in the study of Santos et al.1, the majority of patients underwent liposuction with or without breast implant placement under epidural anesthesia associated with sedation. From this perspective, general anesthesia associated with subarachnoid block was shown to be an excellent anesthetic choice for pain management in liposuction compared with epidural block.
The advantage of subarachnoid anesthesia is its ability to provide good analgesia in the first 24 hours post-surgery8. This can be seen upon assessment of pain levels in patients at six and 18 hours after the surgical procedure, since the results were satisfactory (score 0-3) in 94% (47/50) and 92% (46/50) of the cases, respectively, indicating the analgesia was appropriate in the majority of the patients examined in the immediate postoperative period of liposuction.
Such data supersedes the information found in the work of Silva and Moraes2, in which more than 18% of the cases presented unsatisfactory results (score 4-10). However, their sample was composed of different types of aesthetic plastic surgery including not only liposuction, but also abdominoplasty, rhinoplasty, and breast prosthesis. Furthermore, there is no description of the anesthetic strategy drawn during the perioperative period.
The present study demonstrated that general anesthesia associated with spinal anesthesia was effective and safe in handling pain during the immediate postoperative period of liposuction.
CONCLUSION
Pain can be satisfactorily and safely controlled during the immediate postoperative period of liposuction through the institution of the proposed protocol of general anesthesia combined with spinal block. This protocol can also be used as an option for other types of plastic surgery.
COLLABORATIONS
MVAM Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
PTA Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; writing the manuscript or critical review of its contents.
RSR Analysis and/or interpretation of data; conception and design of the study; writing the manuscript or critical review of its contents.
LAGD Conception and design of the study; completion of surgeries and/or experiments.
JSP Conception and design of the study; completion of surgeries and/or experiments.
FVA Conception and design of the study; completion of surgeries and/or experiments.
JGQ Statistical analyses.
REFERENCES
1. Santos NP, Barnabé AS, Fornari JV, Ferraz RRN. Avaliação do nível de dor em pacientes submetidos a cirurgias plásticas estéticas ou reparadoras. Rev Bras Cir Plást. 2012;27(2):190-4. DOI: http://dx.doi.org/10.1590/S1983-51752012000200004
2. Silva AP, Moraes MW. Incidência de dor no pós-operatório de cirurgia plástica estética. Rev Dor. 2010;11(2):136-9.
3. Azevedo MP, Nunes BC, Pereira ACMP. Dor aguda. In: Cavalcanti IL, Maddalena ML, ed. Dor. Rio de Janeiro: SAERJ; 2003. p. 95-166.
4. Garcia JBS, Issy AM, Sakata RK. Analgesia preemptiva. Rev Bras Anestesiol. 2001;51(5):448-63. DOI: http://dx.doi.org/10.1590/S0034-70942001000500011
5. Kaufman E, Epstein JB, Gorsky M, Jackson DL, Kadari A. Preemptive analgesia and local anesthesia as a supplement to general anesthesia: a review. Anesth Prog. 2005;52(1):29-38. PMID: 15859447 DOI: http://dx.doi.org/10.2344/0003-3006(2005)52[29:PAALAA]2.0.CO;2
6. Moreira L, Truppel YM, Kozovits FGP, Santos VA, Atet V. Analgesia no pós-cirúrgico: panorama do controle da dor. Rev Dor. 2013;14(2):106-10. DOI: http://dx.doi.org/10.1590/S1806-00132013000200006
7. Pimenta CAM, Santos EMM, Chaves LD, Martins LM, Gutierrez BAO. Controle da dor no pós-operatório. Rev Esc Enferm USP. 2009;35(2):180-3. DOI: http://dx.doi.org/10.1590/S0080-62342001000200013
8. Regatieri FL, Mosquera MS. Liposuction anesthesia techniques. Clin Plast Surg. 2006;33(1):27-37. DOI: http://dx.doi.org/10.1016/j.cps.2005.08.003
9. Knize DM, Fishell R. Use of preoperative subcutaneous "wetting solution" and epidural block anesthesia for liposuction in the office-based surgical suite. Plast Reconstr Surg. 1997;100(7):1867-74. PMID: 9393487 DOI: http://dx.doi.org/10.1097/00006534-199712000-00035
10. Geerts WH, Bergqvist D, Pineo GF, Heit JA, Samama CM, Lassen MR, et al. Prevention of venous thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133(6 Suppl):381S-453S. DOI: http://dx.doi.org/10.1378/chest.08-0656
11. Chandrakantan A, Glass PS. Multimodal therapies for postoperative nausea and vomiting, and pain. Br J Anaesth. 2011;107 Suppl 1:i27-40 DOI: http://dx.doi.org/10.1093/bja/aer358
12. Buvanendran A, Kroin JS. Multimodal analgesia for controlling acute postoperative pain. Curr Opin Anaesthesiol. 2009;22(5):588-93. DOI: http://dx.doi.org/10.1097/ACO.0b013e328330373a
13. Danilla S, Fontbona M, de Valdés VD, Dagnino B, Sorolla JP, Israel G, et al. Analgesic efficacy of lidocaine for suction-assisted lipectomy with tumescent technique under general anesthesia: a randomized, double-masked, controlled trial. Plast Reconstr Surg. 2013;132(2):327-32. PMID: 23897332 DOI: http://dx.doi.org/10.1097/PRS.0b013e3182958b20
14. Ready LB, Edwards WT. Tratamento da dor aguda. Rio de Janeiro: Revinter; 1997.
15. Pedroso RA, Celich KLS. Dor: quinto sinal vital, um desafio para o cuidar em enfermagem. Texto Contexto Enferm. 2006;15(2):270-6. DOI: http://dx.doi.org/10.1590/S0104-07072006000200011
16. Cárdenas-Camarena L. Lipoaspiration and its complications: a safe operation. Plast Reconstr Surg. 2003;112(5):1435-41. DOI: http://dx.doi.org/10.1097/01.PRS.0000081469.07342.F2
17. Uchiyama K, Kawai M, Tani M, Ueno M, Hama T, Yamaue H. Gender differences in postoperative pain after laparoscopic cholecystectomy. Surg Endosc. 2006;20(3):448-51. DOI: http://dx.doi.org/10.1007/s00464-005-0406-0
18. Ochroch EA, Gottschalk A, Troxel AB, Farrar JT. Women suffer more short and long-term pain than men after major thoracotomy. Clin J Pain. 2006;22(5):491-8. DOI: http://dx.doi.org/10.1097/01.ajp.0000208246.18251.f2
19. Martinez MAR, Okajima RMO, Proto RS, Lourenço LM, Machado Filho CDS. Estudo de 543 pacientes submetidos à lipoaspiração tumescente. Surg Cosmet Dermatol. 2010;2(3):155-8.
20. Swanson E. Prospective outcome study of 360 patients treated with liposuction, lipoabdominoplasty, and abdominoplasty. Plast Reconstr Surg. 2012;129(4):965-78. PMID: 22183499 DOI: http://dx.doi.org/10.1097/PRS.0b013e318244237f
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. International Society of Aesthetic Plastic Surgery, Hanover, NH, EUA
3. Liga Acadêmica de Cirurgia Plástica de Sergipe, Aracaju, SE, Brazil
4. Universidade Federal de Sergipe, Aracaju, SE, Brazil
5. Hospital do Servidor Público Estadual, Aracaju, SE, Brazil
6. Sociedade Brasileira de Anestesiologia, Rio de Janeiro, RJ, Brazil
7. Hospital São Lucas, Aracaju, SE, Brazil
Institution: Universidade Federal de Sergipe, Aracaju, SE, Brazil.
Corresponding author:
Marcel Vinicius de Aguiar Menezes
Avenida Beira Mar, 280
Aracaju, SE, Brazil - Zip Code 49020-010
E-mail: mviniciusmed@yahoo.com.br
Article received: June 19, 2014.
Article accepted: August 17, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter