

Case Report - Year 2017 - Volume 32 -
Preceding expansion in the treatment of dermatofibrosarcoma protuberans involving the frontal bone
Expansão prévia no tratamento de dermatofibrossarcoma protuberante envolvendo o osso frontal
ABSTRACT
INTRODUCTION: Dermatofibrosarcoma protuberans is a rare skin tumor with intermediate malignancy and low metastatic potential, but a high recurrence rate after surgical treatment. Treatment involves extended resection with variable margins.
METHODS: Patients were managed with preceding expansion of tissues of the forehead using two conventional expanders. The lateral margins of normal-appearing tissue 3-cm apart were tattooed with China ink. In a preceding operation, expanders were inserted through skin incisions at a distance from the marks, by undermining the surgical plane just above the periosteum, while preserving the area of wide resection previously delimited. After the lateral tissues were expanded, the patients underwent surgical resection. The deep margin included the outer table of the frontal bone. The expansion period averaged 45 days.
RESULTS: Three cases of dermatofibrosarcoma protuberans of the forehead with involvement of the outer table of the frontal bone are described. The expanded flaps easily closed the defects. The average follow-up was 194 months without tumor recurrence.
CONCLUSION: Preceding expansion of forehead tissue in the treatment of dermatofibrosarcoma protuberans with invasion of frontal bone, using 3-cm lateral margins and removal of the outer table of the frontal bone, allowed easy closure of the defect in 3 different patients. Average follow-up of 194 months with no recurrence of the lesion showed the effectiveness of the method.
Keywords: Tissue expansion devices; Tissue expansion; Dermatofibrosarcoma; Skin neoplasms; Frontal bone.
RESUMO
INTRODUÇÃO: Dermatofibrossarcoma protuberante é um tumor cutâneo raro de malignidade intermediária e potencial metastático baixo, apresentando, entretanto, alta taxa de recorrência após tratamento cirúrgico. O tratamento cirúrgico clássico é a ressecção alargada com margens variadas.
MÉTODOS: Os pacientes foram submetidos à expansão prévia dos tecidos da região frontal utilizando dois expansores convencionais. Margens laterais de 3 cm de tecido de aparência normal foram tatuadas com tinta nanquim. Os expansores foram incluídos em uma cirurgia anterior, através de incisões cutâneas distantes dessas marcas, em um plano cirúrgico logo acima do periósteo, preservando a área de ressecção alargada previamente delimitada. Os tecidos laterais foram expandidos e, posteriormente, os pacientes foram submetidos à ressecção do tumor. A margem profunda incluiu da lâmina externa do osso frontal. O período médio de expansão foi de 45 dias.
RESULTADOS: Foram relatados três casos de dermatofibrossarcoma protuberante da região frontal com envolvimento da lâmina externa do osso frontal. Os retalhos expandidos fecharam facilmente os defeitos. O acompanhamento pós-operatório médio foi de 194 meses, sem nenhuma recorrência tumoral.
CONCLUSÃO: A expansão tecidual prévia da região frontal no tratamento do dermatofibrossarcoma protuberante, invadindo o osso frontal, usando margens laterais de 3 cm com remoção da lâmina externa, permitiu facilmente o fechamento do defeito, em três pacientes. O tempo de acompanhamento médio de 194 meses sem nenhuma recorrência tumoral mostrou a eficiência do método.
Palavras-chave: Dispositivos para expansão de tecidos; Expansão de tecido; Dermatofibrossarcoma; Neoplasias cutâneas; Osso frontal.
Dermatofibrosarcoma protuberans (DFSP) is a rare infiltrative skin tumor with intermediate malignancy. It has a low potential for metastasis but a high rate of recurrence after surgical treatment1-5. The treatment of choice is surgical wide resection with lateral margins of at least 3 cm and a deep margin including an anatomical structure without tumor infiltration, such as the deep fascia, muscle, periosteum, or outer table of cranial bone2,6-8.
OBJECTIVE
This retrospective study reviewed data of patients with dermatofibrosarcoma protuberans of the forehead involving invasion of frontal bone, treated by preceding expansion of frontal flaps between September 1992 and May 2005.
METHODS
Data of 3 patients who underwent surgery at Hospital Felício Rocho (Belo Horizonte, MG) between September 1992 and April 2005 were reviewed. The patients underwent preceding expansion of tissues of the forehead using two conventional expanders. Lateral margins of normal-appearing tissue 3-cm apart were tattooed with China ink. In a preceding operation, expanders were inserted through skin incisions at a distance from that marks, by undermining the surgical plane just above the periosteum, while preserving the area of wide resection previously delimited. After the lateral tissues were expanded, the patients underwent surgical resection. The deep margin included the outer plate of the frontal bone. The expansion period averaged 45 days.
There were no conflicts of interest or sources of funding. The principles of the Declaration of Helsinki were followed. All patients received an Informed Consent Form. The study was conducted at Hospital Felício Rocho, Belo Horizonte, MG, in the year 2017
RESULTS
Three cases of DFSP of the forehead with involvement of the outer plate of the frontal bone were identified. There was no recurrence during an average follow-up of 194 months.
Case report
Case 1
A male, aged 38 years, with tumor appearance 14 years prior. Tumor resection plus radiotherapy performed elsewhere were followed by recurrence. After admission, biopsy confirmed DFSP. Insertion of expanders was performed in September 1992. Enlarged resection was performed in October 1992, using 3-cm lateral margins, with removal of the outer table of the frontal bone. Expanded flaps easily closed the defect. In March 2008, the patient underwent left nephrectomy for renal carcinoma. In August 2010, he died with multiple metastases of the renal tumor, but no recurrence of DFSP. After the excision, the patient remained free of tumor for 214 months (Figure 1).
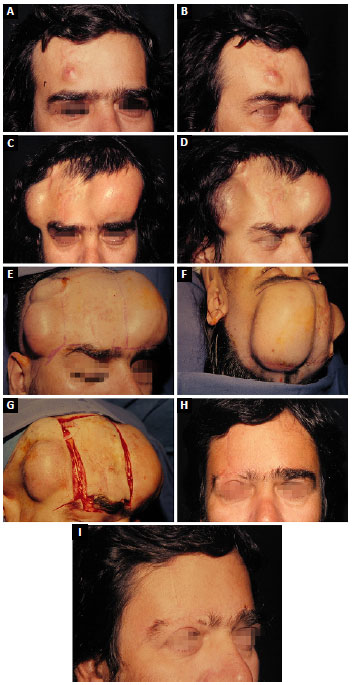
Figure 1. Case 1. A: Dermatofibrosarcoma protuberans in the right frontal region; B: Lateral view; C: Complete flap expansion, frontal view; D: Complete flap expansion, lateral view; E: Location of the incision used to position the expander in the frontal region; F: Preoperative marking of the tumor resection area; G: Extensive resection of dermatofibrosarcoma protuberans; H: Postoperative result, frontal view; I: Postoperative result, lateral view.
Case 2
A male, aged 41 years, with tumor appearance 10 years prior. Two previous surgical resections followed by recurrences were performed elsewhere. After admission, biopsy confirmed DFSP. The patient underwent insertion of skin expanders in April 1998. Enlarged resection was performed in July 1998 using 3-cm lateral margins, with removal of the outer table of the frontal bone. Expanded flaps easily closed the defect. The last follow-up examination was in May 2017 showed no signs of DFSP. The patient was free of tumor for the prior 226 months (Figure 2).
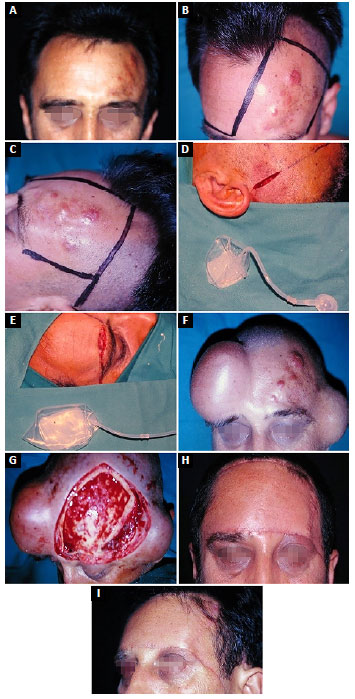
Figure 2. Case 2. A: Dermatofibrosarcoma protuberans in the left frontal region; B: Preoperative marking for placement of the expander, frontal view; C: Preoperative marking, lateral view; D: Expander in left temporal region; E: Expander in right frontal region; F: Complete flap expansion; G: Extensive resection of dermatofibrosarcoma protuberans, with removal of the outer table of the frontal bone; H: Postoperative result, frontal view; I: Postoperative result, lateral view.
Case 3
A male, aged 28 years, reported appearance of the tumor 2 years prior. A previous resection performed elsewhere was followed by a recurrence. Insertion of expanders was performed in April 2005. Wide resection was performed in May 2005, using 3-cm lateral margins, with removal of the outer table of the frontal bone. The last follow-up examination in May 2017 showed no signs of DFSP. The patient was free of tumor for the prior 144 months.
DISCUSSION
Silva Filho et al.1 originally described the use of tissue expanders for a case of DFSP of the frontal region. That particular case was case 1 in the present series. Alves et al.2 described 2 more cases of preceding expansion for forehead DFSP. Khachemoune et al.6 reported a single case of DFSP involving the frontal region in which the outer tables of the calvarium were removed and the patient underwent multistaged repair using skin expanders.
No other papers were found reporting use of tissue expansion in the treatment of DFSP of the frontal region.
Although considered a malignant tumor, DFSP grows slowly and rarely metastasizes. In a series of 30 patients treated with radical surgery, Alves et al.2 found no cases with metastatic disease. This characteristic allows the use of tissue expanders near the tumor without increased risk of disseminating the DFSP.
CONCLUSION
Preceding expansion of forehead tissue in treatment of DFSP invading frontal bone, using 3-cm lateral margins with removal of the outer table, allowed easy closure of the defect in 3 different patients. Average follow-up of 194 months with no recurrence of the lesion showed the effectiveness of the method.
COLLABORATIONS
EHP Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; writing the manuscript or critical review of its contents.
JCRRA Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
AFSF Final approval of the manuscript; completion of surgeries and/or experiments.
RPLF Analysis and/or interpretation of data; final approval of the manuscript.
NAP Analysis and/or interpretation of data; final approval of the manuscript.
ACMA Final approval of the manuscript.
JSAF Completion of surgeries and/or experiments.
REFERENCES
1. Silva Filho AF, Andrade Filho JS, Siqueira IMG, Saraiva PS, Magalhães GM, Alves JCRR. Dermatofibrossarcoma protuberante: aspectos clínicos e cirúrgicos. An Bras Dermatol. 1997;72(3):247-51.
2. Alves JCRR, Fonseca RPL, Silva Filho AF, Andrade Filho JS, Araujo IC, Almeida ACM, et al. Ressecção alargada no tratamento do dermatofibrossarcoma protuberante. Rev Bras Cir Plást. 2014;29(3):395-403.
3. McKee PH, Calonge E, Granter SR. Dermatofibrosarcoma protuberans. In: McKee PH, Calonge E, Granter SR, eds. Pathology of the skin with clinical correlations. 3rd ed. Philadelphia: Elsevier Mosby; 2005. p. 1729-35.
4. Shapiro L, Brownstein MH. Dermatofibrosarcoma protuberans. In: Andrade R, Gumport SL, Popkin GL, Rees TD, eds. Cancer of the skin: biology, diagnosis, management. Philadelphia: WB Saunders; 1976. p. 1069-78. DOI: http://dx.doi.org/10.1097/00000658-196711000-00011
5. McPeak CJ, Cruz T, Nicastri AD. Dermatofibrosarcoma protuberans: an analysis of 86 cases-five with metastasis. Ann Surg. 1967;166(5):803-16. PMID: 4964386
6. Khachemoune A, Barkoe D, Braun M 3rd, Davison SP. Dermatofibrosarcoma protuberans of the forehead and scalp with involvement of the outer calvarial plate: multistaged repair with the use of skin expanders. Dermatol Surg. 2005;31(1):115-9.
7. Heenan PJ. Tumors of the fibrous tissue involving the skin. In: Elder D, ed. Lever's histopathology of the skin. 8th ed. Philadelphia: Lippincott-Raven; 1997. p. 847-87.
8. Portugal EH, Alves JCRR, Fonseca RPL, Andrade Filho JS, Almeida ACM, Araújo IC, et al. Dermatofibrossarcoma protuberante diagnosticado erroneamente como queloide e tratado com acetonido de triancinolona. Rev Bras Cir Plást. 2016;31(1):82-7.
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Hospital Felício Rocho, Belo Horizonte, MG, Brazil
3. Instituto de Cirurgia Plástica Avançada, Belo Horizonte, MG, Brazil
4. Universidade Federal de Minas Gerais, Belo Horizonte, MG, Brazil
5. Faculdade de Medicina da Universidade de Itaúna, MG, Brazil
6. Hospital e Maternidade Therezinha de Jesus, Juiz de Fora, MG, Brazil
7. Faculdade de Ciências Médicas de Minas Gerais, Belo Horizonte, MG, Brazil
Institution: Hospital Felício Rocho, Belo Horizonte, MG, Brazil.
Corresponding author:
Erick Horta Portugal
Rua Santa Maria de Itabira, 217 - Sion
Belo Horizonte, MG, Brazil - Zip Code 30310-600
E-mail: erickhphp@yahoo.com.br
Article received: May 25, 2017.
Article accepted: September 23, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter