

Reviw Article - Year 2017 - Volume 32 -
Psychiatric disorders in aesthetic medicine: the importance of recognizing signs and symptoms
Transtornos psiquiátricos na medicina estética: a importância do reconhecimento de sinais e sintomas
ABSTRACT
Psychiatric disorders are widely reported in patients seeking aesthetic treatments. Although they are not necessarily a contraindication for procedures, the recognition of these symptoms by the professional tends to strengthen the professional-patient relationship, thus leading to a better prognosis. This reduces the chances of dissatisfaction, complications, and aggravation of psychiatric symptoms, in addition to avoiding legal complications. In this article, the most common psychiatric disorders arising in cosmetic and aesthetic treatment are presented and discussed, as well as guidelines for recognizing the symptoms and managing these patients.
Keywords: Aesthetics; Plastic surgery; Psychiatry; Mental health; Body dysmorphic disorders.
RESUMO
Transtornos psiquiátricos são amplamente evidenciados em pacientes que buscam tratamentos estéticos. Apesar de não configurarem necessariamente uma contraindicação para a realização de procedimentos, o reconhecimento desses sintomas pelo profissional tende a contribuir para o fortalecimento da relação profissional-paciente e para um melhor prognóstico, reduzindo as chances de insatisfação, complicações e agravos nos sintomas psiquiátricos, além de evitar complicações legais. No presente artigo, os transtornos psiquiátricos mais comuns no domínio cosmético e estético foram apresentados e discutidos, assim como as orientações para o reconhecimento de sintomas e de manuseio destes pacientes por profissionais de saúde.
Palavras-chave: Estética; Cirurgia plástica; Psiquiatria; Saúde mental; Transtornos dismórficos corporais.
According to the International Society for Aesthetic Plastic Surgery1, in 2013 Brazil was the country in which the most plastic surgeries were carried out, and was second only to the United States in the number of non-surgical cosmetic procedures. Various demographic, social, and psychological factors have been proposed as predictors of desire for aesthetic procedures; however, these factors might vary according to the procedure, culture, and religion of a society2. Studies have found that the main reason for patients to request aesthetic procedures is a hope of becoming more satisfied with their appearance and improving their psychosocial functioning3.
Technological developments in the aesthetic field have provided the possibility of carrying out an even wider range of procedures. Modern aesthetic procedures, both surgical and minimally invasive, allow the treatment of various body dysmorphic and aesthetic dysfunctions, such as acne, stretch marks, cellulitis, localized fat, and scars, among others4.
Moreover, aesthetic medicine also interacts with post-surgical rehabilitation, which is often essential for the recovery of individuals in postoperative stages. Therefore, the development of aesthetic medicine provides not only reconstruction of the body image but also rehabilitation and promotion of physical, mental, and social health.
In the context of mental health, it is known that the aesthetic dysfunctions are associated with several psychiatric disorders, such as depression, anxiety, and post-traumatic stress disorders, by damaging self-esteem and quality of life5. It seems clear that a successful aesthetic procedure could lead to fundamental emotional improvements, such as self-image enhancement and higher self-esteem, consequently affecting the quality of life and mental health3.
Thus, several studies have demonstrated improvement in the psychosocial functioning of subjects who underwent aesthetic treatments4,6. On the other hand, patient failure or dissatisfaction after an aesthetic procedure could lead to a worsening of symptoms, especially when the patient already has a history or current diagnosis of certain psychiatric disorders7.
Studies show that about 50% of individuals seeking aesthetic treatments fulfill the diagnostic criteria for psychiatric disorders, mainly associated with body image disorders8. A study carried out in 2011 found that 21-59% of the patients who underwent aesthetic surgeries presented higher scores regarding physical dissatisfaction and symptoms of psychiatric disorders than members of the general population9.
According to Ritvo et al.7, although such disorders are common, the aesthetic treatment of this population can be very challenging, especially because, in many cases, the patients are obsessed with body image and not satisfied with the results of the procedures. Therefore, familiarization with and recognition of the signs and symptoms of psychiatric disorders can be very important for professionals in the aesthetic field, to avoid having patients undergo unsatisfactory procedures, and (in the context of the growing importance of medical-legal disputes) to avoid lawsuits. Taking these aspects into account, the present article aims to describe the most common psychiatric disorders in the aesthetic domain, and to guide professionals in the recognition of the signs and symptoms of psychiatric disorders and the management of patients with these disorders.
OBSESSIVE-COMPULSIVE DISORDERS (OCD)
Body Dysmorphic Disorder
Body dysmorphic disorder (BDD) is a psychiatric disorder included within the category of obsessive-compulsive disorders, characterized by the individual's exaggerated concern with appearance. In this sense, BBD is mainly characterized by excessive preoccupation with one or more defects or failures in physical appearance that are not observable by third parties, or only slightly visible. This distortion in perception generates intrusive thoughts and repetitive behavior, difficult to control, that can last 3 to 8 hours a day, causing intense distress and damaging multiple aspects of life.
However, it is important that a professional knows how to differentiate BDD from anorexia and bulimia. While in those disorders the concern is with the size or shape of the body , BDD refers to one or more specific body parts, such as the nose, mouth, chin, breasts, head, hair, legs, or hips10.
Studies have found that the prevalence of BDD in the general population ranges from 1-3%11. On the other hand, despite the low prevalence in the general population, the prevalence of BDD in subjects seeking dermatological treatment or plastic surgery can vary from 5 to 15%12, reaching more than 50% in some populations13. Owing to this high prevalence, BDD is the most extensively studied psychiatric disorder in the literature on aesthetic procedures.
Evidence suggests that patients with higher levels of BDD symptoms are less satisfied with the results of aesthetic surgeries, and present higher levels of psychological symptoms and lower levels of self-esteem than patients with less expressive BDD9. Similarly, other studies have shown that the more extensive the symptoms of the disorder, the greater the dissatisfaction of the patient after a procedure14.
Thus, some studies have concluded that carrying out aesthetic procedures in this population, besides not generally improving BDD symptoms15,16, might actually result in exacerbation of the symptoms17, or in the appearance of other exaggerated body concerns18. In addition, studies have reported that rhinoplasty is the most prevalent aesthetic procedure among patients with BDD, mainly owing to the central position of the nose in the face19,20.
EATING DISORDERS
Anorexia Nervosa and Bulimia nervosa
Anorexia nervosa is a serious and complex eating disorder, in which people seek excessive weight loss, leading to extreme thinness. This disorder mainly affects women, resulting in body weight significantly lower than the healthy minimum. Three fundamental characteristics are evidenced in this disorder: persistent restriction in caloric intake, intense fear of gaining weight, and disturbance in self-perception of body weight or shape10.
Anorexia nervosa can be sub-classified into two different forms: a binge eating/purging type of anorexia, or a restrictive type of anorexia. The first is characterized by recurrent episodes of binge eating followed by purging behaviors (auto-induced vomiting, use of laxatives, etc.); the second by weight loss due to dietary restriction, with no alternation of binge eating and purgative behaviors10.
Bulimia nervosa is also considered an eating disorder, characterized by recurrent episodes of uncontrolled binge eating, in which excessive food intake occurs in a short period of time (usually less than 2 hours, with episodes at least once a week) and by a lack of self-control over food consumption. These episodes are accompanied by recurrent inappropriate compensatory behaviors (purging) that aim to prevent weight gain. It is important to point out that the binging and purging usually occur discretely10.
Although both anorexia and bulimia are related to the fear of gaining weight, the symptoms are different. In anorexia nervosa, the weight loss is severe, and usually leaves the person malnourished; in contrast, bulimics generally maintain a normal body weight. Nevertheless, it is estimated that in 10% to 15% of cases, bulimia can evolve into anorexia nervosa; it is also possible for these two syndromes to appear in alternation10.
Despite the importance of eating disorders, few studies have examined the psychological ramifications of performing aesthetic procedures in people with eating disorders. In this sense, it is important to note that eating disorders might be of particular concern for patients interested in body contouring procedures. A study carried out by Jávo et al.21 showed that women with eating problems are more interested in aesthetic procedures than female controls. In addition, the authors found that interest in liposuction was twice as high in this population as in women without eating disorders, and was reported by 52% of participants with eating problems21.
Some studies have reported cases of women with anorexia and bulimia who had previously undergone facial or body procedures, suggesting that these procedures might lead to exacerbation of eating symptoms22. However, the data are contradictory, since other studies reported that procedures such as breast implants, liposuction, and abdominoplasty reduce the risk of developing an eating disorder, as well as improving body image and self-esteem23-25. According to Veer et al.26, it is possible that, even though most patients with eating disorders are satisfied with the initial results of an aesthetic procedure, it usually leads to few changes to the body image and to the subsequent quality of life.
PERSONALITY DISORDERS
It is important to note that, regardless of the area of specialization, personality-related factors can interfere with any doctor-patient relationship27. This is because personality affects essential behaviors, such as seeking help, treatment adherence, coping styles, decision making, lifestyle, and social support choices, among other elements that can undermine the prognosis and treatment of physical and mental diseases.
In addition, evidence suggests that the probability of being a "patient with a problematic medical relationship" is high in individuals with personality disorders28. In a literature review on psychosocial outcomes for patients seeking aesthetic surgery, Honigman et al.29 found that having a personality disorder is one of the main risk factors associated with a poor prognosis.
Narcissistic Personality Disorder
Narcissistic personality disorder is characterized by a pervasive pattern of grandiosity, need for admiration, and lack of empathy, beginning in adulthood and present across a range of contexts. Narcissistic individuals are characterized by unrealistic fantasies of success, a sense of uniqueness, hypersensitivity to evaluation by others, feelings of authority, and expectations of special treatment10.
A recent study evaluated personality-associated characteristics in individuals seeking rhinoplasty in Iran, and found that approximately 26.7% of the individuals had narcissistic personality traits30. According to Veer et al.26, perfectionist and narcissistic patients often point out almost imperceptible imperfections in their appearance, and might have an increased chance of being disappointed with any level of asymmetry, or appearance of surgical scars or stains, following a procedure.
Histrionic Personality Disorder
This disorder is characterized by a pattern of excessive emotionality and a need to call attention to oneself, including approval-seeking and inappropriately seductive behavior, usually dating from the beginning of adulthood. These individuals are vivid, dramatic, animated, and flirtatious, and alternate their states between enthusiasm and pessimism10.
Patients with histrionic personality disorder are usually emotional, and tend to focus on personal appearance rather than on procedures. It is common for these patients to seek aesthetic treatment after a disappointment, such as the end of a relationship or loss of a job. Patients with this type of psychiatric disorder must be monitored closely after a procedure, since they tend to focus on the smallest details. The success of a cosmetic procedure consistently leads to stabilization of the psychiatric symptoms. However, there is a high probability that the patient will become depressed if he or she does not like the results31.
Borderline Personality Disorder
According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), Borderline Personality Disorder (BPD) is characterized by an inflexible pattern of emotional instability and by affective dysregulation, producing an emotional polarization that interferes with interpersonal relationships, self-image, and affects, consequently leading to impulsive or startling behaviors10.
The intensity of the emotional variability evidenced in this disorder, in particular the prevalence of love-hate relationships, generates anguish, feelings of abandonment, and perception of invasion of the ego, which often generates impulsive behavior, chronic feelings of emptiness, and dysfunctional reactions to stress, sometimes leading in turn to threats of (or attempts at) suicide, or self-mutilation. The onset of the disorder can occur in adolescence or adulthood, and the use of medical and mental health resources by these patients is significant.
A retrospective study carried out by Groenman and Sauër32 found that the most insatiable plastic surgery patients-those who were considered addicted to plastic surgeries-showed diagnostic criteria for BPD. Some articles have reported that individuals with BPD usually have a low degree of satisfaction with the results of surgeries and aesthetic procedures33,34. Moreover, in a systematic review of psychiatric disorders in patients undergoing aesthetic surgeries, BPD was described as a risk factor for the worsening of psychosocial prognoses29.
A recent review study showed that individuals with BPD tend to request corrections of various parts of the body for two main reasons: 1) to avoid abandonment by the surgeon, and 2) impulsiveness. In such cases the concern with appearance is superficial, and can change focus from one part of the body to another over time35.
It is important for us to know that individuals with BPD often express anger, or difficulty controlling anger, which are usually directed at family or friends, but can be directed to the professional or team members in cases where they are disappointed with the behavior of the professional or with the result of the procedure, and could result in acts of violence33,36,37.
Consequently, these individuals may not return for follow-up consultation, and will often change professionals. It is also possible that more impulsive individuals present behaviors of self-mutilation, as reported in a case study of a patient with BPD who self-mutilated as a response to the refusal of his surgeon to perform a new aesthetic surgery35.
INVESTIGATION OF SIGNS AND SYMPTOMS BY HEALTHCARE PROFESSIONALS
To avoid possible complications that may result from performing aesthetic procedures in patients with psychiatric disorders, it is important that healthcare professionals recognize the signs and symptoms of each disorder. Therefore, it is extremely important that the medical history be taken in detail, addressing questions about the history of previous procedures, history of psychiatric disorders, and other factors that we will cover below.
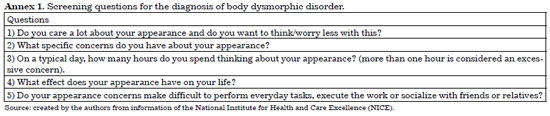
Responding to the high prevalence of BDD among aesthetic patients, the National Institute for Health and Care Excellence (NICE) proposed five questions that may aid in the diagnosis of BDD, presented in annex 1. The NICE guidelines clearly state that all patients with suspected or confirmed BDD diagnosis should be referred to a psychiatrist before any procedure or surgery is performed. However, it is important to note that, even after having received the opinion of a psychiatric specialist, the decision to perform the procedure should be taken by the professional.
Regarding eating disorders, anorexia nervosa has three essential characteristics: persistent restriction of caloric intake; intense fear of gaining weight or getting fat or persistent behavior that interferes with weight gain; and disturbance in the perception of their own weight or shape. The individual maintains a physical weight below what is minimally normal for age, gender, development, and physical health.
Bulimia nervosa is also characterized by three central features: recurrent episodes of binge eating[1] (Criterion A); recurrent inappropriate compensatory behaviors to prevent weight gain (Criterion B); and self-assessment unduly influenced by shape and body weight (Criterion D). To qualify for the diagnosis, binge eating and inappropriate compensatory behaviors should occur on average at least once a week for three months (Criterion C)10.
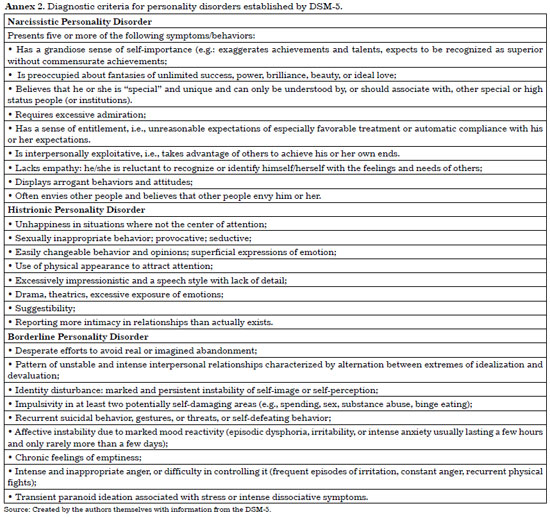
Annex 2 presents the diagnostic criteria established by the DSM-5 for each of the personality disorders previously discussed. Professionals should be alert for these signs and symptoms, to identify patients with a possible diagnosis of personality disorder.
DISCUSSION
Recently, a study evaluated the association between mental health problems and the postoperative results of cosmetic surgeries, within 30 days after the procedure. The authors observed that patients with psychiatric disorders more frequently required hospital care within this time period than those without mental health diagnoses (11.1% vs. 3.6%; adjusted odds ratio [AOR]: 1.78 [95% confidence interval, 1.59- 1.99])38.
Moreover, they found that the cost of post-surgery care for patients who needed care within 30 days after the initial procedure was, on average, 35,637 dollars38. Thus, in addition to the problems arising from dissatisfaction with the treatment, the higher prevalence of post-surgical complications associated with patients with psychiatric disorders can lead to high costs for both the professional and the client.
It is highly recommended that healthcare professionals refer patients who present signs and symptoms of psychiatric disorders to a specialist (psychiatrist, psychologist), who is requested to decide whether to authorize them to perform the procedure. Even with the authorization of a psychiatrist, it is up to the professional responsible for performing the aesthetic procedure to decide on its realization individually for each patient.
If the professional decides to conduct the procedure, among the main precautions raised in the literature is the use of an Informed Consent Form, containing before-and-after documentation through photographs and images, rigorous post-procedure treatment advice, and, more important than any of these, a detailed explanation of the specific risks and complications associated with aesthetic procedures, allowing the patient to thoroughly understand these issues. In addition, the patient must be aware of the actual results that can be expected, to avoid frustration after a procedure is performed26.
[1] Defined as intake, in a given period (usually less than two hours), of a substantially larger amount of food than most individuals would eat in the same period in similar circumstances.
CONCLUSIONS
Psychiatric disorders are not always considered a contraindication for aesthetic procedures; however, due to the high incidence of subsequent complications and patient dissatisfaction with the results, the professional must be alert to the signs and symptoms of these disorders39. It is then up to the medical professional to assume an ethically correct posture, respecting the autonomy of the patient, but also taking into consideration the technical indications, the associated risks and, above all, the benefit that the procedures will bring to the patient.
COLLABORATIONS
JNS Analysis and/or interpretation of data; final approval of the manuscript; conception and design of the study; writing the manuscript or critical review of its contents.
FO Analysis and/or interpretation of data; final approval of the manuscript; conception and design of the study; writing the manuscript or critical review of its contents.
JCMN Final approval of the manuscript; Writing the manuscript or critical review of its contents.
RCN Final approval of the manuscript; Writing the manuscript or critical review of its contents.
REFERENCES
1. International Society of Aesthetic Plastic Surgeons (ISAPS). International Survey on Aesthetic/Cosmetic – 2013 [acesso 2017 Out 9] Disponível em: http://www.isaps.org/Media/Default/global-statistics/2014%20ISAPS%20Global%20Stat%20Results.pdf
2. Brunton G, Paraskeva N, Caird J, Bird KS, Kavanagh J, Kwan I, et al. Psychosocial predictors, assessment, and outcomes of cosmetic procedures: a systematic rapid evidence assessment. Aesthetic Plast Surg. 2014;38(5):1030-40. PMID: 24962402 DOI: http://dx.doi.org/10.1007/s00266-014-0369-4
3. von Soest T, Kvalem IL, Roald HE, Skolleborg KC. The effects of cosmetic surgery on body image, self-esteem, and psychological problems. J Plast Reconstr Aesthet Surg. 2009;62(10):1238-44. PMID: 18595791 DOI: http://dx.doi.org/10.1016/j.bjps.2007.12.093
4. Imadojemu S, Sarwer DB, Percec I, Sonnad SS, Goldsack JE, Berman M, et al. Influence of surgical and minimally invasive facial cosmetic procedures on psychosocial outcomes: a systematic review. JAMA Dermatol. 2013;149(11):1325-33. PMID: 24068036 DOI: http://dx.doi.org/10.1001/jamadermatol.2013.6812
5. Rahmani N, Hashemi SA, Ehteshami S. Vitamin E and its clinical challenges in cosmetic and reconstructive medicine with focus on scars; a review. J Pak Med Assoc. 2013;63(3):380-2.
6. de Aquino MS, Haddad A, Ferreira LM. Assessment of quality of life in patients who underwent minimally invasive cosmetic procedures. Aesthetic Plast Surg. 2013;37(3):497-503. DOI: http://dx.doi.org/10.1007/s00266-012-9992-0
7. Ritvo EC, Melnick I, Marcus GR, Glick ID. Psychiatric conditions in cosmetic surgery patients. Facial Plast Surg. 2006;22(3):194-7. DOI: http://dx.doi.org/10.1055/s-2006-950177
8. Ishigooka J, Iwao M, Suzuki M, Fukuyama Y, Murasaki M, Miura S. Demographic features of patients seeking cosmetic surgery. Psychiatry Clin Neurosci. 1998;52(3):283-7. PMID: 9681579 DOI: http://dx.doi.org/10.1046/j.1440-1819.1998.00388.x
9. Mulkens S, Bos AE, Uleman R, Muris P, Mayer B, Velthuis P. Psychopathology symptoms in a sample of female cosmetic surgery patients. J Plast Reconstr Aesthet Surg. 2012;65(3):321-7. DOI: http://dx.doi.org/10.1016/j.bjps.2011.09.038
10. American Psychological Association - APA. Diagnostic and Statistical Manual of Mental disorders - DSM-5. 5th ed. Washington: American Psychiatric Association; 2013.
11. Conrado LA. Transtorno dismórfico corporal em dermatologia: diagnóstico, epidemiologia e aspectos clínicos. An Bras Dermatol. 2009;84(6):569-81. DOI: http://dx.doi.org/10.1590/S0365-05962009000600002
12. Sarwer DB, Spitzer JC. Body image dysmorphic disorder in persons who undergo aesthetic medical treatments. Aesthet Surg J. 2012;32(8):999-1009. DOI: http://dx.doi.org/10.1177/1090820X12462715
13. Crerand CE, Franklin ME, Sarwer DB. Body dysmorphic disorder and cosmetic surgery. Plast Reconstr Surg. 2006;118(7):167e-80e. PMID: 17102719 DOI: http://dx.doi.org/10.1097/01.prs.0000242500.28431.24
14. Picavet VA, Gabriëls L, Grietens J, Jorissen M, Prokopakis EP, Hellings PW. Preoperative symptoms of body dysmorphic disorder determine postoperative satisfaction and quality of life in aesthetic rhinoplasty. Plast Reconstr Surg. 2013;131(4):861-8. PMID: 23249985 DOI: http://dx.doi.org/10.1097/PRS.0b013e3182818f02
15. Phillips KA, Grant J, Siniscalchi J, Albertini RS. Surgical and nonpsychiatric medical treatment of patients with body dysmorphic disorder. Psychosomatics. 2001;42(6):504-10. PMID: 11815686 DOI: http://dx.doi.org/10.1176/appi.psy.42.6.504
16. Crerand CE, Phillips KA, Menard W, Fay C. Nonpsychiatric medical treatment of body dysmorphic disorder. Psychosomatics. 2005;46(6):549-55. PMID: 16288134 DOI: http://dx.doi.org/10.1176/appi.psy.46.6.549
17. Veale D. Outcome of cosmetic surgery and DIY' surgery in patients with body dysmorphic disorder. Psych Bulletin. 2000;24(6):218-20. DOI: http://dx.doi.org/10.1192/pb.24.6.218
18. Tignol J, Biraben-Gotzamanis L, Martin-Guehl C, Grabot D, Aouizerate B. Body dysmorphic disorder and cosmetic surgery: evolution of 24 subjects with a minimal defect in appearance 5 years after their request for cosmetic surgery. Eur Psychiatry. 2007;22(8):520-4. DOI: http://dx.doi.org/10.1016/j.eurpsy.2007.05.003
19. Pecorari G, Gramaglia C, Garzaro M, Abbate-Daga G, Cavallo GP, Giordano C, et al. Self-esteem and personality in subjects with and without body dysmorphic disorder traits undergoing cosmetic rhinoplasty: preliminary data. J Plast Reconstr Aesthet Surg. 2010;63(3):493-8. DOI: http://dx.doi.org/10.1016/j.bjps.2008.11.070
20. Reichert M, Scheithauer M, Hoffmann TK, Hellings P, Picavet V. What rhinoplasty surgeons should know about body dysmorphic disorder (BDD). Laryngorhinootologie. 2014;93(8):507-13.
21. Jávo IM, Pettersen G, Rosenvinge JH, Sørlie T. Predicting interest in liposuction among women with eating problems: a population-based study. Body Image. 2012;9(1):131-6. DOI: http://dx.doi.org/10.1016/j.bodyim.2011.08.002
22. Willard SG, McDermott BE, Woodhouse LM. Lipoplasty in the bulimic patient. Plast Reconstr Surg. 1996;98(2):276-8. DOI: http://dx.doi.org/10.1097/00006534-199608000-00010
23. Saariniemi KM, Helle MH, Salmi AM, Peltoniemi HH, Charpentier P, Kuokkanen HO. The effects of aesthetic breast augmentation on quality of life, psychological distress, and eating disorder symptoms: a prospective study. Aesthetic Plast Surg. 2012;36(5):1090-5. DOI: http://dx.doi.org/10.1007/s00266-012-9917-y
24. Saariniemi KM, Salmi AM, Peltoniemi HH, Helle MH, Charpentier P, Kuokkanen HO. Abdominoplasty improves quality of life, psychological distress, and eating disorder symptoms: a prospective study. Plast Surg Int. 2014;2014:197232. DOI: http://dx.doi.org/10.1155/2014/197232
25. Saariniemi KM, Salmi AM, Peltoniemi HH, Charpentier P, Kuokkanen HO. Does Liposuction Improve Body Image and Symptoms of Eating Disorders? Plast Reconstr Surg Glob Open. 2015;3(7):e461. DOI: http://dx.doi.org/10.1097/GOX.0000000000000440
26. Veer V, Jackson L, Kara N, Hawthorne M. Pre-operative considerations in aesthetic facial surgery. J Laryngol Otol. 2014;128(1):22-8. PMID: 24406082 DOI: http://dx.doi.org/10.1017/S0022215113003162
27. Caddell J, Lyne J. Personality disorders in patients seeking appearance-altering procedures. Oral Maxillofac Surg Clin North Am. 2010;22(4):455-60. DOI: http://dx.doi.org/10.1016/j.coms.2010.07.003
28. Davison SE. Principles of managing patients with personality disorder. Adv Psychiatr Treat. 2002;8(1):1-9. DOI: http://dx.doi.org/10.1192/apt.8.1.1
29. Honigman RJ, Phillips KA, Castle DJ. A review of psychosocial outcomes for patients seeking cosmetic surgery. Plast Reconstr Surg. 2004;113(4):1229-37. PMID: 15083026 DOI: http://dx.doi.org/10.1097/01.PRS.0000110214.88868.CA
30. Zojaji R, Arshadi HR, Keshavarz M, Mazloum Farsibaf M, Golzari F, Khorashadizadeh M. Personality characteristics of patients seeking cosmetic rhinoplasty. Aesthetic Plast Surg. 2014;38(6):1090-3. PMID: 25270095 DOI: http://dx.doi.org/10.1007/s00266-014-0402-7
31. Kwentus JA, Brown T. Psychiatric perspectives on facial cosmetic surgery. Ear Nose Throat J. 1980;59(10):403-11. PMID: 7227247
32. Groenman NH, Sauër HC. Personality characteristics of the cosmetic surgical insatiable patient. Psychother Psychosom. 1983;40(1-4):241-5. PMID: 6657879 DOI: http://dx.doi.org/10.1159/000287771
33. Ambro BT, Wright RJ. Psychological considerations in revision rhinoplasty. Facial Plast Surg. 2008;24(3):288-92. DOI: http://dx.doi.org/10.1055/s-0028-1083083
34. Wright MR. Management of patient dissatisfation with results of cosmetic procedures. Arch Otolaryngol. 1980;106(8):466-71. PMID: 7396791 DOI: http://dx.doi.org/10.1001/archotol.1980.00790320018005
35. Morioka D, Ohkubo F. Borderline personality disorder and aesthetic plastic surgery. Aesthetic Plast Surg. 2014;38(6):1169-76. PMID: 25209530 DOI: http://dx.doi.org/10.1007/s00266-014-0396-1
36. Napoleon A. The presentation of personalities in plastic surgery. Ann Plast Surg. 1993;31(3):193-208. DOI: http://dx.doi.org/10.1097/00000637-199309000-00001
37. Davis RE, Bublik M. Psychological considerations in the revision rhinoplasty patient. Facial Plast Surg. 2012;28(4):374-9. DOI: http://dx.doi.org/10.1055/s-0032-1319837
38. Wimalawansa SM, Fox JP, Johnson RM. The measurable cost of complications for outpatient cosmetic surgery in patients with mental health diagnoses. Aesthet Surg J. 2014;34(2):306-16. DOI: http://dx.doi.org/10.1177/1090820X13519100
39. Mowlavi A, Lille S, Andrews K, Yashar S, Schoeller T, Wechselberger G, et al. Psychiatric patients who desire aesthetic surgery: identifying the problem patient. Ann Plast Surg. 2000;44(1):97-106. PMID: 10651375 DOI: http://dx.doi.org/10.1097/00000637-200044010-00018
1. Universidade Federal do Rio Grande do Sul, Porto Alegre, RS, Brazil
2. Hospital de Clínicas de Porto Alegre, Porto Alegre, RS, Brazil
3. Universidade de Passo Fundo, Passo Fundo, RS, Brazil
Institution: Universidade Federal do Rio Grande do Sul, Porto Alegre, RS, Brazil.
Corresponding author:
Juliana Nichterwitz Scherer
Rua Gal Francisco de Paula, 556
Porto Alegre, RS, Brazil - Zip Code 91330-440
E-mail: juliananscherer@gmail.com
Article received: January 16, 2017.
Article accepted: September 23, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter