

Ideas and Innovation - Year 2018 - Volume 33 -
Closed glabellar myotomy: a new surgical approach to treat wrinkles without scarring
Miotomia glabelar fechada: uma nova abordagem cirúrgica para tratar rugas sem cicatrizes
ABSTRACT
INTRODUCTION: Hyperactivity of the glabellar musculature and resulting wrinkles are frequent complaints in the field of plastic surgery. Treatment consists of blocking the involved muscles. We propose a closed approach for the treatment of glabellar musculature.
METHODS: Seventy-eight patients underwent operation between April 2012 and August 2015. Myotomy includes the use of markings and polyglactin 0 wire or steel wire, passing through the marked lines several times, entering the eyebrow and using the juxtaperiostal plane, returning through the same orifice of the needle toward the entry hole, and using the subcutaneous plane.
RESULTS: Good results were obtained in all cases by preventing glabellar muscle activity during the period evaluated (at least 1 year), with improvement in wrinkles and muscle hyperactivity. The complications observed included temporary paresthesia in the frontal region (35 cases) and partial recurrence (4 cases). There was no case of total recurrence. The options for long-term surgical treatment of glabellar wrinkles are myotomy, partial neurotomy, or myectomy. Closed glabellar myotomy prevents some possible complications associated with these options, reduces the surgical time, requires the use of conventional surgical instruments, eliminates scarring, and causes asymmetric correction, less edema, and fewer bruises.
CONCLUSION: Closed glabellar myotomy seems to be a good alternative compared to other traditional surgical options, because it eliminates scarring, allows correction of asymmetry, and presents good long-term results.
Keywords: Rhytidoplasty; Reconstructive surgical procedures; Face; Esthetics.
RESUMO
INTRODUÇÃO: A hiperatividade da musculatura glabelar e as consequentes rugas são queixas frequentes na cirurgia plástica. O tratamento consiste em impedimento dos mésculos relacionados. Propomos uma abordagem fechada para o tratamento da musculatura glabelar.
MÉTODOS: 78 pacientes foram operados entre abril de 2012 e agosto de 2015. A miotomia é realizada guiada pela marcação e tem início utilizando fio de poliglactina 0 ou fio de aço, passando várias vezes através das linhas marcadas, entrando pelo supercílio e utilizando o plano justaperiostal, retornando através do mesmo orifício da agulha em direção ao orifício de entrada, agora usando o plano subcutâneo.
RESULTADOS: Foram obtidos bons resultados em todos os casos com impedimento da atividade da musculatura glabelar durante o período avaliado (pelo menos 1 ano), com melhora das rugas e hiperatividade. As complicações observadas foram parestesia temporária na região frontal central (35 casos) e recidiva parcial (4 casos). Não foi observado nenhum caso de recorrência completa. As opções de tratamento cirérgico de longo prazo para rugas glabelar são miotomia, neurotomia parcial ou miectomia. A miotomia glabelar fechada evita algumas possíveis complicações associadas a essas opções, diminui o tempo cirérgico utilizando instrumentos cirérgicos convencionais, permite a correção de assimetria, com menos edema, menos equimoses e evita cicatrizes.
CONCLUSÃO: A miotomia glabelar fechada parece ser uma boa alternativa às outras opções cirúrgicas tradicionais, porque evita cicatrizes, permite correção de assimetria e apresenta bons resultados a longo prazo.
Palavras-chave: Ritidoplastia; Procedimentos cirérgicos reconstrutivos; Face; Estética.
Wrinkles occur from the contraction and hyperactivity of glabellar muscles and are frequent complaints in private plastic surgery clinics1.
The muscles that are related to wrinkles and hyperactivity are the corrugators, with oblique and horizontal portions, the depressor supercilii, and the medial portion of the orbicularis oculi muscle of the eye. Treatment involves the blocking of contraction activity in these muscles. This can be done chemically using botulinum toxin2, with a temporary effect, or surgically via classic coronal access3, endoscopic access4, superciliary access5, transblepharoplasty access6 and minimal non-endoscopic accesses7.
OBJECTIVE
The objective of this study is to describe the use of an alternative approach to myotomy of the glabellar muscles, without incisions, performed with multiple suture passes.
METHODS
The patients were prepared with blue pen markings upon forced expression for vertical glabellar wrinkles (related with corrugator supercilii and the medial portion of the orbital fibers of the orbicularis oculi) and horizontal (related with the procerus muscle and depressor supercilii) (Figure 1).
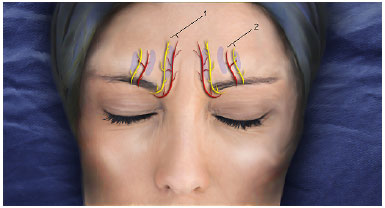
Figure 1. Projection of the supratrochlear (1) and supraorbital (2) nerves, in yellow, and corresponding arterial vessels in red. The supraorbital vascular-nervous bundle can be palpated from the supraorbital notch in the upper orbital rim. The vascular-nervous bundle is medial to the upper orbital rim.
The supraorbital and supratrochlear nerves were marked based on their anatomical references (supraorbital cleft) and suture passages were planned in parallel to prevent sectioning of the major vascular and nerve bundles (Figure 1). Sedation or general anesthesia was recommended for patient comfort. Infiltration of the glabellar region was performed with 20-25 mL of 0.25% lidocaine solution and 1: 250,000 epinephrine.
Myotomy was performed vertically, guided by the markings of the wrinkles in the skin, using polygalactin 0 or steel suture 0. We preferred to start inferiorly (near the orbital rim) (Figure 2a), passing deeply juxtaperiostal and exiting in the frontal region above the limits of the glabellar musculature (Figures 2b and 2c).
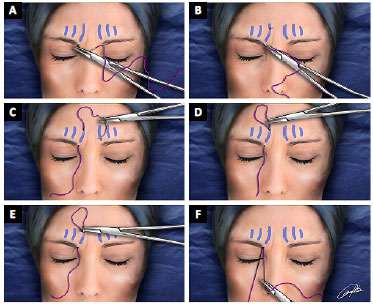
Figure 2. A: Begin with the needle on the bottom edge of the superciliary follicles; B: The passage of the rectified needle is deep, juxtaperiostal, exiting the frontal region, above the limits of the glabellar musculature; C: The needle returns through the same upper orifice; D: The needle progresses toward the entrance orifice, in the subcutaneous plane; E: The needle comes out in the same inlet orifice near the orbital rim; F: The glabellar musculature is "embraced" and is then sectioned by the wire.
Thereafter, using the same exit hole of the needle in the frontal region (Figure 2d), the needle was directed inferiorly in the subcutaneous plane to the entry hole, near the orbital rim (Figure 2e). With this vertical maneuver, the glabellar musculature was "embraced" by the suture, and the muscle was "serrated" with soft to-and-from movements of the suture (Figure 2f). We repeated this maneuver 5 times on each side, in different glabellar wrinkles, avoiding the projection of nerves (previously marked). The procerus and corrugator supercilii muscles were released with similar horizontal maneuvers (2 passes), close to the fronto-nasal suture.
Hemostasis was performed with compression for 5-10 minutes during the procedure. Dressings were made from rectangular foam coated cotton fabric and elastic bands, which were removed after 24 hours. The follow-ups occurred 1 day, 1 week, and 1,3, and 12 months postoperatively.
RESULTS
Seventy-eight patients, 73 (93.5%) women and 5 men (6.4%) underwent this surgical technique between March 2012 and August 2015 during rhytidoplasty due to complaints of wrinkles or hyperactivity of the glabellar musculature, classified as grade 3, 4, or 5, according to the Lemperle et al8 classification for glabellar wrinkles.
All cases were evaluated 1, 3, 6 and 12 months postoperatively. The longest follow-up period was 4 years (8 cases). Good results were achieved in all cases (Figures 3 and 4), with blocking of the vertical and horizontal wrinkles, besides improvement of hyperactivity during evaluation. The most commonly observed complication was temporary paresthesia of the frontal central region and/or scalp, with spontaneous resolution at 3 and 12 months. Complete ablation was observed in 74 (94.8%) cases and partial recurrence in 4 (5.2%) cases. Partial recurrence was observed when fewer passes were made, especially in the first cases evaluated. This was attributed to the learning curve.

Figure 3. A: Woman, 53 years old, preoperative aspect, glabellar region under contraction; B: 4 months postoperatively under contraction; C: Woman, 41 years old, preoperative aspect glabellar region under contraction; D: 6 months postoperatively under contraction; E: Woman 51 years old, preoperative glabellar region under contraction; F: 6 months postoperatively under contraction

Figure 4. A: Female patient, 57 years old, preoperative aspect, glabellar region under contraction; B: Postoperative period of 13 months under contraction; C: Female patient, 39 years old, preoperative aspect, glabellar region under contraction; D: Post-operative period of 7 years under contraction.
Hematomas were observed in 12 (15.3%) cases during the procedure and were drained manually with compression and dressings routinely, without recurrence. Thereafter, the infiltrated volume was increased, facilitating the passage of the wire and reducing hematomas.
No case of seroma or infection was observed. Asymmetry was also not observed.
DISCUSSION
Many patients use botulinum toxin for relief of hyperactivity and glabellar wrinkles with good results. After several applications, some patients request more lasting procedures. Several accesses and surgical techniques have been developed in this quest.
Originally, surgical access to treat the glabellar musculature was through a classic coronal incision3,4. More recently, endoscopic techniques4, superciliary access5, transblepharoplasty6 access, and other non-endoscopic accesses with minimal incisions have emerged as less-invasive alternatives7.
The main advantage of the closed glabellar myotomy technique is the lack of an apparent scar, in addition to being simple, fast, with a fast learning curve and less chance of complications. The disadvantage is that it is made without direct vision, with theoretical possibility of lesions of the nerves in the region and recurrence. Neither hypotheses were observed in the cases studied. We attribute this to the myotomy in multiple levels, which hinders muscle regeneration, the little anatomical variation of the supratrochlear and supraorbital nerves in this topography, and personal experience in myotomy5,9,10.
Minimum contraction was observed in cases with type 4 and 5 classifications of Lemperle et al8. This was attributed to residual fibers related to cases of severe glabellar muscle hyperactivity and good regenerative capacity of the interlaced musculature in the glabellar area. Even in cases of partial recurrence, there was a large reduction of contraction and high patient satisfaction.
Local edema was observed in all cases, reaching the eyelid region in the first post-surgical days, with improvement in 1 week with dressings and cold compresses.
Muscular treatment of the glabellar region can be performed with myotomy or myectomy. We prefer myotomy given the results obtained during the last 12 years with similar muscular approaches5,9,10 and to prevent depressions and irregularities without the use of fillers.
Myotomy can be performed with threaded stranded steel wire or polyglactin. Initially, straight stranded steel wire was used, but the difficulty in obtaining this suture made us look for a more available alternative, and we started to use polyglactin 0, which despite being a little more resistant in the treated tissues, can perform with similar efficiency in closed glabellar myotomy.
The result is similar to that obtained with other surgical techniques and botulinum toxin but produces long-term results.
The dressing is very important to prevent hematoma and seroma and should not be removed within the first 24 hours of the procedure.
In our opinion, this new access is easier and faster than other surgical techniques available, with minimal and transient-possible complications. The cases were followed-up for 12 months post-surgically.
No references of closed glabellar myotomy were found in the reviewed literature (MEDLINE, LILACS).
CONCLUSION
Closed glabellar myotomy seems to be a good alternative to other surgical approaches in the treatment of glabellar hyperactivity and glabellar wrinkles, to eliminate the need for incisions and the small likelihood of complications.
COLLABORATIONS
RSG Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
DOB Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
GP Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
REFERENCES
1. Isse NG, Elahi MM. The corrugator supercilii muscle revisited. Aesthetic Surg J. 2001;21(3):209-15. DOI: http://dx.doi.org/10.1067/maj.2001.116055
2. Carruthers JD, Carruthers JA. Treatment of glabellar frown lines with C. botulinum-A exotoxin. J Dermatol Surg Oncol. 1992;18(1):17-21.
3. Ortiz-Monasterio F, Barrera G, Olmedo A. The coronal incision in rhytidectomy--the brow lift. Clin Plast Surg. 1978;5(1):167-79.
4. Ramirez OM. Why I prefer the endoscopic forehead lift. Plast Reconstr Surg. 1997;100(4):1033-9; discussion 1043-6. DOI: http://dx.doi.org/10.1097/00006534-199709001-00030
5. Gomes RS. Tratamento musculatura glabelar: abordagem superciliar. In: Graziosi A, Viterbo F. Cirurgia Estética da Região Frontal. 1ª ed. Rio de Janeiro: MedBook; 2011. p. 229-36.
6. Guyuron B, Michelow BJ, Thomas T. Corrugator supercilii muscle resection through blepharoplasty incision. Plast Reconstr Surg. 1995;95(4):691-6. DOI: http://dx.doi.org/10.1097/00006534-199504000-00010
7. Pitanguy I, Gontijo de Amorim NF. Forehead lifting: the juxtapilose subperiosteal approach. Aesthetic Plast Surg. 2003;27(1):58-62. DOI: http://dx.doi.org/10.1007/s00266-002-0058-6
8. Lemperle G, Holmes RE, Cohen SR, Lemperle SM. A classification of facial wrinkles. Plast Reconstr Surg. 2001;108(6):1735-50; discussion 1751-2. DOI: http://dx.doi.org/10.1097/00006534-200111000-00048
9. Gomes RS. Frontal and glabellar myotomy: single short frontal scar approach. Rev Bras Cir Plástica. 2011;26(3):446-52. DOI: http://dx.doi.org/10.1590/S1983-51752011000300014
10. Gomes RS, Rocha JD. Closed platysmotomy with a new device. Plast Reconstr Surg. 2012;130(6):915e-916e. PMID: 23190860 DOI: http://dx.doi.org/10.1097/PRS.0b013e31826da1b0
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Hospital Universitário de Florianópolis, Florianópolis, SC, Brazil
3. Universidade Federal de Santa Catarina, Florianópolis, SC, Brazil
Institution: Universidade Federal de Santa Catarina, Florianópolis, SC, Brazil.
Corresponding author:
Rogerio Schutzler Gomes
Rua Vitor Konder, 125 s. 301 - Centro
Florianópolis, SC, Brazil - Zip Code 88015-400
E-mail: plasticarogerio@gmail.com
Article received: February 7, 2017.
Article accepted: September 23, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter