

Original Article - Year 2018 - Volume 33 -
High-definition laser-assisted lipoaspiration
Lipoaspiração laser-assistida de alta definição
ABSTRACT
INTRODUCTION: Since the introduction of the liposuction technique, the improvement of body contour has been gaining new horizons. Superficial liposuction has been used in favor of aesthetics; the use of technologies, such as VASER and diode laser at 915- and 980-nm wavelengths, helps reduce complications and improves post-time, healing time, and cutaneous retraction.
METHODS: Fourteen patients submitted to high-resolution laser lipolysis were studied between 2014 and 2016. The level of patient satisfaction regarding the treatment outcome was assessed.
RESULTS: The majority of the patients were men, with a mean age of 39 years and a mean pain score of 2.3 on the visual pain scale (0 to 10), presenting lasting results after 1 year, with no complications and an early return to work and physical activities.
CONCLUSIONS: The use of diode laser at the wavelengths of 915 and 980 nm in high-definition liposculpture promoted satisfactory, promising results and should be tested in a larger sample of patients.
Keywords: Lipolysis; Lipectomy; Lasers; Personal satisfaction; Aesthetics.
RESUMO
INTRODUÇÃO: Desde a introdução da técnica de lipoaspiração, a melhora do contorno corporal vem ganhando novos horizontes. O uso da lipoaspiração superficial passou a ser usado a favor da estética e, com isso, o uso de tecnologias, tais como o VASER e o laser de Diodo, nos comprimentos de 915 e 980 nn, diminuem as complicações, com melhora da dor pós-operatória, tempo de cicatrização e retração cutânea.
MÉTODOS: Foram estudados, inicialmente, 16 pacientes submetidos à laserlipólise de alta definição, entre o período de 2014 e 2016. O nível de satisfação em relação ao resultado foi questionado aos pacientes.
RESULTADOS: A maioria dos pacientes foi do sexo masculino, idade média 39 anos, com média de dor de 2,3 de na escala de visual de dor (0 a 10), apresentando resultados duradouros após 1 ano, sem complicações e retorno às suas atividades de trabalho e físicas precocemente.
CONCLUSÕES: Desta forma, o uso do laser de Diodo com comprimentos de ondas de 915 e 980nm, associado à Lipoescultura de Alta Definição, promoveu resultados satisfatórios, promissores devendo ser testado numa amostragem maior de pacientes.
Palavras-chave: Lipólise; Lipectomia; Lasers; Satisfação pessoal; Estética.
Improvements in body contour via fat removal have been constantly refined. Between 1970 and 1980, Schrudde published the use of a curette to remove fat in areas such as the lower limbs1,2. Illouz then published the use of blunt cannulas with holes for fat suction3. The initial problems of bleeding, unexpected aesthetic results, and difficult recovery have been resolved with the introduction of new compression loops and local anesthetics as used in the tumescent technique described by Hunstad4. The recent technological advances observed, such as the development of ultrasonic liposuction and vibrolipoaspiration, have yielded patient benefits, including reduction of tissue trauma and especially physical stress experienced by surgeons during the surgery5.
Athletes constantly complain that even if they perform physical activities, they cannot achieve defined abdominal muscles, i.e., the desired "washboard."
The traditional abdominal liposuction involves liposuction of the deep layer and usually leaves a layer of fat throughout the wall of the abdomen, preserving the subdermal fat, which minimizes irregularities. The treatment of this layer alone fails to reach the goal of a "tiny belly" because the subdermal fat disrupts the visibility of the muscular details6.
The superficial liposuction technique is performed using a thin cannula to refine the skin fold or groove; it was first reported by Illouz to improve the appearance of the infragluteal fold. It is a frequent cause of persistent grooves and sequelae, producing contour irregularities6,7.
In 1993, Mentz et al.6 published for the first time a work on high-definition liposuction for athletic men who could not define their abdominal muscles through bodybuilding and called it "abdominal etching," used only for the anterior wall of the abdomen and for patients with less than 15% fat in the body. In 1997, Ersek and Salisbury published their work, also of the same name, customized, and proposed a specific cannula design for superficial liposuction8.
Alongside traditional suction-assisted lipoplasty, other options include ultrasonic, vibratory, and laser lipoplasties. Studies on alternatives and new tools seek to reduce the downtime, operator effort, and bleeding, promote cutaneous retraction, and facilitate surgery in previously operated fibrotic areas9,10.
In 2003, Hoyos presented an improvement of the technique described by Mentz in the Bolivian National Congress, expanding its use to simulate all the muscles of the abdomen, back flanks, and legs, specifically pectorals in men and glutes in women, which denominated high-definition liposculpture (HDL). It was a breakthrough technique, but required highly trained surgeons for its accomplishment. The technique is exhausting for surgeons and very painful and traumatic for patients. The adverse consequences of the procedure include a slow recovery and prolonged edema11. In 2007, Hoyos and Millard12 published an association of VASER use with HDL.
The first studies on laser lipolysis were published by Apfelberg between 1992 and 1996 using the neodymiun yttrium aluminum garnet laser inside the cannula employed for liposuction13. Widely used in Europe and Latin America, laser lipolysis (also called laser lipoplasty) was introduced in North America in 199410,14 and approved by the Food and Drug Administration in October 200615-17.
The application of the laser in liposuction promotes a reduction of the mechanical trauma to the surrounding tissues, which results in less formation of fibrosis, reduced bleeding via coagulation of the blood vessels, less pain, and faster recovery, favoring postoperative comfort. In addition, immediate and late marked tissue retraction occurs via stimulation of collagen, which is better evaluated after the third postoperative month17-25. Minor complications, such as ecchymosis, edema, and temporary decrease in sensitivity in the operated region, burns, nodularities, and seromas, are correlated with the use of laser in liposculpture5,10,19,22,26-28.
The wavelengths 1064 nm and 980 nm are better absorbed by water than by fat. Between 900 nm and 950 nm, absorption in fat is greater than absorption in water. The fat absorption coefficient is seven times higher at 924 nm than at 1064 nm. Further, the water absorption peak is greater at 975 nm than at 1064 nm29,30.
OBJECTIVE
The purpose of this study was to evaluate the outcomes of diode laser at 915-nm and 980-nm wavelengths in HDL.
METHODS
In this study, we selected 14 patients treated by the same author using high-definition laser-assisted liposuction, starting in 2014. Only one patient had a sedentary lifestyle. Two patients who had less than 30 postoperative days were excluded. The mean age of the patients (eight men and six women) was 39 years (ranging from 23 to 64 years).
All patients were examined, and the risks and procedures were discussed. They underwent routine preoperative examinations, were released by the cardiologist, signed a preoperative consent form, and authorized the disclosure of their surgical results. The study followed the rules of the Declaration of Helsinki, and there are no conflicts of interest.
Some patients underwent combined surgeries. Patient 3 underwent mammaplasty with prosthesis implantation and abdominoplasty scar retouching; patient 6 underwent pectoral prosthesis implantation, rhinoplasty, and gynecomastia surgery; patient 10 underwent facial minilifting; and patient 13 underwent plicature of the aponeurosis of the rectus abdominis muscle.
Detailed preoperative markings were performed with the patients in the orthostatic position. The patients were asked to flex and contract their abdominal muscles to help define the details of the musculature. The medial and lateral areas of the rectus abdominis muscle were marked on the linea alba and semilunaris. The transverse interstices of the rectus abdominis muscle were also marked separately. With the patients on their back, the flanks and back were delimited (Figure 1).

Figure 1. Preoperative markings.
The patients were anesthetized, intubated, and left with an artificial ventilatory support and wore surgical compression socks and intermittent external pneumatic compression device in the legs (Phlebo Press® DVT, Mego Afek, Israel). All of them received antimicrobial prophylaxis with 2 g cefazolin at the anesthetic induction or up to 1 hour before surgery and were positioned first in the ventral horizontal decubitus for treatment of the posterior region. The areas to be treated were then degermed using chlorhexedine degermant and antiseptic solution consisting of chlorhexedine alcohol.
Punctures were performed using scalpel blade n15 in the upper medial intergluteal region and lumbar medians to access the flanks. In case treatment of the upper dorsal region was needed, two other punctures were performed on each side, one medial and another superolateral to the region.
The anesthetic solution used was uniformly distributed xylocaine (0.05 to 0.1%) with adrenaline (1: 1000) at a concentration of 1: 250,000 U/mL using a Klein needle.
Fibers of 600-800 nm in diameter and initially at the wavelength of 915 nm were used for lipolysis, continuous pulse, and individualized potency according to the medical evaluation and treatment protocols of the device manufacturer (Delight®, Vydence Medical, Brazil) (Figure 2).

Figure 2. Delight® apparatus - Vydence Medical.
Thereafter, liposuction was performed using a Mercedes curved cannula and 3-mm straight vacuum connected to the aspirator (Medela Dominant 50®, Switzerland) and adjusted to a vacuum pressure of 50 cmHg. The pinch test was performed to assess the thickness of the residual subcutaneous tissue.
The wavelength of 980 nm was then fired in the treated regions to promote tissue contraction.
The proportions between the 915- and 980-nm wavelengths were inconstant and dependent on the main action that the operator most preferred, individually defined lipolysis or cutaneous retraction.
Mononylon 5.0 sutures and occlusive dressings (Terracortril®) were used.
The patients were then moved to the dorsal horizontal position and inserted with a bladder catheter for relief or delay and after new asepsis and antisepsis, performed bilaterally on the pubic bone bilaterally, superiorly and within the umbilical scar, another in the upper region of the linea alba, and another 2 on each side, in the semilunar lines, for the treatment of the transverse inscriptions of the rectus abdominis, external oblique, and anterior serratus muscles.
After infusion of the solution, the same sequence of procedures described above was performed, seeking to intensify the markings of the muscular limits superficially.
After finishing the treatments, closing the punctures, and applying dressings, the patients were applied with a compression mesh.
After an average of 6 to 8 hours postoperatively under appropriate conditions, the patients were discharged with antibiotic prophylaxis for another 4 days (cefadroxil 500 mg) and analgesics, such as dipyrone or codeine in combination with paracetamol.
The chemoprophylaxis for deep venous thrombosis with low molecular weight heparin (enoxaparin) was analyzed in each case, i.e., whether with risk factors, longer surgical time and longer recovery time, prolonged trips before or after the procedure, at a dose of 40 mg per day for 7 days. The compression stockings were used for a mean of 1 to 7 postoperative days.
The first follow-up was performed on the first postoperative day to start the treatment with lymphatic drainage and electric current ultrasound (Manthus®, KLD Biosistemas, Brazil), ranging from 10 to 20 sessions, based on the presence of local edema and swallowing condition.
The stitches were removed between 7 and 12 days postoperatively, and the micropore was maintained up to 3 months in the evident scars.
The majority of the patients were allowed to perform physical activities after 7 days.
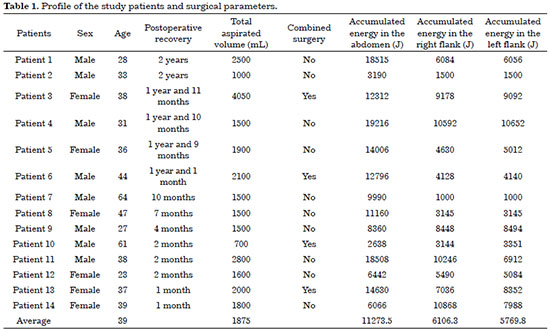
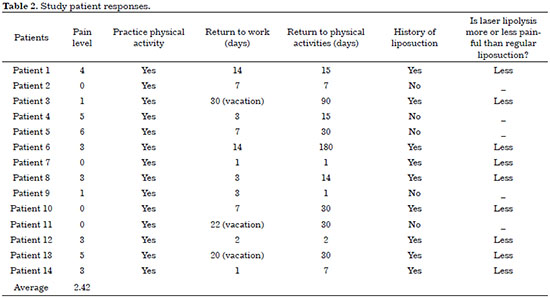
To evaluate the results, a questionnaire regarding expectations and postoperative satisfaction was prepared, which was delivered and answered by the patients personally or via e-mail (Tables 1 and 2).
RESULTS
Ten patients underwent only high-definition laser liposuction. All of them were discharged on the same day; those who were working returned to work after an average of 4.25 days and physical activities after an average of 12.2 days. The patients who underwent combined surgeries had to return to work and physical activities late. The average aspirated volume was 1875 mL, ranging from 700 mL to 2800 mL.
The average accumulated energy delivered by the optical fiber was 11273.5 J in the abdomen and 6106.3 J and 5769.8 J in the right and left flanks, respectively (Table 1).
The mean pain score was 2.42 (on a scale of 0 to 10; ranging from 0 to 6). Eight patients had more than 6 months of follow-up. Of them, two (25%) reported having lost the aesthetic result because they had gained weight. One of these eight patients became pregnant before completing 1 year of postoperative follow-up and stated that she did not lose the result despite her pregnancy.
No seroma was detected in any of the patients studied. There were no serious bruises. Only small bruises were observed in nine patients (69.23%).
All 14 patients in this study were satisfied. Twelve patients (85.71%) reported higher than expected results, and two (14.28%) stated that their results adequately met their expectations. All indicated that they would undergo the same procedure if necessary (Table 2). All patients who had already underwent liposuction using only cannulas previously (9) stated that the procedure using laser was less painful.
No patient had skin burns. Some had dyschromias in the puncture site due to the friction of the liposuction cannula, but did not express a desire to touch up the scars. In sequence, some cases are reported in Figures 3 to 7.
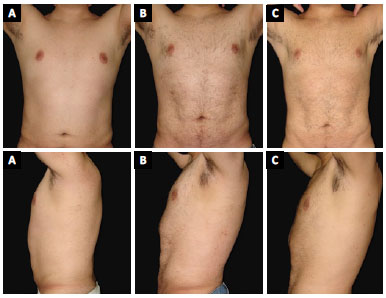
Figure 3. Patient 1. A: Preoperative; B: 3-months postoperative; C: 1-year postoperative.
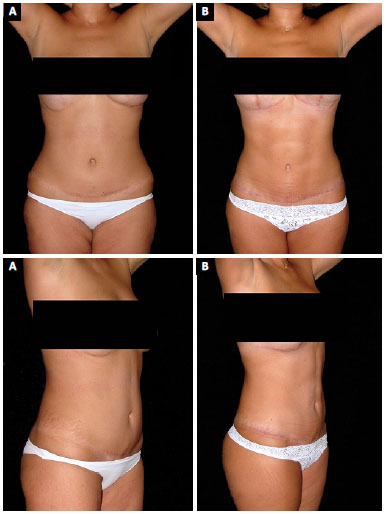
Figure 4. Patient 3. A: Preoperative; B: 6-months postoperative.
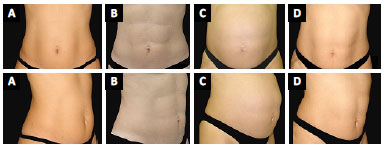
Figure 5. Patient 5. A: Preoperative; B: 2-months postoperative; C: Postoperative period of 1.4 years and 26 weeks and 4 days of gestation; D: 3-months puerperium.

Figure 6. Patient 7. A: Preoperative; B: 9-months postoperative.
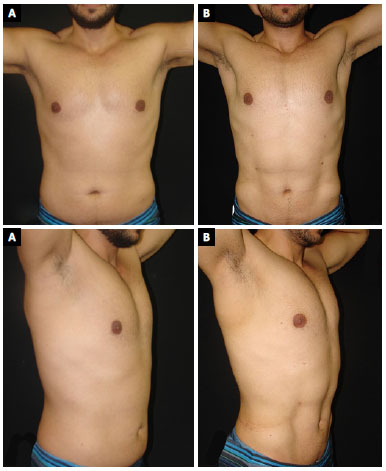
Figure 7. Patient 9. A: Preoperative; B: 3-months postoperative.
DISCUSSION
Lipoplasty of the deep layer only does not achieve the desired "taupe belly" result in patients. The increasing search for an athletic body has been demanding among professionals, using their labor skills and more advanced techniques to improve the results. Surface layer treatment is necessary to optimize results6.
In this study, diode laser at the wavelengths of 915 and 980 nm using a high-definition technique was employed.
These wavelengths in laser lipolysis led to fat liquefaction and vessel coagulation, reducing bleeding, trauma, pain, edema, and cutaneous retraction, preventing increased sagging, mainly supraumbilical sagging, decreasing the "downtime" among patients, and finally allowing an early return to their physical activities5,9,10,14,17,20.
In 2007, Hoyos and Millard12 presented that their VASER-assisted high-resolution liposculpture achieved an 84% satisfaction rate among their patients. Seromas were observed in 6.5% of cases and resolved with punctures. The use of drains was standardized for 48 to 72 hours. Of the 306 cases, 3.92% presented a loss of definition.
The results were persistent during pregnancy in the study by Hoyos and Millard12 as in our study.
Regarding pain on a scale of 1 to 5, Hoyos and Millard12 published a scale between 3 and 4. In this sample, the mean score was 2.42 (on a scale of 0 to 10). In the study by Dornelles et al. in which laser lipolysis at 980 nm was used in 400 cases, patients who have had an experience with cannulated liposuction have reported postoperative evolution with less pain and recovery of a more rapid discomfort compared with their previous experience. The action of the laser in the innervation surrounding the path of the laser fiber promotes paresthesia and even transient anesthesia, making the postoperative period more comfortable5. In agreement with our observations, the findings of these studies are in favor of the lower index of pain and faster recovery using laser in lipoplasty.
The technique presented here, specifically for those patients who want to have a highly defined and athletic-looking abdomen, showed minimal risks. Despite the increase in the duration of the procedure, the thermomechanical energy of the laser seemed to reduce the risks of complications, such as bleeding and hemodynamic changes, although we were not able to affirm this because these factors were not part of this study. Abdelaal and Aboelatta24 conducted laboratory studies in supernatants of liposuction on the side where laser-assisted liposuction was performed and reported that there was a 50% reduction in the amount of hemoglobin and red blood cell loss. Badin et al.25 histologically analyzed the region submitted to the laser and also showed decreased bleeding.
The patient satisfaction exceeded the expectations in the study cohort. With proper patient selection and use of the high-definition laser-assisted technique, improved sculpting the abdomen can be achieved, enhancing natural folds, defining muscular contours, and achieving a larger and more natural cutaneous retraction than that in deep lipoplasty.
In the study by Mentz et al.6 regarding superficial layer treatment in specific anatomical regions, they concluded that this treatment could be used for specific patients who want to have a muscular abdomen and could exceed expected satisfaction. Ersek and Salisbury8 concluded that sculpting the abdominal musculature promotes a high level of outcome for experienced plastic surgeons. Holes and Millard12 concluded that this definition can reach an audience that had never thought about undergoing a body contouring procedure but would seek to achieve definitions in the body they could not achieve with diets and exercises.
In our study, two patients were older than 60 years and demonstrated that the desire to have a "small abdomen" is not restricted to young men, as also evidenced in the study by Hoyos and Millard12.
In the analysis of 534 laser lipolysis procedures by Reynaud et al.10 in 2009, 83% of patients reported no pain or discomfort in the first week, and 17% reported average pain or discomfort. Some of the study patients underwent aspiration after laser lipolysis.
Moreno-Moraga and Royo de La Torre21 also demonstrated a low pain intensity and level of satisfaction, and more than 80% of patients achieved their expectation after laser lipolysis.
In 2013, Senra22 published in his study on laser lipolysis that 96% of patients considered their results as satisfactory and that the complaints of pain were discrete.
Coinciding with our observations, the findings of these studies are in favor of a lower pain index and faster recovery using laser in lipoplasty.
However, comparative studies between VASER and diode laser are needed. It was not found, also other works, using the laser in the technique of HDL.
Although the technique presents a high learning curve and a longer surgical time, the recovery of the patients without combined surgeries was fast, with an early return to their work and physical activities.
The use of diode laser at the wavelengths of 915 and 980 nm in HDL yielded satisfactory outcomes.
COLLABORATIONS
RPM Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
REFERENCES
1. Schrudde J. Lipektomie und Lipexhaerese im Bereich der unteren Extremitäten. Langenbecks Arch Chir. 1977;345(1):127-31. DOI: http://dx.doi.org/10.1007/BF01305460
2. Schrudde J. Lipexeresis as a means of eliminating local adiposity. Aesthetic Plast Surg. 1980;4(1):215-26. DOI: http://dx.doi.org/10.1007/BF01575221
3. Illouz YG. Surgical remodeling of the silhouette by aspiration lipolysis or selective lipectomy. Aesthetic Plast Surg. 1985;9(1):7-21. PMID: 2986432 DOI: http://dx.doi.org/10.1007/BF01570678
4. Hunstad JP. Tumescent and syringe liposculpture: a logical partnership. Aesthetic Plast Surg. 1995;19(4):321-33. PMID: 7484470 DOI: http://dx.doi.org/10.1007/BF00451658
5. Dornelles RFV, Silva AL, Missel J, Centuriôn P. Laserlipólise com diodo 980 nm: experiência com 400 casos. Rev Bras Cir Plast. 2013;28(1):124-9. DOI: http://dx.doi.org/10.1590/S1983-51752013000100021
6. Mentz HA 3rd, Gilliland MD, Patronella CK. Abdominal etching: differential liposuction to detail abdominal musculature. Aesthetic Plast Surg. 1993;17(4):287-90. DOI: http://dx.doi.org/10.1007/BF00437100
7. Illouz YG. Surgical implications of "fixed point": a new concept in plastic surgery. Aesthetic Plast Surg. 1989;13(3):137-44. PMID: 2801294 DOI: http://dx.doi.org/10.1007/BF01570210
8. Ersek RA, Salisbury AV. Abdominal etching. Aesthetic Plast Surg. 1997;21(5):328-31. PMID: 9298999 DOI: http://dx.doi.org/10.1007/s002669900131
9. Goldman A. Submental Nd:Yag laser-assisted liposuction. Lasers Surg Med. 2006;38(3):181-4. PMID: 16453321 DOI: http://dx.doi.org/10.1002/lsm.20270
10. Reynaud JP, Skibinski M, Wassmer B, Rochon P, Mordon S. Lipolysis using a 980-nm diode laser: a retrospective analysis of 534 procedures. Aesthetic Plast Surg. 2009;33(1):28-36. PMID: 18972152 DOI: http://dx.doi.org/10.1007/s00266-008-9262-3
11. Manzaneda Cipriani R. Lipomarcación de alta definición: reporte de dos casos. Horiz Med [Internet]. 2015;15(2):70-5. [citado 2016 Ago 20]. Disponível em: http://www.redalyc.org/articulo.oa?id=371641084011
12. Hoyos AE, Millard JA. VASER-assisted high-definition liposculpture. Aesthet Surg J. 2007;27(6):594-604. DOI: http://dx.doi.org/10.1016/j.asj.2007.08.007
13. Apfelberg DB, Rosenthal S, Hunstad JP, Achauer B, Fodor PB. Progress report on multicenter study of laser-assisted liposuction. Aesthetic Plast Surg. 1994;18(3):259-64. DOI: http://dx.doi.org/10.1007/BF00449791
14. Mordon S, Eymard-Maurin AF, Wassmer B, Ringot J. Histologic evaluation of laser lipolysis: pulsed 1064-nm Nd:YAG laser versus cw 980-nm diode laser. Aesthet Surg J. 2007;27(3):263-8. DOI: http://dx.doi.org/10.1016/j.asj.2007.03.005
15. Tagliolatto S, Medeiros VB, Leite OG. Laserlipólise: atualização e revisão da literatura. Surg Cosmet Dermatol. 2012;4(2):164-74. [citado 2016 Ago 12]. Disponível em: http://www.surgicalcosmetic.org.br/detalhe-artigo/203/Laserlipolise--atualizacao-e-revisao-da-literatura
16. Katz B, McBean J, Cheung JS. The new laser liposuction for men. Dermatol Ther. 2007;20(6):448-51. DOI: http://dx.doi.org/10.1111/j.1529-8019.2007.00160.x
17. Tagliolatto S, Medeiros VB, Teresani PCS, Leite OG, Filipe JV, Mazzaro CB, et al. Experiência em laserlipólise: casuística de 120 casos no período de 2004 a 2010. Surg Cosmet Dermatol. 2011;3(4):282-7. [citado 2016 Ago10]. Disponível em: http://www.redalyc.org/articulo.oa?id=265522077004
18. Prado A, Andrades P, Danilla S, Leniz P, Castillo P, Gaete F. A prospective, randomized, double-blind, controlled clinical trial comparing laser-assisted lipoplasty with suction-assisted lipoplasty. Plast Reconstr Surg. 2006;118(4):1032-45. PMID: 16980867 DOI: http://dx.doi.org/10.1097/01.prs.0000232428.37926.48
19. Goldman A, Wollina U, de Mundstock EC. Evaluation of Tissue Tightening by the Subdermal Nd: YAG Laser-Assisted Liposuction Versus Liposuction Alone. J Cutan Aesthet Surg. 2011;4(2):122-8. DOI: http://dx.doi.org/10.4103/0974-2077.85035
20. Mordon SR, Wassmer B, Reynaud JP, Zemmouri J. Mathematical modeling of laser lipolysis. Biomed Eng Online. 2008;7(10):1-13. [citado 2016 Set 18]. Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2292728/pdf/1475-925X-7-10.pdf DOI: http://dx.doi.org/10.1186/1475-925X-7-10
21. Moreno-Moraga J, Royo de La Torre J. Our experience treating 500 lipodystrophic areas with a 924/975 nm laser, a new device that induces lipolysis and heating of the dermis and fibrous septa of fatty tissue. J Clin Dermatol. 2010;1(2):1-10. [citado 2016 Set 18]. Disponível em: https://www.researchgate.net/publication/268062696_Our_Experience_Treating_500_Lipodystrophic_Areas_with_a_924975_nm_Laser_a_New_Device_That_Induces_Lipolysis_and_Heating_of_the_Dermis_and_Fibrous_Septa_of_Fatty_Tissue
22. Senra AB. Avaliação de 10 anos de laserlipólise em 766 pacientes. Rev Bras Cir Plást. 2013;28(3):389-97.
23. Wolfenson M, Roncatti C, Alencar AH, Barros T, Silva Neto JF, Santos Filho FCN. Laserlipólise: redução da pele e prevenção de umbigo flácido nas lipoplastias seguindo parâmetros de segurança no uso do laser de diodo - com duplo comprimento de onda 924 e 975 nm. Rev Bras Cir Plást. 2011;26(2):259-65.
24. Abdelaal MM, Aboelatta YA. Comparison of Blood Loss in Laser Lipolysis vs Traditional Liposuction. Aesthet Surg J. 2014;34(6):907-12. DOI: http://dx.doi.org/10.1177/1090820X14536904
25. Badin AZ, Gondek LB, Garcia MJ, Valle LC, Flizikowski FB, de Noronha L. Analysis of laser lipolysis effects on human tissue samples obtained from liposuction. Aesthetic Plast Surg. 2005;29(4):281-6. DOI: http://dx.doi.org/10.1007/s00266-004-0102-9
26. Sasaki GH, Tevez A. Laser-assisted liposuction for facial and body contouring and tissue tightening: a 2-year experience with 75 consecutive patients. Semin Cutan Med Surg. 2009;28(4):226-35. DOI: http://dx.doi.org/10.1016/j.sder.2009.10.003
27. Gentileschi S, Servillo M, D'Ettorre M, Salgarello M. Abdominal Subcutaneous Mass After Laser-Assisted Lipolysis and Immediate Multiple Treatments with a Dual-Wavelength Laser, Vacuum and Massage Device. Aesthet Surg J. 2016;36(4):NP144-9. DOI: http://dx.doi.org/10.1093/asj/sjv248
28. Palm MD, Goldman MP. Laser lipolysis: current practices. Semin Cutan Med Surg. 2009;28(4):212-9. DOI: http://dx.doi.org/10.1016/j.sder.2009.10.002
29. Anderson RR, Farinelli W, Laubach H, Manstein D, Yaroslavsky AN, Gubeli J 3rd, et al. Selective photothermolysis of lipid-rich tissues: a free electron laser study. Lasers Surg Med. 2006;38(10):913-9. PMID: 17163478 DOI: http://dx.doi.org/10.1002/lsm.20393
30. Khoury JG, Saluja R, Keel D, Detwiler S, Goldman MP. Histologic evaluation of interstitial lipolysis comparing a 1064, 1320 and 2100 nm laser in a ex vivo model. Lasers Surg Med. 2008;40(6):402-6. DOI: http://dx.doi.org/10.1002/lsm.20649
Belledevi Plástica & Dermatologia, São José do Rio Preto, SP, Brazil
Institution: Belledevi Plástica & Dermatologia, São José do Rio Preto, SP, Brazil.
Corresponding author:
Rodrigo Pinheiro Motta
Avenida Murchid Homsi, 2200, 7 andar - Quinta das Paineiras
São José do Rio Preto, SP, Brazil - Zip Code 15080-325
E-mail: drrodrigo@belledevi.com.br
Article received: March 14, 2017.
Article accepted: January 26, 2018.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter