

Reviw Article - Year 2017 - Volume 32 -
Correcting historical errors in lower eyelid reconstruction
Corrigindo erros históricos na reconstrução de pálpebra inferior
ABSTRACT
The history of plastic surgery is very rich, with the description of various types of flaps and other surgical techniques over the centuries. Many authors in the nineteenth and early twentieth centuries proposed the development of surgical flaps for the reconstruction of the periorbital region, which allowed the repair of eyelid deformities at the time and still remain of great clinical applicability to date. Owing to the presence of myriads of techniques and eponyms, often describing identical or very similar techniques, a plastic surgeon often feels confused while reading the description of a technique that was learned under another name during training. Sometimes, even in academic applications and evaluations, these techniques may be presented with unusual nomenclatures, alluding to the diffuser rather than to the creator of the technique, leading to misunderstandings and errors. This review aims to correct some historical errors, assisting new surgeons who wish to work in this area.
Keywords: Eyelids; Surgical flaps; History of medicine; Plastic surgery; Eyelid Neoplasias; Reconstructive surgical procedures.
RESUMO
A história da cirurgia plástica é muito rica, com a descrição de diversos tipos de retalhos e outras técnicas cirúrgicas ao longo dos séculos. Muitos autores, no século XIX e início do século XX, propuseram a confecção de retalhos cirúrgicos para reconstrução da região periorbital, que possibilitaram a reparação de deformidades palpebrais naquele momento e ainda hoje têm uma grande aplicabilidade clínica. Em meio a uma miríade de técnicas e epônimos, que muitas vezes descrevem técnicas idênticas ou muito semelhantes, o cirurgião plástico sente-se confuso ao ler a descrição de uma técnica que durante a sua formação aprendeu com outro nome. Por vezes, mesmo em concursos ou avaliações, essas técnicas podem se apresentar com nomenclatura pouco usual, fazendo alusão ao difusor ao invés do criador da técnica, levando a equívocos e erros. Este artigo de revisão tem o objetivo de corrigir alguns erros históricos, e servir de apoio aos novos cirurgiões que desejam trabalhar nesta área.
Palavras-chave: Pálpebras; Retalhos cirúrgicos; História da medicina; Cirurgia plástica; Neoplasias palpebrais; Procedimentos cirúrgicos reconstrutivos.
Reconstruction of lower eyelid defects, whether of congenital, neoplastic, or traumatic origin, can be performed using various standard techniques, which provide safe and reliable results. Many authors have described the unique features of the eyelid anatomy, as well as their approaches, to periorbital reconstruction. Some developed their own techniques and approaches to defects, whereas others only added small details to and slightly modified the traditional techniques already described for the reconstruction of the complex anatomy of the eyelids1.
Owing to the presence of myriads of techniques and eponyms, often describing identical or very similar techniques, a plastic surgeon often feels confused while reading the description of a technique that was learned under another name during training. Sometimes, even in academic applications or evaluations, these techniques may be presented with unusual nomenclatures, alluding to the diffuser rather than to the creator of the technique, leading to misunderstandings and errors.
OBJECTIVE
This review aimed to clarify the history of lower eyelid reconstruction and to correct nomenclature errors in the technique that uses flaps from the upper eyelid or the frontal region, for reconstruction of the lower eyelid.
LITERATURE REVIEW
The history of plastic surgery intertangles with the history of medicine itself. References to the use of sutures for wound closure on the face, use of splints for correction of different nasal fractures, and topics for facial rejuvenation can be found in ancient Egyptian writings ("Smith's papyrus"), dating back approximately 2000 years BC2.
Carl Ferdinand von Graefe, often designated as the founder of modern plastic surgery, was credited with having performed the first true reconstructive blepharoplasty in 1809. He performed the reconstruction of the lower eyelid in a young woman with gangrene secondary to erysipelas, and he used a pedicle flap on the skin of the adjacent cheek region3. Since then, different techniques for partial or total reconstruction of the lower eyelids have been developed.
Most reconstructions of the anterior lamella of the lower eyelid can be performed by direct closure of small defects, grafts, or rotation of laterally based flaps and vertical myocutaneous flaps for larger defects4.
The preparation of the transposition flaps for the closure of the lower eyelid defects began approximately two centuries prior. Johan Karl Fricke, in 1829, extensively described the treatment of palpebral deformities by using flaps of the periorbital regions. He described the use of a monopedicled flap based on the temporal region in his publications5,6 (Figure 1), which became popularly known as the Fricke flap.

Figure 1. Fricke flap, published in 1829.
Preparation and final appearance of the original Fricke patch5.
This type of flap can be used in the reconstruction of major defects in the upper or lower eyelid. A lateral base skin flap uses the skin above the eyebrow and is transposed to cover the anterior lamella defect. This flap is raised subcutaneously to avoid deepening in the region, which could cause injury to the temporal branch of the facial nerve.
Therefore, this flap is only used on the reconstruction of defects of the anterior lamella, whereas reconstruction of the posterior lamella must be performed with grafts for full thickness defects. The donor area is usually closed by primary closure. A disadvantage of this type of flap is the elevation of the eyebrow because this ends up being mobilized superiorly to enable the primary closure.
The transposition of the skin from the upper lid to the lower lid is often incorrectly called the Fricke flap. The design of this flap, which was used to treat an ectropion of the lower eyelid caused by burns, was first described by William Horner in 1837 at a university in Pennsylvania7. According to some authors8, William Horner was the first to accurately describe a true Z-plasty (Figure 2).
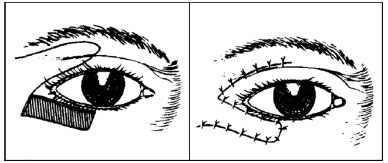
Figure 2. Flap described by Horner in 1837.
Flap exchanging skin from upper to lower eyelid (or Z-plasty)7.
Only some years later, in 1854, Denonvilliers described a similar procedure. However, many surgeons consider him the creator of the Z-plasty technique. Denonvilliers used this flap to repair a lower eyelid deformity by using the skin of the upper eyelid to correct a cicatricial ectropion9. However, during that time he never made a reference to the term Z-plasty, which only became popular in the following years.
Because no illustration was reported in the original Denonvilliers publications, the first diagrams illustrating this surgery for correction of cicatricial ectropion only appeared in the following years. In 1860, Cazelles, one of Denonvilliers' students, published his doctoral thesis containing several diagrams (Figure 3). This thesis was largely based on what the author learned from Denonvilliers regarding the treatment of eyelid ectropion and undoubtedly contributed to the spread of his mentor's popularity.

Figure 3. Correction of cicatricial ectropion described by Cazzeles in 1860.
Illustration extracted from the thesis of Cazelles, a disciple of Denonvilliers, who demonstrated the correction of cicatricial ectropion through a flap from the upper eyelid to the lower eyelid, as recommended by his mentor10.
Beard11 and Davis12, more than half a century after Denonvilliers' original descriptions for the treatment of cicatricial ectropion, helped popularize the author's name in the United States (Figure 4)13.

Figure 4. Denonvilliers' original Z-plasty assumption, published by Beard and Davis in the USA, at the beginning of the 20th century11,12.
There is no doubt that these incisions in Z and patchwork for the relief of contractures had Denonvilliers as one of the main precursors of the technique. Because of the limitations of information diffusion at the time, the technique was often "rediscovered" by other authors and published as a "new procedure"14.
Landolt, in 1885, was the first to describe the use of a bipediculated flap of the upper eyelid. This oculoplastic surgeon described the possibility of separating the anterior and posterior lamellae, allowing for the construction of two well-vascularized flaps that could be easily slid over the other, and the rearrangement between the lamellae, enabling the correction of defects in one of the lamellae without the need for more distant flaps15.
This author recognized the importance of including the muscle in the skin flap, aiming at good vascularization, although without considering the possibility of the muscle remaining innervated and functional. The procedure was recommended in two steps, wherein the pedicles of the upper eyelid should be sectioned in a second stage.
Another pioneer in the reconstruction of the lower eyelid using flaps of the upper eyelid was French Léon Tripier16. He is believed to have performed the first case of eyelid reconstruction using a functional myocutaneous flap17. In 1888, Tripier, described the use of a bipediculated flap of the upper eyelid with the conformation of a bridge, based on the orbicularis oculi muscle, to repair major defects in the lower eyelid.
One of Tripier's goals was to achieve a musculocutaneous flap that would injure as few nerve fibers as possible and also maintain the continuity of the fibers of the orbicularis muscle to restore the correct function of the lower eyelid. This attempt had failed at the hands of his predecessors18. Tripier reported to be successful in treating three cases of extensive lower eyelid reconstruction using the bipediculated upper eyelid flap (Figure 5). In this same publication, he described the creation of a bipediculated analog flap of the frontal region just above the eyebrow to treat defects ranging from one-half to two-thirds of the upper eyelid.

Figure 5. Original description of Tripier's bipediculated myocutaneous flap.
Léon Tripier described, in 1889, in the newspaper Gazette des Hôpitaux de Paris, a functional bipediculated myocutaneous flap, based on the orbicularis oculi muscle - there is no drawing in the original article16.
Figure 6 shows the schematic representation of the first bipediculated flap described by Tripier.

Figure 6. Tripier flap.
Tripier's bipediculated myocutaneous flap scheme. Adapted from: Grabb & Smith's Plastic Surgery. 6th Ed. 2007 by Lippincott Willians & Wilkins. Philadelphia, PA, USA. p. 404.
Sir Harold Gillies, a New Zealand otolaryngologist based in London, considered one of the greatest surgeons of the last century, used two head and neck molds to teach reconstruction using flaps to surgeons in the Armed Forces, during the First World War (Figure 7). These molds clearly showed an example of the modified Tripier bipediculated flap, which was being used to transfer skin from the supraciliary region to cover the lower palpebral region18.

Figure 7. Molds developed by Gillies.
Notice the preparation of the modified Tripier flap in the left periorbital region18.
A Landolt student, Dupuis-Dutemps, in 1901, described a modification in the original flap of his teacher, using only one pedicle of the upper eyelid to maintain the vascularization of the flap19.
Other authors have subsequently modified these earlier descriptions. They described the same flap, although with minor modifications.
Most of the surgeries applied in eyelid reconstruction have their foundations in techniques described almost two centuries prior. A large number of these ancient techniques continue to have great applicability today.
Finding the title of a publication on a "new technique" discovered in the surgical literature is common. However, this new technique sometimes represents only a minor modification of an old procedure that the author does not even mention, either by lack of knowledge or vanity.
We conclude this review by making an allusion to the Latin proverb, "nihil sub sole novum," that is, "there is nothing truly new in existence." Every new idea has some kind of precedence or echo of the past.
COLLABORATIONS
AAA Analysis and/or interpretation of data; final approval of the manuscript; conception and design of the study; writing the manuscript or critical review of its contents.
RSF Analysis and/or interpretation of data; final approval of the manuscript; conception and design of the study; writing the manuscript or critical review of its contents.
REFERENCES
1. Rafii AA, Enepekides DJ. Upper and lower eyelid reconstruction: the year in review. Curr Opin Otolaryngol Head Neck Surg. 2006;14(4):227-33. DOI: http://dx.doi.org/10.1097/01.moo.0000233592.76552.d2
2. The Edwin Smith Surgical Papyrus. Bethesda: National Library of Medicine (US), History of Medicine Division; 2015. [acesso 2017 Out 27]. Disponível em: https://ceb.nlm.nih.gov/proj/ttp/flash/smith/smith.html
3. Rogers BO. History of oculoplastic surgery: the contributions of plastic surgery. Aesthetic Plast Surg. 1988;12(3):129-52. DOI: http://dx.doi.org/10.1007/BF01570922
4. McCord CD, Codner MA. Lower eyelid reconstruction. In: McCord C, Codner M, eds. Eyelid and Periorbital Surgery. 1st ed. St. Louis: Quality Medical Publishing; 2008. p. 543-76.
5. Fricke JCG. Die Bildung neuer Augenlider (Blepharoplastik) nach Zerstorungen und dadurch hervorgebrachten Auswartswendungen derselben. Hamburg: Perthes and Bessler; 1829.
6. Montandon D, Maillard G. Plasties et Reconstructions Orbitopalpebrales. Medicine et Hygiene. Geneve; 1979.
7. Horner W. Clinical Report on the Surgical Department of the Philadelphia Hospital, Blockley, for the months of May, June, and July, 1837. Am J Med Sci. 1837;20(41):99-112. DOI: http://dx.doi.org/10.1097/00000441-183720410-00005
8. Borges AF, Gibson T. The original Z-plasty. Br J Plast Surg. 1973;26(3):237-46. PMID: 4580014 DOI: http://dx.doi.org/10.1016/0007-1226(73)90008-8
9. Denonvilliers CP. Ectropion. Bulletins de la Société de Chirurgie de Paris. 1856;7:243.
10. Cazelles EH. Du traitement de l'ectropion cicatriciel [Thése pour le Doctorat en Médecine]. Faculte de Medecine de Paris. Rognoux, Imprimeur de la Faculté de Médecine. Paris; 1860.
11. Beard CH. Varieties of Blepharoplastly. In: Wood CA, ed. System of Ophthalmic Operations. Vol. 2, Chap. XIII. Chicago: Cleveland Press; 1911. p. 1435.
12. Davis JS. Plastic Surgery: Its Principles and Practice. Philadelphia: Blakiston's Son & Co.; 1919. p. 372-89.
13. Ivy RH. Who originated the Z-plasty? (Charles Pierre Denonvilliers). Plast Reconstr Surg. 1971;47(1):67-72. DOI: http://dx.doi.org/10.1097/00006534-197101000-00013
14. Davis JS. The relaxation of scar contractures by means of the Z-, or reversed Z-type incision: Stressing the use of scar infiltrated tissues. Ann Surg. 1931;94(5):871-84.
15. Landolt. Nouveau procéde de blepharoplastie. Archives d'Ophtalmologie 1881;1:9-13.
16. Tripier L. Lambeau musculo-cutané en forme de pont. Appliqué à la restauration des paupières. Gazette Hôpitaux Paris. 1889;62:1124-5.
17. Labbé D, Bénateau H, Rigot-Jolivet M. Homage to Leon Tripier. Description of the first musculocutaneous flap and current indications. Ann Chir Plast Esthet. 2000;45(1):17-23. PMID: 10783508
18. Elliot D, Britto JA. Tripier's innervated myocutaneous flap 1889. Br J Plast Surg. 2004;57(6):543-9. PMID: 15308402 DOI: http://dx.doi.org/10.1016/j.bjps.2004.02.021
19. Dupuy-Dutemps L. Autoplasties palpebro-palpebrale dans le traitement de l'ectropion cicatriciel de la paupiére inferieure. Arch Ophthalmol. 1901;21:518-25.
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Instituto Ivo Pitanguy, Rio de Janeiro, RJ, Brazil
3. 38ª Enfermaria da Santa Casa de Misericórdia do Rio de Janeiro, Rio de Janeiro, RJ, Brazil
4. Pontifícia Universidade Católica do Rio de Janeiro, Rio de Janeiro, RJ, Brazil
5. Universidade Federal do Paraná, Curitiba, PR, Brazil
6. Hospital de Clínicas, Universidade Federal do Paraná, Curitiba, PR, Brazil
7. Universidade de São Paulo, São Paulo, SP, Brazil
Institutions: Instituto Ivo Pitanguy, Rio de Janeiro, RJ, Brazil; Hospital de Clínicas, Universidade Federal do Paraná, Curitiba, PR, Brazil.
Corresponding author:
Alexei Almeida Andrade
Rua Sorocaba, 305, Apto 1808 - Botafogo
Rio de Janeiro, RJ, Brazil - Zip Code 22271-110
E-mail: alexeiandrade@yahoo.com.br
Article received: May 31, 2017.
Article accepted: September 23, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter