

Original Article - Year 2018 - Volume 33 -
Epidemiologic profiles, major complications, and mortality rate at a burn treatment center in the Amazon
Epidemiologia, principais complicações e mortalidade dos pacientes atendidos em um Centro de Tratamento de Queimados na Amazônia
ABSTRACT
INTRODUCTION: Despite complex multidisciplinary treatment, many burn patients die. This study aimed to determine epidemiologic profiles of burn patients, highlighting major complications.
METHODS: This retrospective study analyzed the medical records of burn patients managed at the Metropolitan Hospital for Urgent and Emergent Care, Pará State, between January 2007 and December 2012.
RESULTS: most patients were males (69.1%) aged 18 to 30 years (35.5%), referred from other hospitals (35.8%), and employed as construction workers (21.2%). The most frequent complications were respiratory (69.4%) and renal failure (57.1%), followed by sepsis (38.8%).
CONCLUSIONS: The data obtained were similar to those reported in national and international literature, highlighting the need for burn prevention and inspection of construction sites, as well as implementation of treatment protocols to improve care for burn patients.
Keywords: Burns/complications; Amazon; Epidemiology; Death.
RESUMO
INTRODUÇÃO: São muitos os pacientes queimados que, apesar de um complexo tratamento multidisciplinar, são levados ao óbito. O objetivo deste estudo é determinar o perfil epidemiológico, ressaltando as principais complicações que acometem os pacientes queimados.
MÉTODOS: Estudo retrospectivo que analisou prontuários de pacientes queimados atendidos no Hospital Metropolitano de Urgência e Emergência no Estado do Pará, no período de janeiro de 2007 até dezembro de 2012.
RESULTADOS: A maioria dos pacientes era do sexo masculino (69,1%), entre 18 e 30 anos (35,5%), procedente de outros hospitais (35,8%), trabalhador da construção civil (21,2%). As complicações mais encontradas foram insuficiência respiratória (69,4%), insuficiência renal (57,1%) e sepse (38,8%).
CONCLUSÕES: Os dados obtidos são similares aos encontrados na literatura nacional e internacional, evidenciando a necessidade de prevenção e fiscalização de trabalhadores da construção civil, bem como de implementar protocolos de tratamento para melhorar a assistência ao paciente queimado.
Palavras-chave: Queimaduras/complicações; Amazônia; Epidemiologia; Óbito.
Burn-related mortality has significantly decreased over the past 30 years1,2. However, many patients with severe burns develop complications that require complex multidisciplinary treatment, and many die3,4. Among the most common complications, sepsis and pneumonia often progress to multiple organ failure, which is s a major cause of mortality in these patients5-7.
An estimated 265,000 burn-related deaths occur annually, mostly in developing or underdeveloped countries8. Most are the result of accidents that could be prevented through the implementation of simple measures9. In Brazil, studies suggest that around 1,000,000 individuals sustain burn injuries each year10. In 2011, 1,437 patients were admitted to intensive care units, but Brazil only has 45 hospital facilities qualified to care for burn victims, and these are spread through the five Brazilian regions11,12.
There are few scientific studies on the epidemiology, risk factors, and treatment course of burn patients in the Northern region of Brazil. This region collects the least amount of data on burn injuries13. The present study analyzed the medical records of patients treated at the Metropolitan Hospital for Urgent and Emergent Care (HMUE) in Ananindeua (PA). This hospital has 20 beds and is the Northern region referral center for burn treatment.
The literature has shown that epidemiologic studies provide vital information for the development of public policies focused on burn prevention, as well as strategies that improve the treatment of burn injuries3,14,15.
OBJECTIVE
This study aimed to determine the epidemiologic profile, major complications, and mortality rate of patients treated at the HMUE Burn Treatment Center in Ananindeua (PA), between January 2007 and December 2012.
METHODS
This observational, descriptive, and cross-sectional study used data from the medical records of burn victims admitted to the HMUE between January 2007 and December 2012. We included patients older than 18 years and excluded those whose records did not provide adequate data for use in the assessment protocol previously prepared by researchers. We also excluded patients presenting for follow-up care.
The study protocol collected the following data: sex, age, where the injury occurred (geographic location), profession, association with work, referral source (primary care unit, emergency ward, hospital, residence, or other, e.g., community), percentage of burned body surface area, lesion depth (1st, 2nd, or 3rd degree), type of injury (thermal, electric, or chemical), and burn site and complications during hospitalization.
The diagnosis of sepsis was based on the criteria of the International Guidelines for Management of Severe Sepsis and Septic Shock: 2012. The criteria for the diagnosis of renal failure were based on the Acute Kidney Injury Network classification. Respiratory failure was diagnosed using carbon dioxide and oxygen levels obtained through arterial blood gas analysis in medical charts.
Descriptive and inferential statistical methods were used to characterize a sample of 647 burn patients according to death or survival outcomes. Quantitative variables were reported as mean and standard deviation. Qualitative variables were reported as absolute and relative frequency distributions.
Qualitative variables were compared using the independent chi-square test; when the restriction was npq<5, the G test for independent samples was applied (Ayres et al., 2007, p. 135). A significance (alpha) level = 0.05 was established. Statistical analysis was performed using GrafTable version 2.0 and BioEstat version 5.3.
The work was approved by the Ethics Committee for Research Involving Human Beings of the Health Sciences Institute of the Federal University of Pará (CEP/UEPA).
RESULTS
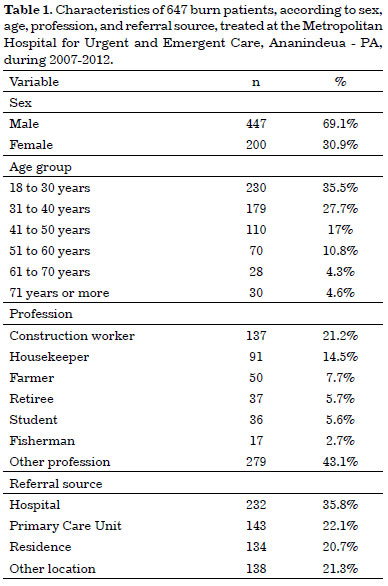
The study included 647 burn patients older than 18 years of age who were treated at the HMUE between January 2007 and December 2012. Of these, 69.1% (447) were males and 30.9% (200) were females. The largest age group was between 18 and 30 years old (35.5%), with those aged 61 to 70 years comprising 4.3% and those 70 years or older comprising 4.6%.
Among professions, construction workers (particularly electricians, welders, masons, master builders, and painters) accounted for the most burn injuries (21.2%). The second most affected category was domestic workers (14.1%), including housewives, who are exposed to similar risks of domestic accidents involving direct flame and hot liquids. Farmers accounted for 7.7% of burn injuries, followed by retirees (5.7%), and students (5.6%). All other professions and those who did not meet the protocol criteria were categorized as Others, accounting for 43.1%.
Among patients treated at the HMUE, 35.8% were transferred from other hospitals. Many patients were referred from primary care units (22%) or presented from their residences (20.7%). The general community, workplace, and other facilities accounted for 21.3% of patients (Table 1).
The most affected body regions were the upper limbs (UL), followed by the lower limbs (LL) and the face and torso, accounting for 49%, 46.5%, and 45,7%, respectively. The least affected body region was the perineum, accounting for 9.6% of burn patients. The hands (29.4%), neck (24.1%), abdomen (23.2%), back (18.7%), and foot (16.4%) were also affected (Figure 1).
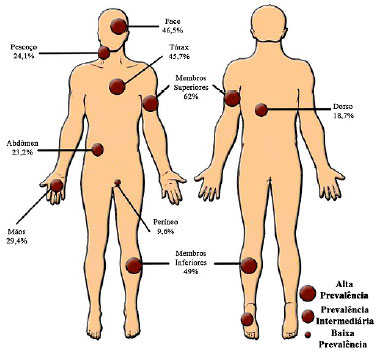
Figure 1. Burn distribution in 647 patients treated at the Metropolitan Hospital for Urgent and Emergent Care, Ananindeua - PA, during 2007-2012.
Only 8 patients (1.2%) presented with 1st degree burns. About 60% of all patients had 2nd degree burns and about 35% had 3rd degree burns. Only 44 patients (6.8%) had concurrent orthopedic trauma and burn injuries. The average body surface area involved was 26%, excluding 44 cases with unavailable data.
The length of hospital stay was not specified in 64.6% of the charts. About 12% of patients remained hospitalized for a period ranging from 1 to 7 days, with 8 to 14 days in 7.9% and 15 to 30 days in 8.3%. Only 13 patients remained hospitalized for more than 2 months. No patient was hospitalized for more than 4 months.
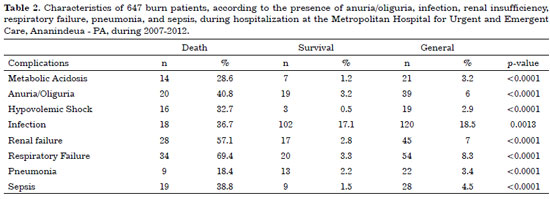
Complications were observed in 63.1% of burn patients, while 36.9% had no complications. The mortality rate was 83.7% in patients with complications and 16.3% in patients with no complications.
The primary complications in patients who died were respiratory failure (69.4%), renal failure (57.1%), and sepsis (38.8%) (Table 2). Of 120 patients with decreased urine output (anuria or oliguria), 18 died. Among all patients studied, 19 had hypovolemic shock and only 3 survived their burn injuries. During the hospital stay, 22 patients had pneumonia and 13 survived. Metabolic acidosis was a complication in only 3.2% (21) of the patients studied. Among other hydration and biochemical abnormalities, hypoalbuminemia and hypokalemia were present in 5.6% and 4.8% of the patients, respectively.
DISCUSSION
The patients in this study were predominantly males (69.1%) aged 18 to 30 years, consistent with other reports3,16,17. These findings suggest that males have increased risk factors, both at work and in daily life. In contrast, studies by Kumar et al.18 in India and Ahmadijouybari et al.9 in Iran showed a predominance of females, with most burn injuries being non-accidental (i.e., the result of attempted suicide or homicide).
Among all professional categories, construction workers were most commonly affected by burns, as a result of exposure to a hazardous work environment. This indicates that workplace safety measures and monitoring are deficient. Some construction workers may take risks, probably because of the lack of training, and many fail to use protective equipment or standard accident prevention protocols.
The burn injuries sustained by construction workers occurred both at the workplace, where they may be monitored, but also during side work outside the workplace, possibly because of self-exposure to the risk of accidents, as a consequence of self-confidence and work experience.
Domestic workers and housewives were also significantly affected by burns, due to exposure to stoves, hot liquids, and gas explosions, especially when the equipment is primitive, as reported by Kumar et al18.
Farmers were often affected by burns. This can be explained by the economic dynamics of Pará state, where family farming is still a primary source of income for a significant part of the population. Careless agricultural practices can expose the worker to the inherent risks of this activity. Pará is the second largest state in Brazil, and lacks an adequate road network, making it difficult to implement and supervise educational policies aimed at improving the health of rural workers.
Retirees were often affected by burns. Such accidents are likely to occur when elderly individuals attempt household tasks that are not compatible with declining physical ability.
Fishermen were also significantly affected. A large part of the population of Pará practices this activity, since the Amazon River plays a crucial role in economic dynamics.
Similar to a study by Ortiz-Prado et al.19 and Wasiak et al.20, the regions with the highest burn prevalence were LL and UL. The burn site may also be an important risk factor for adverse surgical outcomes. LL reconstruction procedures were more likely to develop complications21. Skin grafting was performed in 33.5% of the patients studied. Of these, approximately 60% had 3rd degree burns. Autologous dermo-epidermal grafting was used to restore the cutaneous barrier, to promote wound healing by reducing fluid, electrolyte, and protein loss, as well as reducing the risk of infection.
Concomitant trauma may increase burn-related mortality, as reported by Hefny et al.22. However, this association was not statistically significant (p>0.844) in our analysis. Of 6.8% with concurrent trauma and burns, only 3 died.
A large percentage had 3rd degree burns (35%), with different degrees of depth, consistent with prior reports23.
Similar to the 20% reported by Leão et al.17, the average body surface involvement was 26% in this study. However, this was in contrast to the study by Kumar et al.18, who reported an average body surface involvement greater than 50%. This is explained by the fact that most burns were non-accidental, i.e., the result of attempted suicide or homicide.
Burn patients are subject to social stigmatization, because of absence from work, disabilities, self- or family-inflicted physical injuries, huge medical expenses, etc. All these aspects must be considered in the treatment of these patients24.
Most patients had complications (63.1%), and mortality was greater in this group. Respiratory insufficiency, renal failure, and sepsis were the primary complications. The literature indicates that renal injury is particularly important4, since severe burns might promote intense inflammatory activity and apoptosis, decreased renal perfusion, and exposure to nephrotoxic metabolites.
A significant number of patients developed pneumonia. This reaffirms the findings of Brusselaers1, who reported that pneumonia was a respiratory complication most likely to be fatal. Of patients with pneumonia, 59% died, consistent with the findings reported by Kumar et al.18.
Hypovolemic shock, also consistent with the report by Kumar et al.18, was associated with a high mortality rate. In our study, hypovolemic shock occurred in approximately 3% of patients. Of these, about 80% died, in agreement with Kumar et al.18, who reported that hypovolemic shock is the fifth most common complication associated with death, being responsible, along with toxemia, for 5.7% of all mortality.
A decline in urine output (oliguria or anuria) was detected in 39 patients. About 40% of these individuals died. In 21 burn patients, anuria/oliguria was caused by dehydration. Anuria/oliguria progressed to kidney failure in 28 patients. Among the 3 primary complications associated with death in burn patients, acute renal failure is commonly observed, and is associated with multiple organ failure6.
All burn patients have a high risk of infections and sepsis, requiring management by the entire health team, since recent studies showed that sepsis was the leading cause of death in burn patients who survived the initial burn injury4. In this study, 76% of patients who died developed sepsis during treatment, reaffirming the report by Belba and Petrela3, demonstrating that most deaths were caused by sepsis.
CONCLUSION
This study showed that burn patients treated in the HMUE Burn Treatment Center were predominantly males aged 18 to 30 years, who worked in construction and were referred from other hospitals in the region. Most second degree burns occurred in the upper limbs, and complications associated with the risk of death were respiratory failure, kidney failure, and sepsis.
COLLABORATIONS
JACS Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
FSV Analysis and/or interpretation of data; final approval of the manuscript; writing the manuscript or critical review of its contents.
MMM Analysis and/or interpretation of data; statistical analyses; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
AVML Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
LMC Analysis and/or interpretation of data; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
CLPB Analysis and/or interpretation of data; statistical analyses; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
REFERENCES
1. Brusselaers N, Monstrey S, Vogelaers D, Hoste E, Blot S. Severe burn injury in Europe: a systematic review of the incidence, etiology, morbidity, and mortality. Crit Care. 2010;14(5):R188. DOI: http://dx.doi.org/10.1186/cc9300
2. Klein MB, Goverman J, Hayden DL, Fagan SP, McDonald-Smith GP, Alexander AK, et al.; Inflammation and Host Response to Injury, and Large-Scale Collaborative Research Program. Benchmarking outcomes in the critically injured burn patient. Ann Surg. 2014;259(5):833-41. DOI: http://dx.doi.org/10.1097/SLA.0000000000000438
3. Belba MK, Petrela EY. Epidemiology and mortality of burned patients treated in the University Hospital Center in Tirana, Albania: an analysis of 2337 cases during the period 1998-2008. Burns. 2012;38(2):155-63. DOI: http://dx.doi.org/10.1016/j.burns.2011.03.024
4. Rex S. Burn injuries. Curr Opin Crit Care. 2012;18(6):671-6. DOI: http://dx.doi.org/10.1097/MCC.0b013e328359fd6e
5. Kallinen O, Maisniemi K, Böhling T, Tukiainen E, Koljonen V. Multiple organ failure as a cause of death in patients with severe burns. J Burn Care Res. 2012;33(2):206-11. DOI: http://dx.doi.org/10.1097/BCR.0b013e3182331e73
6. Dokter J, Felix M, Krijnen P, Vloemans JF, Baar ME, Tuinebreijer WE, et al.; Dutch Burn Repository Group. Mortality and causes of death of Dutch burn patients during the period 2006-2011. Burns. 2015;41(2):235-40. DOI: http://dx.doi.org/10.1016/j.burns.2014.10.009
7. Chipp E, Milner CS, Blackburn AV. Sepsis in burns: a review of current practice and future therapies. Ann Plast Surg. 2010;65(2):228-36. DOI: http://dx.doi.org/10.1097/SAP.0b013e3181c9c35c
8. Organização Mundial de Saéde. Burns Fact Sheet nº 365. Genebra: Departamento de Saéde; 2014. [acesso 2017 Dez 27]. Disponível em: http://www.who.int/mediacentre/factsheets/fs365/en/
9. Ahmadijouybari T, Najafi F, Moradinazar M, Karami-matin B, Karami-matin R, Ataie M, et al. Two-year hospital records of burns from a referral center in Western Iran: March 2010-March 2012. J Inj Violence Res. 2014;6(1):31-6.
10. Fracanoli TS, Magalhães FL, Guimarães LM, Serra MCVF. Estudo transversal de 1273 pacientes internados no centro de tratamento de queimados do Hospital do Andaraí de 1997 a 2006. Rev Bras Queimaduras. 2007;7(1):33-7.
11. Brasil. Ministério da Saéde. Cartilha orienta o atendimento às vítimas de queimadura. [Internet]. Brasília: Ministério da Saéde; 2012. [acesso 2015 Maio 3]. Disponível em: http://www.blog.saude.gov.br/promocao-da-saude/30988-cartilha-orienta-atendimento-as-vitimas-de-queimadura.html
12. Brasil. Ministério da Saéde e Agência de Saéde de MG. Atenção à Saéde: Mais R$ 1,8 milhão para assistência a queimados. [Internet]. Jan 2012 [acesso 2015 Abr 2015]. Disponível em: http://www.blog.saude.gov.br/29536-mais-r-1-8-milhao-para-assistencia-a-queimados.html
13. Brasil. Ministério da Saéde. Indicadores básicos para a saéde no Brasil: conceitos e aplicações. [Internet]. Brasília: Ministério da Saéde; 2008 [acesso 2012 Out 5]. Disponível em: http://tabnet.datasus.gov.br/tabdata/livroidb/2ed/indicadores.pdf
14. Gowri S, Vijaya AN, Powar R, Honnungar R, Mallapur MD. Epidemiology and Outcome of Burn Injuries. J Indian Acad Forensic Med. 2012;34(4):312-4.
15. Wolf SE, Phelan HA, Arnoldo BD. The year in burns 2013. Burns. 2014;40(8):1421-32. PMID: 25454722 DOI: http://dx.doi.org/10.1016/j.burns.2014.10.026
16. Steinvall I, Fredrikson M, Bak Z, Sjoberg F. Mortality after thermal injury: no sex-related difference. J Trauma. 2011;70(4):959-64. DOI: http://dx.doi.org/10.1097/TA.0b013e3181e59dbe
17. Leão CEG, Andrade ES, Fabrini DS, Oliveira RA, Machado GLB, Gontijo LC. Epidemiologia das Queimaduras no estado de Minas Gerais. Rev Bras Cir Plást. 2011;26(4):573-7.
18. Kumar S, Ali W, Verma AK, Pandey A, Rathore S. Epidemiology and mortality of burns in the Lucknow Region, India--a 5 year study. Burns. 2013;39(8):1599-605. DOI: http://dx.doi.org/10.1016/j.burns.2013.04.008
19. Ortiz-Prado E, Armijos L, Iturralde AL. A population-based study of the epidemiology of acute adult burns in Ecuador from 2005 to 2014. Burns. 2015;41(3):582-9. DOI: http://dx.doi.org/10.1016/j.burns.2014.08.012
20. Wasiak J, Spinks A, Ashby K, Clapperton A, Cleland H, Gabbe B. The epidemiology of burn injuries in an Australian setting, 2000-2006. Burns. 2009;35(8):1124-32. DOI: http://dx.doi.org/10.1016/j.burns.2009.04.016
21. Kamolz LP, Parvizi D, Schintler M. Tissue expansion: things we should keep in mind. Burns. 2013;39(5):1024-5. DOI: http://dx.doi.org/10.1016/j.burns.2013.01.022
22. Hefny AF, Idris K, Eid HO, Abu-Zidan FM. Factors affecting mortality of critical care trauma patients. Afr Health Sci. 2013;13(3):731-5.
23. Montes SF, Barbosa MH, Sousa Neto AL. Aspectos clínicos e epidemiológicos de pacientes queimados internados em um Hospital de Ensino. Rev Esc Enferm USP. 2011;45(2):369-73. DOI: http://dx.doi.org/10.1590/S0080-62342011000200010
24. Enshaei A, Masoudi N. Survey of early complications of primary skin graft and secondary skin graft (delayed) surgery after resection of burn waste in hospitalized burn patients. Glob J Health Sci. 2014 Sep 18;6(7 Spec No):98-102. DOI: http://dx.doi.org/10.5539/gjhs.v6n7p98
1. Curso de Medicina, Universidade do Estado do Pará, Belém, PA, Brazil
2. Universidade Federal do Pará, Belém, PA, Brazil
3. Universidade Federal do Rio de Janeiro, Rio de Janeiro, RJ, Brazil
Institution: Hospital Metropolitano de Urgência e Emergência, Belém, PA, Brazil.
Corresponding author:
Marina Matos Martins
Rua Tiradentes, 650, apto 1101 - Reduto
Belém, PA, Brazil - Zip Code 66053-330
E-mail: maris.martins1@gmail.com
Article received: October 26, 2015.
Article accepted: October 19, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter