

Original Article - Year 2018 - Volume 33 -
Venous thromboembolism in abdominoplasty: a prevention protocol
Tromboembolismo venoso (TEV) em abdominoplastias: um protocolo de prevenção
ABSTRACT
INTRODUCTION: Abdominoplasty is an accomplished cosmetic surgery, in which the risk of venous thromboembolism (VTE) must be considered, based on the predisposing factors involved and their severity. There are, to date, no well-defined protocols for VTE prophylaxis in plastic surgery. The objective of this paper is to present a protocol for the prophylaxis of VTE used in the Plastic Surgery Service of the Hospital e Maternidade Celso Pierro (HMCP) - Pontifícia Universidade Católica (PUC) de Campinas in São Paulo (SP), while also showing the incidence of VTE in patients undergoing abdominoplasties before and after initiation of the protocol, as well as the incidence of hematomas after the total period of 6 years.
METHODS: For the creation of this protocol, medical records of patients who underwent abdominoplasty from January 2010 to December 2015 were revised, identifying cases of VTE in this period, associated or not with the use of pharmacological prophylaxis, and those of hematoma after initiation of the protocol.
RESULTS: The protocol for prophylaxis of VTE that has been used in the service since 2014 is based on the Anger Protocol and includes non-pharmacological measures and pharmacological measures. Two hundred and forty-three medical records were analyzed in this study. After initiation of the protocol, no cases of VTE were observed in the 74 patients who underwent abdominoplasty, and only one case of hematoma was observed. Before the protocol was initiated, VTE developed in 2 cases among 169 operated patients.
CONCLUSION: After adopting the VTE prophylaxis protocol, we achieved an incidence of 0% VTE in the abdominoplasties in this period, compared to an incidence of 1.18% before the protocol. The incidence of bruising after surgery was 1.35%, which is comparable to rates in the literature for surgery without the use of pharmacological prophylaxis.
Keywords: Abdominoplasty; Venous thromboembolism; Reconstructive surgical procedures; Chemoprevention; Surgery; Plastic.
RESUMO
INTRODUÇÃO: A abdominoplastia é uma cirurgia estética muito realizada, na qual o risco de tromboembolismo (TEV) deve ser considerado pelos fatores predisponentes envolvidos e por sua gravidade. Não há, até o momento, protocolos bem definidos para profilaxia de TEV em Cirurgia Plástica. O objetivo é apresentar um protocolo de profilaxia de TEV utilizado no serviço de Cirurgia Plástica do HMCP - PUC Campinas, mostrando a incidência de TEV nas abdominoplastias antes e após o início do protocolo, bem como a incidência de hematomas após, no período total de 6 anos.
MÉTODOS: Revisão de prontuários de pacientes submetidos à abdominoplastia no período de janeiro de 2010 a dezembro de 2015, identificando os casos de TEV nesse período, associados ou não ao emprego de profilaxia farmacológica, e os de hematoma após início do protocolo.
RESULTADOS: O protocolo de profilaxia de TEV que é utilizado no serviço desde 2014 tem como base o protocolo de Anger e inclui medidas não farmacológicas e farmacológicas. Foram analisados 243 prontuários nesse estudo. Após início do protocolo, não foi evidenciado nenhum caso de TEV nos 74 pacientes submetidos à abdominoplastia e foi observado apenas um caso de hematoma. Já antes do mesmo, 2 casos de TEV ocorreram entre 169 pacientes operados.
CONCLUSÃO: Após a adoção do protocolo de profilaxia de TEV, alcançamos uma incidência de TEV de 0% nas abdominoplastias nesse período, enquanto a mesma foi de 1,18% antes do protocolo. Já a incidência de hematomas após foi de 1,35%, comparável a taxas da literatura para a cirurgia sem a utilização de profilaxia farmacológica.
Palavras-chave: Abdominoplastia; Tromboembolia venosa; Procedimentos cirúrgicos reconstrutivos; Quimioprevenção; Cirurgia plástica.
Deep venous thrombosis (DVT) and pulmonary thromboembolism (PTE), which is the most severe outcome, are components of the nosological entity known as venous thromboembolism (VTE) and are relatively common complications for patients undergoing surgery. In the literature, there are few publications on the incidence of VTE in plastic surgery and suggested protocols for its prevention, with no definition of onset and duration of prophylaxis.
Thromboembolic events are largely silent clinically and difficult to diagnose, which leads to a delay in treatment and, consequently, a high mortality rate. A prevention protocol is vital in order to avoid this dreaded outcome1. Studies show that most plastic surgeons do not incorporate prophylactic regimens consistent with their practice (up to 25% do not perform prophylaxis in patients undergoing abdominoplasty for fear of hemorrhagic complications).2
Body contour procedures, such as abdominoplasty, involve prolonged operative time under general anesthesia, extensive dissection, and a postoperative time of reduced mobility; all of these are risk factors for a thromboembolic event. Although abdominoplasty has a low mortality rate, the main cause of death is PTE.2 In order to stratify the risk of DVT/PTE, there are protocols that guide whether prophylaxis is necessary and which is the best therapeutic option for each case.
OBJECTIVE
The objective of this paper is to present a protocol of prophylaxis for VTE to be used in the Plastic Surgery Service of the Hospital e Maternidade Celso Pierro (HMCP) - Pontifícia Universidade Católica (PUC) de Campinas in São Paulo (SP), showing the incidence of VTE in patients undergoing abdominoplasties before and after initiation of the protocol, as well as the incidence of hematomas after a total period of 6 years.
METHODS
A retrospective study was performed at the Plastic Surgery Service of HMCP - PUC Campinas/SP, with a medical records analysis of all patients who underwent abdominoplasty (conventional and anchor/Torek) and were operated between January 2010 and December 2015. In this study, only abdominoplasties were considered, and all patients were put under general anesthesia.
From January 2010 to December 2013, 169 patients who only used non-pharmacological prophylaxis (elastic stocking, intraoperative lower limb manipulation, early ambulation) were operated on, and from January 2014 to December 2015, 74 patients who had used non-pharmacological prophylaxis associated with pharmacological prophylaxis, initially with enoxaparin 40 mg/day for 5 days and then with rivaroxaban 10 mg/day for 10 days, totaling a period of 15 days of drug prophylaxis, underwent an operation.
The present study followed the principles of Helsinki and all patients completed the Informed Consent Term prior to the surgical procedure.
RESULTS
Until December 2013, only non-pharmacological prophylaxis of VTE (elastic stocking, intraoperative lower limb manipulation, early ambulation) was used in abdominoplasties at our plastic surgery service. As of January 2014, based on the work of Anger,3 we adopted a protocol for stratification of DVT/PTE risk.
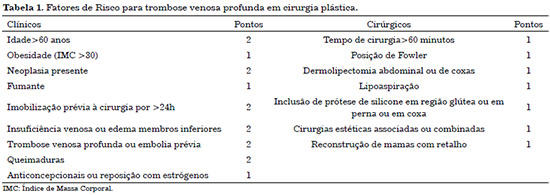
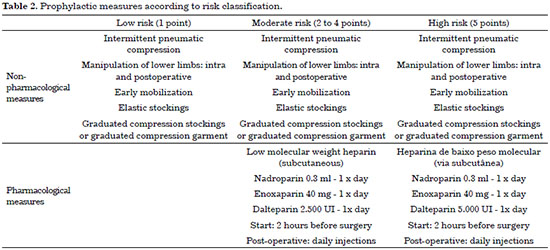
This protocol is the most used for plastic surgery in Brazil. Patients with <1 point are considered to be at low risk and do not require pharmacological prophylaxis; however, patients with a score of 2 to 4 are at moderate risk and those with a score of >5 are at high risk (Table 1). Drug prophylaxis is indicated for patients with a score >2 (Table 2).
Based on the Anger Protocol, all patients undergoing abdominoplasty are considered at least moderate risk, with 1 point for the surgical time greater than 60 minutes, 1 point for the surgery itself, and 1 point for the required Fowler position. Therefore, all patients undergoing this procedure should receive some type of pharmacological thromboembolic prophylaxis.2,3
The pharmacological therapy employed in our service consisted of the use of enoxaparin at a dose of 40 mg/day for 5 days, the first dose being performed during anesthetic induction. Starting on day 6, patients were given rivaroxaban at a dose of 10 mg/day for 10 days. From January 2010 to December 2015, 243 patients underwent abdominoplasty with general anesthesia. Of the total, 3 (1.23%) of the patients were male and 240 (98.7%) were female. From January 2010 to December 2013, 169 abdominoplasties were performed (2 male patients), and only non-pharmacological prophylaxis was performed. From January 2014 to December 2015, 74 abdominoplasties were performed (1 male patient).
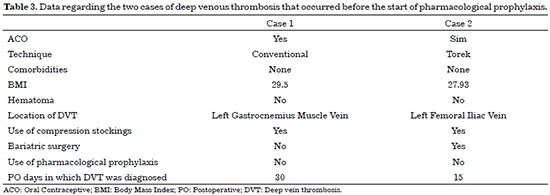
It was observed that, prior to the initiation of the protocol, when only non-pharmacological prophylaxis (elastic stocking, intraoperative lower limb manipulation, early ambulation) was used, DVT developed (Table 3) in 2 female patients using oral contraceptives (OAC). One case was a conventional abdominoplasty, while the other was an abdominoplasty at anchor. In both cases, the diagnosis was made with the help of ultrasonography with venous Doppler echocardiography after clinical suspicion.
After initiation of the protocol, we did not observe any cases of DVT or PTE. Only 1 case of hematoma was identified (Table 4), in which the patient presented hypovolemic shock and was surgically reopened in the immediate postoperative period. In the intraoperative period, a hematoma was observed in all areas of the detachment, in moderate quantity, and no active bleeding point was observed. The patient underwent transfusion of packed red blood cells and presented a favorable clinical evolution, receiving discharge in 2 days.
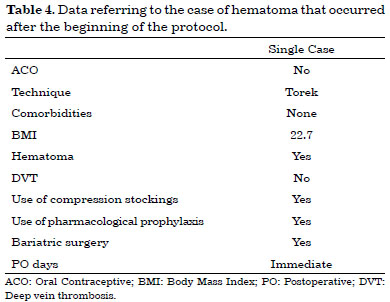
After the treatment of cases of DVT and hematoma, all the patients were subjected to an evaluation by the hematology team that excluded hematological pathologies.
A two-proportion equality test was performed (significance level p < 0.05), but the statistical analysis of the data showed no difference between cases of DVT and hematoma before and after the prophylaxis protocol was adopted (Figure 1).
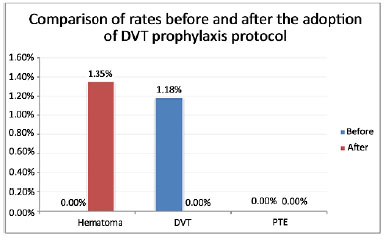
Figure 1. Rates before and after adoption of the protocol for prophylaxis of deep venous thrombosis (DVT).
DISCUSSION
Procedures like abdominoplasty have several factors that increase the4,5 risk of thromboembolic events, such as: 1) vessel injury, with intense dissection and rupture of superficial veins; 2) long operative time; 3) general anesthesia, with decreased peripheral vascular resistance; 4) intraoperative position of the patient that reduces the venous return of the extremities (venous stasis); 5) reduced postoperative mobility; 6) obesity; and 7) plication of the diastasis of the rectus abdominis muscle which decreases the venous return.
In addition, it has been described that abdominoplasty alone already shows an increase in the activity of the coagulation cascade (an increase in the production of thrombin in the postoperative period, which explains the state of hypercoagulability), which can be prevented with the use of prophylaxis.4,6 There are few studies in the literature that show the results of perioperative chemoprophylaxis in the incidence of thromboembolic events, risk of hematomas, or other adverse effects in patients undergoing plastic surgery. The timing of initiation and duration of prophylaxis remain controversial.
Studies have shown that abdominoplasty alone, when not combined with any other procedure, is associated with a rate of 0.1% to 1.1% for DVT, 0.34% to 1.1% for PTE, and 0.5 to 8% for hematoma.2,4,5 When combined surgery is performed, these values increase significantly.1 In cases of death due to PTE, specific data for abdominoplasties are not found in the literature, but a mortality rate of 0.1 to 0.8% is reported for general surgery patients.
Thromboembolic phenomena present an incidence of about 0.6% when drug prophylaxis is used. According to the literature, cases of bruising vary between 2.3 and 8% when using prophylaxis, which does not differ from the incidence of bruising in general surgery.2 However, a meta-analysis by Koch et al.7 of 39 articles, including more than 16,000 patients, demonstrated that there is an increase in bleeding/bruising rates with the use of low molecular weight heparin in patients undergoing large surgeries.
Prophylaxis for VTE, recommended for at least 7 days or more after high-risk surgery, has one disadvantage, because low molecular weight heparin is admitted via an injection. The new regimens with oral anticoagulants reduce hospitalization time and make prophylaxis less inconvenient and safer.8 Oral anticoagulants have the advantage of not requiring regular monitoring of coagulation with laboratory tests and the dose or dose range need not be altered according to the coagulation8 laboratory parameters.
On the other hand, in cases of hematoma or bleeding, when low molecular weight heparin is used as the antidote, protamine sulfate may be given. If these complications occur after administration of the new oral anticoagulants, there are still no specific antidotes that reverse the action of the anticoagulation effect.9 Therefore, in our service, we initially used enoxaparin, which comes with a greater risk of bleeding/bruising, and then replaced it with the oral anticoagulant, rivaroxaban, on day 6. This method combines security with practicality.
When we considered the use of oral anticoagulants for thromboprophylaxis (rivaroxaban in the protocol of this study), 4 large clinical studies with a total of 12,000 patients showed that rivaroxaban is superior in efficacy to 40 mg subcutaneous enoxaparin.1 Rivaroxaban is an oral anticoagulant that directly inhibits blood coagulation factor Xa and is well absorbed in the intestine. The maximum effect of rivaroxaban occurs in 4 hours and lasts up to 12 hours, but the factor Xa activity does not return to normal within 24 hours, and 1 dose per day is sufficient.
After the introduction of the protocol in our service, only 1 patient (1.35%) required a re-hemorrhage, which is comparable to bleeding rates when chemoprophylaxis is not performed.10
Considering that the coagulation cascade is activated during surgery (e.g. abdominoplasty), it would be interesting to start preoperative prophylaxis to prevent its activation. Pannucci et al.11 demonstrated that the use of prophylactic enoxaparin initiated from 6-8 hours postoperatively and maintained until hospital discharge in high-risk patients may be protective of VTE for up to 60 days.
All data presented in this study are consistent with those in the literature, including the percent of VTE before and after prophylaxis and the presence of hematoma with the use of prophylaxis (1.18% of DVT before the protocol and 0% after protocol; 1.35% hematoma after introduction of the protocol). The risk of VTE should be balanced against the increased risk of bleeding with the use of low molecular weight heparin, always remembering that bleeding is an expected and manageable complication, whereas PTE can be a fatal and an unacceptable sequel in the context of elective surgery1,4.
There are few studies in the literature that show the true incidence of thromboembolic events, as most are based on retrospective studies. In addition, only about one third of the cases are symptomatic, which impairs the creation of protocols and recommendations for the proper treatment of VTW12.
This study presents several limitations, because it is a retrospective study that includes a relatively small, heterogeneous sample of patients after initiation of the protocol. However, it contributes positively to the existing literature. Larger, prospective studies are needed to conclude the efficacy, timing, and duration of chemoprophylaxis for patients undergoing plastic surgery. It can be concluded that adequate antithrombotic prophylaxis for patients undergoing abdominoplasty leads to lower morbidity/mortality and acute events, and hemorrhagic complications can be adequately managed.
COLLABORATIONS
TAJ Writing the manuscript or critical review of its contents.
ACCV Final approval of the manuscript; conception and design of the study.
GLD Final approval of the manuscript.
REFERENCES
1. Dini GM, Ferreira MC, Albuquerque LG, Ferreira LM. How safe is thromboprophylaxis in abdominoplasty? Plast Reconstr Surg. 2012;130(6):851e-857e. PMID: 23190837 DOI: http://dx.doi.org/10.1097/PRS.0b013e31826d9fc0
2. Ponteli EP, Scialom JM, Pontelli TEGS. Profilaxia tromboembólica farmacológica e por compressão pneumática intermitente em 563 casos consecutivos de abdominoplastia. Rev Bras Cir Plást. 2012;27(1):77-86. DOI: http://dx.doi.org/10.1590/S1983-51752012000100013
3. Anger J, Baruzzi ACA, Knobel E. Um protocolo de prevenção de trombose venosa profunda em cirurgia plástica. Rev Bras Cir Plást. 2003;18(1):47-54.
4. Hatef DA, Kenkel JM, Nguyen MQ, Farkas JP, Abtahi F, Rohrich RJ, et al. Thromboembolic risk assessment and the efficacy os enoxaparin prophylaxis in excisional body contouring surgery. Plast Reconstr Surg. 2008;122(1):269-79. DOI: http://dx.doi.org/10.1097/PRS.0b013e3181773d4a
5. Paiva RA, Pitanguy I, Amorim NFG, Berger R, Shdick HA, Holanda TA. Tromboembolismo venoso em cirurgia plástica: protocolo de prevenção na Clínica Ivo Pitanguy. Rev Bras Cir Plást. 2010;25(4):583-8. DOI: http://dx.doi.org/10.1590/S1983-51752010000400003
6. Colwell AS, Reish RG, Kuter DJ, Phil BD, Austen WG Jr, Fogerty AE. Abdominal contouring procedures increase activity of the coagulation cascade. Ann Plast Surg. 2012;69(2):129-33. DOI: http://dx.doi.org/10.1097/SAP.0b013e318226b38b
7. Koch A, Bouges S, Ziegler S, Dinkel H, Daures JP, Victor N. Low molecular weight heparin and unfractionated heparin in thrombosis prophylaxis after major surgical intervention: update of previous meta-analyses. Br J Surg. 1997 Jun;84(6):750-9. PubMed PMID: 9189079.
8. Munson CF, Reid AJ. Novel oral anticoagulants in plastic surgery. J Plast Reconstr Aesthet Surg. 2016;69(5):585-93. DOI: http://dx.doi.org/10.1016/j.bjps.2016.02.011
9. Gold A. Deep vein thrombosis chemoprophylaxis in plastic surgery. Clin Plastic Surg. 2013;40(3):399-404. DOI: http://dx.doi.org/10.1016/j.cps.2013.04.003
10. Reish RG, Damjanovic B, Colwell AS. Deep venous thrombosis prophylaxis in body contouring: 105 consecutive patients. Ann Plast Surg. 2012;69(4):412-4. PMID: 22964679 DOI: http://dx.doi.org/10.1097/SAP.0b013e31824a45e0
11. Pannucci CJ, Dreszer G, Wachtman CF, Bailey SH, Portschy PR, Hamill JB, et al. Postoperative enoxaparin prevents symptomatic venous thromboembolism in high-risk plastic surgery patients. Plast Reconstr Surg. 2011;128(5):1093-103. PMID: 22030491 DOI: http://dx.doi.org/10.1097/PRS.0b013e31822b6817
12. Miszkiewicz K, Perreault I, Landes G, Harris PG, Sampalis JS, Dionyssopoulos A, et al. Venous thromboembolism in plastic surgery: incidence, current practice and recommendations. J Plast Reconstr Aesthet Surg. 2009;62(5):580-8. PMID: 19264567 DOI: http://dx.doi.org/10.1016/j.bjps.2008.11.109
1. Hospital e Maternidade Celso Pierro, Pontifícia Universidade Católica de Campinas, Campinas, SP, Brazil
2. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
Institution: Hospital e Maternidade Celso Pierro, Campinas, SP, Brazil.
Corresponding author:
Thatiana Ambrogini Justino
Avenida John Boyd Dunlop, S/N - Jardim Ipaussurama
Campinas, SP, Brazil - Zip Code 13060-904
E-mail: thaty_ambro@hotmail.com
Article received: June 25, 2017.
Article accepted: December 5, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter