

Original Article - Year 2018 - Volume 33 - Issue 1
Reconstruction of the abdominal wall: a case series
Reconstrução de parede abdominal: série de casos
ABSTRACT
INTRODUCTION: Patients with abdominal wall defects present challenging complications that require the use of advanced surgical approaches.
METHODS: This primary, retrospective, and descriptive study evaluated patients who underwent abdominal wall reconstruction at the Plastic Surgery Service of the Clinics Hospital of the Federal University of Pernambuco.
RESULTS: The medical records of 18 patients were reviewed, including 15 women (83.3%) and 3 men (16.7%), with a mean age of 41 years (range, 16-79 years). Seventeen patients (94.4%) had a history of previous surgery. The causes of abdominal injury were cesarean section in eight cases (44.4%), oncologic surgery in six (33.3%), trauma surgery in two (11.1%), and bariatric surgery in two (11.1%). The etiology of the defect was necrotizing fasciitis in eight cases (44.4%), incisional hernia in four (22.2%), trauma in two (11.1%), surgical wound dehiscence in two (11.1%), abdominal wall neoplasia in two (11.1%), and total thickness defect in one (5.5%). The surgical interventions included the component separation technique in seven cases (38.9%), simple VY advancement flap in six (33.3%), closure with abdominoplasty in three (16.7%), and tissue expander in two (11.1%). Four patients (22.2%) presented complications.
CONCLUSIONS: Abdominal wall defects are challenging cases for plastic surgeons, as their treatment is difficult, but the results are satisfactory even in the most severe cases.
Keywords: Abdominal wall; Reconstruction; Necrotizing fasciitis; Abdominal hernia; Ventral hernia.
RESUMO
INTRODUÇÃO: Os pacientes com defeitos de parede abdominal chegam ao consultório do cirurgião plástico em situações muitas vezes complexas, necessitando de abordagem cirúrgica avançada.
MÉTODOS: Estudo primário, retrospectivo e descritivo de pacientes submetidos a procedimentos cirúrgicos de reconstrução de parede abdominal pelo Serviço de Cirurgia Plástica do Hospital das Clínicas da Universidade Federal de Pernambuco (HC-UFPE).
RESULTADOS: Foram revisados e incluídos os prontuários de 18 pacientes, 15 (83,3%) do sexo feminino e 3 (16,7%) do masculino, com idade variando de 16 a 79 anos (média de 41 anos). Dezessete pacientes possuíam histórico de cirurgia prévia (94,4%), sendo a cesárea presente em 8 dos casos (44,4%), seguida de cirurgia oncológica com 6 (33,3%), cirurgia do trauma com 2 (11,1%) e bariátrica com 2 (11,1%). Em relação à etiologia do defeito, 8 (44,4%) eram decorrentes de fasciite necrosante, 4 (22,2%) de hérnia incisional, 2 (11,1%) por trauma, 2 (11,1%) por infecção de ferida operatória e 2 (11,1%) por neoplasia de parede abdominal, sendo somente um (5,5%) paciente com defeito de espessura total. A técnica cirúrgica de separação dos componentes foi realizada em 7 dos casos (38,9%), seguida de retalho de avanço simples em 6 (33,3%), fechamento com tela associado à abdominoplastia em 3 (16,7%), e expansor tecidual em 2 (11,1%). Quanto às complicações, houve 4 casos (22,2%).
CONCLUSÕES: Defeitos de parede abdominal são casos desafiadores para o cirurgião plástico, seu tratamento se mostra árduo, porém com resultados satisfatórios mesmo nos casos mais severos.
Palavras-chave: Parede abdominal; Reconstrução; Fasciite necrosante; Hérnia abdominal; Hérnia ventral.
Patients with abdominal wall defects have challenging complications that require the use of advanced surgical approaches. Surgical reconstruction has different levels of complexity, from minor tissue loss (Figure 1) to total thickness defects with visceral involvement (Figure 2). The causes of abdominal injury include hernias (Figure 3), infection (Figures 1 and 2), trauma, and sequelae of neoplasia treatment (Figure 4)1,2.
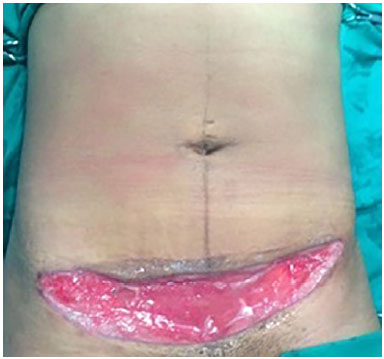
Figure 1. Necrotizing fasciitis with partial thickness involvement of the abdominal wall.

Figure 2. Necrotizing fasciitis with total thickness involvement of the abdominal wall.

Figure 3. Incisional hernia.

Figure 4. Defect resulting from excision of an abdominal wall sarcoma.
The main surgical goals should include restoration of the function and integrity of the musculofascial wall, obtaining a stable skin cover of soft tissues, and aesthetic optimization1,3. Surgical treatment varies according to the etiology and extent of the defect, and several surgical techniques are available, usually associated with the placement of surgical meshes. For small defects, simpler options can be used, including primary synthesis, grafts, and local and regional flaps.
The surgical procedures available for treating defects of moderate to large size include progressive pneumoperitoneum, first described by Goñi-Moreno in 1947; the Lázaro da Silva technique, described in 1971; and the component separation technique, described by Ramirez. Furthermore, abdominal wall transplantation is possible in complex cases4-7.
In the Clinics Hospital of the Federal University of Pernambuco (Hospital das Clínicas da Universidade Federal de Pernambuco-HC-UFPE), the number of patients referred to the Plastic Surgery Service for abdominal wall reconstruction has increased. Therefore, determining the profile of these patients is necessary to understand their care needs and improve the therapeutic approach.
OBJECTIVE
To describe a series of cases of patients with abdominal wall defects who underwent reconstructive surgery at the Plastic Surgery Service of HC-UFPE.
METHODS
This primary, retrospective, and descriptive study evaluated patients who underwent abdominal wall reconstruction at the Plastic Surgery Service of HC-UFPE, Recife, Pernambuco, Brazil. The records of patients who underwent operation between June 2011 and June 2017, regardless of the etiology and extent of the defect and the surgical reconstruction technique used, were analyzed, provided these patients maintained a suitable outpatient follow-up. The patients who missed follow-up were excluded from the study.
The evaluated data included sex, age, comorbidities, surgical history, smoking, etiology and depth of the defect, treatment, and complications. The study complied with the principles of the Declaration of Helsinki (2000) and Resolution 196/96 of the National Health Council. The study was approved by the research ethics committee of our institution under Certificate for Ethics Assessment (Certificado de Apresentação para Apreciação Ética-CAAE) No. 71479317.0.0000.5208 and Opinion No. 2.283.186.
RESULTS
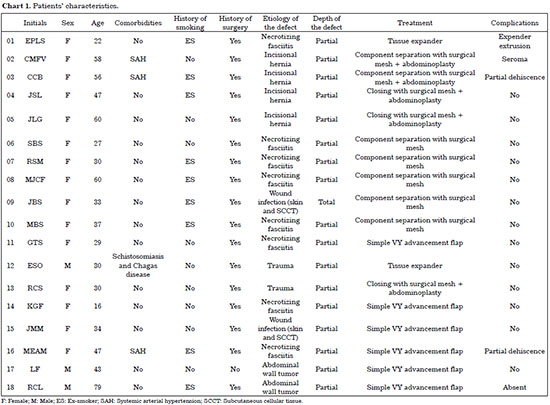
The medical records of 19 patients, including 15 women (83.3%) and 3 men (16.7%), with a mean age of 41 years (range, 16-79 years), were reviewed (Chart 1). Of the study participants, three (16.7%) presented systemic arterial hypertension; one (5.5%), Chagas disease; and one (5.5%), schistosomiasis. None of the participants were active smokers at the time of the surgical procedure. However, nine patients (50%) had a previous history of smoking and 17 (94.4%) had a history of previous surgery. The causes of abdominal injury were cesarean section in eight cases (44.4%), oncologic surgery in six (33.3%), trauma surgery in two (11.1%), and bariatric surgery in two (11.1%).
The etiology of the abdominal wall defect included necrotizing fasciitis (NF) in eight cases (44.4%), incisional hernia in four (22.2%), trauma in two (11.1%), surgical wound dehiscence in two (11.1%), and abdominal wall neoplasia in two (11.1%). Only one patient (5.5%) presented a total thickness defect. The surgical interventions included the component separation technique in seven cases (38.9%), placement of a simple VY advancement flap in six (33.3%), closure with a surgical mesh + abdominoplasty in three (16.7%) and use of a tissue expander in two (11.1%).
Some patients underwent more than one therapeutic approach, and abdominoplasty was associated with surgical reconstruction in four cases (22.2%). Four patients (22.2%) presented complications, including surgical wound dehiscence in two (11.1%), tissue expander extrusion in one (5.5%), and seroma in one (5.5%).
DISCUSSION
The development of surgical reconstruction of the abdominal wall arose from the need to approach complex cases that required the use of advanced surgical techniques2. The causes of abdominal injuries may include hernias, infections, trauma, and sequelae of treatment of neoplasias1,2.
In contrast to the results of previous studies, which reported that incisional hernia was the main cause of abdominal wall defect, the primary cause found in this series was NF (44.4% of the cases), and all these cases were associated with recently performed cesarean sections. However, this atypical finding is because of an outbreak of NF in the obstetric center of HC-UFPE2,8. Surgical treatment varied according to the etiology and extent of the defect. Barbosa et al.9 found that in the presence of abdominal flaccidity, abdominoplasty was performed in association with surgical reconstruction to improve the final aesthetic result (Figures 5 to 7).

Figure 5. Abdominoplasty combined with abdominal wall reconstruction.

Figure 6. Abdominoplasty combined with abdominal wall reconstruction.

Figure 7. Abdominoplasty combined with abdominal wall reconstruction.
Hernias, which is the main etiological factor of abdominal wall defects, can be treated using a wide variety of approaches. The main treatment approach for small hernial defects is primary synthesis. For moderate to large defects, placement of an alloplastic mesh in the anterior or posterior plane combined with laparoscopic or open surgery can be used. The mesh should be chemically inert, be able to withstand mechanical stress, and not cause foreign body reactions, carcinogenesis, or allergies10. Surgical meshes are made of different materials, including polytetrafluoroethylene and polyester; polypropylene is the most frequently used and is considered safe. However, the drawback of using surgical meshes is the possibility of infections and/or extrusion2,8.
In complex cases, including large hernias with loss of domicile, prior tissue expansion may be necessary, including progressive pneumoperitoneum, which was first described by Goñi-Moreno in 1947. This technique consists of introducing atmospheric air into the abdominal cavity by using a Veress needle in multiple sessions, with gradual expansion of the abdominal wall and posterior reconstruction of the wall with synthesis by planes and placement of the surgical mesh1,3.
Another option for treating these types of hernias, particularly those with mature and elastic hernia sacs, is the Lázaro da Silva technique, which was initially described in 1971. This procedure involves the use of flaps of the hernial sac and anterior and posterior leaflets of the rectus abdominis muscle, with a total of six flaps. A combined suture technique is used to avoid compartment syndrome and allow the use of a surgical mesh1.
However, designated component separation, the technique used in 38.9% of the reconstructions and first described by Ramirez (Figure 4) and indicated for moderate to large defects, is considered effective and safe because it follows the dynamics of the abdominal wall muscles, separating the rectus abdominis muscle from its posterior leaflet and the external oblique muscle, increasing the mobilization of these components and decreasing tension after suturing; this dynamics can be reinforced by placing a surgical mesh1,2,5,11.
In 2010 and 2012, Barbosa et al. published a series of cases (12 and 10, respectively) reconstructed with this technique. The authors reported that this technique is versatile and be used for several types of defect, with only one case of seroma in each series and no case of late complications, demonstrating the safety of the technique12.
Therefore, in our service, small to moderate hernia defects are usually resolved by the general surgery team. However, for major defects, the component separation technique combined with placement of a surgical mesh with or without abdominoplasty tends to be used, depending on the indication, because this combined technique provides excellent results and low complication rates.
Defects due to infections may include partial loss limited to the skin and, in extreme cases, NF (Figure 8), which was the main etiology in our series. NF is an infection that affects the superficial fascias of the abdomen, perineum, and genitalia, and can reach the deep fascia. NF is triggered by accidental or surgical trauma in most cases but was caused primarily by cesarean section in our series. The main comorbidity associated with this condition is diabetes mellitus; however, this complication was not observed in our series1.

Figure 8. Necrotizing fasciitis.
The primary treatment of active infection is early surgical debridement and antibiotic therapy. However, the established sequelae can be treated using different techniques, including primary synthesis; placement of grafts, local or regional flaps, or expanders; and vacuum therapy1-3.
In our service, for minor and superficial defects, cutaneous grafting and/or local or regional flap placement tends to be used. However, in larger or deeper defects, the adopted strategies included tissue expansion before making a flap, or component separation and placement of a surgical mesh. Vacuum therapy is used depending on the indication and availability in the hospital because of the high cost.
Other etiological factors of abdominal wall defects are substance losses due to local trauma and sequelae of neoplastic treatment. These defects may be treated using different strategies, but the use of local and regional flaps is more common. The use of flaps is satisfactory, especially in cases of deep defects such as those involving the rectus abdominis muscle for contralateral defects and the fasciocutaneous muscle of the tensor fascia lata or cutaneous muscle of the rectus femoris for defects of the lower region.
These types of reconstructions promote a significant volume gain and reinforcement of the abdominal wall. The disadvantages are defects in the donor area and the need to make skin grafts for flap coverage1. Therefore, the choice of the ideal flap depends on several factors, including the location, depth, and extent of the defect, and the status of the surgical bed; and the risk-benefit ratio of each modality should be weighed.
Abdominal wall reconstruction surgeries continue to be challenging, and complication and recurrence rates range from 20% to 63%2,13. The number of patients with complications found in our series (4, 22.2%) was similar to that found in previous studies (Figures 9 and 10). Two patients had a high body mass index, of whom one had an abdominal scar (Figure 11). This complication may have been the cause of the impairment of the distal irrigation of the abdominal cutaneous flap. However, surgery was justified by the negative effect of hernia on the quality of life, including interfering with work activities, family functions, and ambulation2. In view of the partial exposure of the surgical mesh and the possibility of mesh loss in one case, it was decided to initiate vacuum therapy after granulation was observed. Therefore, a skin graft was performed to improve the scar tissue and aesthetic result.

Figure 9. Extrusion of the tissue expander.

Figure 10. Surgical wound dehiscence with partial exposure of the surgical mesh.
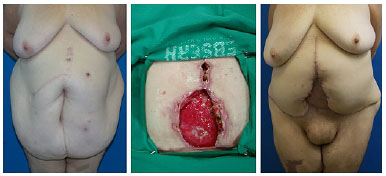
Figure 11. Surgical wound dehiscence with partial exposure of the surgical mesh and treatment with vacuum therapy and skin graft.
In one patient (Figure 9), the lack of cooperation associated with the discontinuation of follow-up after placement of the tissue expander resulted in the extrusion of the expander. For this reason, the surgical team decided to advance the skin flap as much as possible, and a skin graft was placed on the bloody remains, thus resolving the case. It is important to note that all these patients were former smokers. However, a previous study indicated that not smoking for at least 4 weeks before the procedure and up to 4 weeks after surgery achieved healing and complication rates similar to those of subjects who never smoked14.
CONCLUSION
Abdominal wall defects are challenging cases for the plastic surgeon and can lead to aesthetic and functional problems to the patient. The treatment of these defects is difficult, but the results are satisfactory even in the most severe cases. Therefore, there is no ideal reconstructive technique for each type of defect. However, the risk-benefit ratio of each strategy should be weighed, with thorough analysis of the context, including social and aesthetic issues, to increase the chances of success.
COLLABORATIONS
KK Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
ICGL Analysis and/or interpretation of data; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
PSL Final approval of the manuscript; writing the manuscript or critical review of its contents.
RA Final approval of the manuscript; writing the manuscript or critical review of its contents.
MBL Final approval of the manuscript; writing the manuscript or critical review of its contents.
REFERENCES
1. Alves JCRR, Silva Filho AF, Pereira NA, Ferrer KS, Carvalho EES. Reconstrução da parede abdominal. In: Melega JM, ed. Cirurgia Plástica: Fundamentos e Arte. Cirurgia Reparadora de Tronco e Membros. Rio de Janeiro: Guanabara Koogan; 2003. p. 242-55.
2. Singh NK, Khalifeh MR, Bank J. Reconstrução Abdominal. In: Neligan PC, Chang J, eds. Cirurgia Plástica, Volume 4. Extremidade Inferior, Tronco e Queimaduras. Rio de Janeiro: Elsevier Saunders; 2015. p. 279-96.
3. Dumanian GA. Abdominal Wall Reconstruction. In: Thorne CH, Bartlett SP, Beasley RW, Aston SJ, Gurtner GC, Spear SL, eds. Grabb and Smith's Plastic Surgery. Philadelphia: Lippincott Williams & Wilkins; 2013. p. 1682-93.
4. Oliveira Junior FC, Melega JM, Pinheiro AS, Destro C, Maciel PJ. Comparação entre a utilização da tela de Marlex em um dos dois planos para a reconstrução da parede abdominal pós-TRAM. Rev Bras Cir Plást. 2010;25(3 Suppl.1):49.
5. Vargo JD, Larsen MT, Pearson GD. Component Separation Technique for Repair of Massive Abdominal Wall Defects at a Pediatric Hospital. Ann Plast Surg. 2016;77(5):555-9. DOI: http://dx.doi.org/10.1097/SAP.0000000000000652
6. Ersoy YE, Celebi F, Erozgen F, Ergun SS, Akaydin M, Kaplan R. Repair of a postappendectomy massive ventral hernia using tissue expanders. J Korean Surg Soc. 2013;84(1):61-5. PMID: 23323238 DOI: http://dx.doi.org/10.4174/jkss.2013.84.1.61
7. Giele H, Vaidya A, Reddy S, Vrakas G, Friend P. Current state of abdominal wall transplantation. Curr Opin Organ Transplant. 2016;21(2):159-64. DOI: http://dx.doi.org/10.1097/MOT.0000000000000276
8. McCraw JB, Arnold PG. McCraw and Arnold's Atlas of Muscle and Musculocutaneous Flaps. Norfolk: Hampton Press Publishing Company Inc; 1986. p. 387-456.
9. Barbosa MVJ, Nahas FX, Pereira LM. Hernioplastia incisional associada a abdominoplastia. Rev Bras Cir Plást. 2010;25(3 Suppl.1):54.
10. Roxo CP, Carvalho TM, Borba MA, Silva lRB, Roxo ACW. Reconstrução de parede abdominal com tela aloplástica após infecção por micobactéria. Rev Bras Cir Plást. 2012;27(2):340-3. DOI: http://dx.doi.org/10.1590/S1983-51752012000200030
11. Nahas FX, Kimura AK, Barbosa MV, Juliano Y, Ferreira LM. Components separation technique with limited subcutaneous undermining: a cadaver study. Ann Plast Surg. 2011;67(3):303-8. DOI: http://dx.doi.org/10.1097/SAP.0b013e3181fb4a92
12. Barbosa MVJ, Nahas FX, Pereira LM. Aplicabilidades da técnica de separação de componentes para o tratamento das deformidades da parede abdominal. Rev Bras Cir Plást. 2010;25(3Suppl.1):44.
13. Desai KA, Razavi SA, Hart AM, Thompson PW, Losken A. The Effect of BMI on Outcomes Following Complex Abdominal Wall Reconstructions. Ann Plast Surg. 2016;76 Suppl 4:S295-7. PMID: 26808768 DOI: http://dx.doi.org/10.1097/SAP.0000000000000673
14. Harrison B, Khansa I, Janis JE. Evidence-Based Strategies to Reduce Postoperative Complications in Plastic Surgery. Plast Reconstr Surg. 2016;138(3 Suppl):51S-60S. DOI: http://dx.doi.org/10.1097/PRS.0000000000002774
1. Hospital das Clínicas, Universidade Federal de Pernambuco, Recife, PE, Brazil
2. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
Institution: Hospital das Clínicas, Universidade Federal de Pernambuco, Recife, PE, Brazil.
Corresponding author:
Kelson Kawamura
Av. Professor Moraes Rego, 1235, Cidade Universitária
Recife, PE, Brazil - Zip Code 50670-901
E-mail: kelson.1989k@hotmail.com
Article received: June 20, 2017.
Article accepted: January 26, 2018.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter