

Case Report - Year 2018 - Volume 33 - Issue 1
Closure of hemicorporectomy using a subtotal unilateral tight flap: a case report
Fechamento de hemicorporectomia com utilização do retalho subtotal unilateral da coxa: relato de caso
ABSTRACT
Hemicorporectomy or translumbar amputation was first described in 1950 by Kredel to treat locally advanced pelvic neoplasia. This extensive surgical procedure can achieve oncological cure and improve clinical status and quality of life. The authors present a case report of a 34-year-old patient with squamous cell carcinoma in a chronic pressure ulcer affecting the right perineum, gluteus, and posterior thigh. The patient underwent hemicorporectomy with reconstructive surgery using a partial-thickness flap of the left thigh. The postoperative course was good, and the use of a partial-thickness flap of the thigh to close the hemicorporectomy proved to be safe, efficient, and reproducible.
Keywords: Squamous cell carcinoma; Pressure ulcer; Surgical flaps; Reconstructive surgical procedures; Amputation; Osteomyelitis.
RESUMO
A hemicorporectomia ou amputação translombar foi primeiramente descrita em 1950 por Kredel como método curativo para neoplasia localmente avançada de pelve. Trata-se de um procedimento cirérgico extenso, que quando bem indicado é capaz de prover a cura oncológica, além de possibilitar a melhora clínica e de qualidade de vida. Os autores apresentam o relato de caso de um paciente de 34 anos, com carcinoma espinocelular em élcera de pressão crônica, acometendo períneo, gléteo e coxa posterior à direita. O paciente foi submetido à hemocorporectomia com reconstrução utilizando retalho subtotal da coxa esquerda. Observou-se boa evolução no pós-operatório e a utilização do retalho subtotal da coxa para fechamento da hemicorporectomia se mostrou como método seguro, eficiente e de técnica reprodutível.
Palavras-chave: Carcinoma de células escamosas; Úlcera por pressão; Retalhos cirérgicos; Procedimentos cirérgicos reconstrutivos; Amputação; Osteomielite.
Hemicorporectomy or translumbar amputation was first described in 1950 by Kredel, and this technique was considered the only curative method for locally advanced pelvic neoplasia. Ten years later, the first case of successful hemicorporectomy was described by Kennedy et al. for recurrent rectal adenocarcinoma. This patient survived only 11 days, and the cause of death was acute pulmonary edema. In 1961, Aust and Absolon presented the first case of hemicorporectomy with prolonged survival (approximately 19 years)1.
During the last 5 decades, there have been improvements in the surgical technique involving hemicorporectomy, including the use of thigh flaps, providing a cushion to support the remaining lumbar spine and abdominal viscera, and removing the suture line from the supporting region, as occurred in the primary closure of fish-mouth incisions. This strategy may help avoid total dehiscence due to exposure of the spinal canal and meningitis, thus reducing morbidity and mortality.
Important advances included the two-stage approach, separating the time of urinary and digestive derivation from the hemicorporectomy, and the back-to-front approach. The back approach, with lumbar spine section, significantly reduced blood loss because Batson’s venous plexus was not engorged, as was common after ligation of the iliac veins or vena cava1,2.
The use of a full-thickness flap of the thigh was first described by Georgiade in 1956 for extensive trochanteric ulcers with associated femoral osteomyelitis. Since then, variations of this flap have been used in cases of pressure ulcers, hemipelvectomy, and hemicorporectomy. The partial-thickness flap of the thigh does not include the posterior compartment, thus reducing its volume and weight. This flap procedure can be performed unilaterally or bilaterally depending on the defect and flap size required for closure3.
The first case of hemicorporectomy was described in Brazil in 2006 in Manaus and the procedure was performed because of the progression of a pressure ulcer to squamous cell carcinoma (Marjolin). In this case, an approach involving a one-stage front-to-back primary closure of the trunk was chosen4.
CASE REPORT
The hemicorporectomy in the reported case was performed at the Cancer Institute of the State of São Paulo in 2016. A one-stage procedure with a combined approach for closure of the vascular structures and spine was chosen and a partial-thickness flap of the left thigh was used to close the trunk in a 34-year-old male patient diagnosed with squamous cell carcinoma in a chronic pressure ulcer (Marjolin).
The patient had paraplegia due to a firearm injury 26 years prior. Since 1997, he had pressure ulcers (trochanteric, ischial, and sacral) that were difficult to treat using multiple approaches. In 2013, he underwent debridement of a right sciatic ulcer and closure with a gluteal VY thigh flap.
The pathological diagnosis was well-differentiated squamous cell carcinoma with involvement at the margins. In 2013 and 2014, the patient was subjected to 3 more surgical procedures due to margin expansion, but none was sufficient for total resection of the cancer, with persistence of deep margins and encroachment on the anal margins. The patient developed a fistula and infection, requiring prolonged hospitalization for broad-spectrum antibiotic therapy, creation of a loop colostomy at the right colonic flexure, and debridement of infection in the right hip.
The patient had clinical stage T4N + M0 when hemicorporectomy was chosen. The lesion was ulcerovegetative and extensive, involving the perineum, gluteal region, and right posterior thigh, with foul odor and need for antibiotic venous therapy at a day hospital (Figure 1).

Figure 1. Preoperative.
Hemicorporectomy with curative intent and improvement of the quality of life was chosen in a multidisciplinary meeting. The patient was prepared psychologically and showed interest in undergoing the procedure, despite its magnitude. The surgical procedure involved preliminary planning by the medical teams, opting for a one-stage procedure because the patient already had an intestinal bypass.
The procedure was started with the patient in horizontal dorsal decubitus (HDD) position by the oncologic surgery team. A transverse incision was made at the level of the iliac crests, and an inventory of the abdominal cavity demonstrated paracaval, bilateral iliac, and left inguinal lymphatic involvement without clinical signs of metastatic disease. The right common iliac artery and left internal iliac artery were ligated, and blood flow was maintained through the bilateral iliac veins and left external iliac artery.
The plastic surgery team was responsible for dissecting the partial-thickness flap of the left thigh. A medial and lateral incision was made throughout the length of the thigh and the two incisions were joined anteriorly at the knee level. A medial incision was made between the adductor magnus and semimembranosus muscle and a lateral incision was made in the lateral intermuscular septum of the femur. Dissection was made from the distal to the proximal region in the subperiosteal plane, and ligation of the superficial femoral vessels was made distally. The adductor muscle was sectioned proximally, and the deep femoral artery was closed after excision of the vascular branches of the thigh (Figure 2).
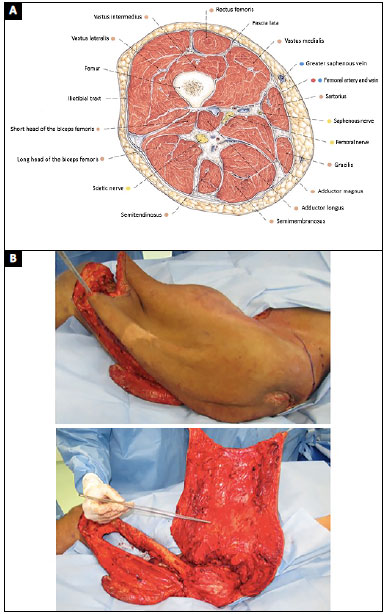
Figure 2. A: Source: Sobota Atlas Vol. 2, ed. 21; B: Partial-thickness flap of the thigh.
The patient was moved to the left decubitus position and the spine surgeons sectioned the spine at L4/L5 and sutured the dural sac. The position was again changed to HDD, followed by ligation of the right and left internal common iliac veins, sectioning of the remaining paravertebral muscles, and disarticulation (Figure 3). A new distal colostomy was performed for reimplantation of the ureters and closure of the peritoneum. The flap was positioned for tissue closure, excess flap tissue was discarded, closure was performed with two Blake drains, and the incisions were sutured in planes (Figure 4).
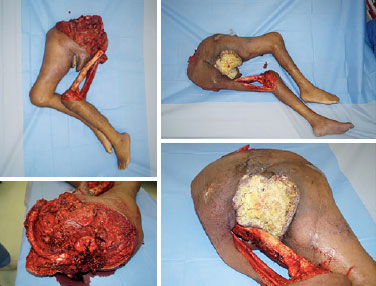
Figure 3. Disarticulation.
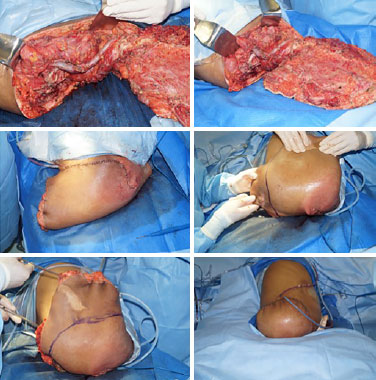
Figure 4. Closure.
The procedure lasted 16 hours and required 9,500 mL of crystalloid, 100 mL of albumin, three units of packed red blood cells, and 2,860 mL of diuresis. At the end of surgery, the patient required noradrenaline 0.3 µg/kg/min and was transferred to the intensive care unit. The patient was extubated on the first postoperative day, an oral diet was initiated, administration of vasoactive drugs was suspended on the third postoperative day, and the patient was transferred to the ward on the fourth postoperative day.
Prior to preparation of this case report, the patient had been hospitalized for 25 days in the ward, fed orally, and reported being satisfied with the surgical results. One complication was a collection of 80 mL of fluid under the surgical flap, which was drained by computed tomography-guided needle aspiration, and the remaining drains were removed. There was partial loss of continuity between the epidermis and dermis along a 6-cm suture line, but surgical intervention was not required (Figure 5).

Figure 5. Postoperative.
DISCUSSION
Hemicorporectomy or translumbar amputation is an extensive and radical procedure and its main indications are locally advanced pelvic neoplasms and complex pressure ulcers3.
Improvements in intensive care associated with the pathophysiological understanding of volume overload and increased peripheral vascular resistance after vessel ligation were the major contributors to the decrease in early in-hospital mortality. The evolution of the operative technique with migration to the back-to-front approach reduced intraoperative bleeding and hospitalization time2.
The use of the partial-thickness flap of the thigh provided a support cushion for the abdominal viscera and remaining lumbar spine, removing the suture line from the support region and consequently reducing the severity of the complications related to surgical closure. The surgical technique described herein proved to be safe, efficient, and reproducible.
The participation of plastic surgeons in the multidisciplinary team is essential because of the many advantages of a partial-thickness flap of the thigh compared to primary closure. Although the literature reports postoperative complications in 100% of cases of hemicorporectomy closure, the extent of closure varies according to the technique used, and primary closure of fish-mouth incisions is associated with the highest complication rate3.
In general, the quality of life of these patients is improved in the postoperative period despite the sequelae associated with the procedure. Psychological and emotional support for the patient and family, in addition to rehabilitation are essential3.
COLLABORATIONS
TTM Conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
FFB Final approval of the manuscript; completion of surgeries and/or experiments.
VATG Final approval of the manuscript; completion of surgeries and/or experiments.
CALA Final approval of the manuscript; completion of surgeries and/or experiments.
VAP Completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
ARGN Completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
RG Final approval of the manuscript.
REFERENCES
1. Chang DW, Lee JE, Gokaslan ZL, Robb GL. Closure of hemicorporectomy with bilateral subtotal thigh flaps. Plast Reconstr Surg. 2000;105(5):1742-6. PMID: 10809106 DOI: http://dx.doi.org/10.1097/00006534-200004050-00021
2. Barnett CC Jr, Ahmad J, Janis JE, Lemmon JA, Morrill KC, McClelland RN. Hemicorporectomy: back to front. Am J Surg. 2008;196(6):1000-2. PMID: 19095122 DOI: http://dx.doi.org/10.1016/j.amjsurg.2008.08.009
3. Janis JE, Ahmad J, Lemmon JA, Barnett CC Jr, Morrill KC, McClelland RN. A 25-year experience with hemicorporectomy for terminal pelvic osteomyelitis. Plast Reconstr Surg. 2009;124(4):1165-76. PMID: 19935300 DOI: http://dx.doi.org/10.1097/PRS.0b013e3181b61169
4. Ricci MA, Duarte EL, Souza RC, Albuquerque-Peres CM, Guimaraes GC, Lopes A. Hemicorporectomy with double barreled wet colostomy: an extremely rare procedure. Rev Col Bras Cir. 2009;36(6):525-8. PMID: 20140398
1. Hospital das Clínicas, Faculdade de Medicina, Universidade de São Paulo, São Paulo, SP, Brazil
2. Universidade de São Paulo, São Paulo, SP, Brazil
3. Instituto do Câncer do Estado de São Paulo, São Paulo, SP, Brazil
Institution: Instituto do Câncer do Estado de São Paulo, São Paulo, SP, Brazil.
Corresponding author:
Thomaz Tourinho de Menezes
Rua Edith de Gama e Abreu, 352, apt 603
Itaigara - Salvador, BA, Brazil - Zip Code 41815-010
E-mail: thomazmenezes@hotmail.com
Article received: March 16, 2017.
Article accepted: January 26, 2018.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter