

Articles - Year 2000 - Volume 15 -
Nevus Comedonicus: Surgical Treatment
Nevo Comedônico: Tratamento Cirúrgico
ABSTRACT
Nevus comedonicus is a rare cutaneous abnormality clinically characterized by slightly prominent grouped papules with dark and firm keratotic pad. It consists in a linear or zosteroid lesion that has been treated by means of conservative or surgical methods. The present paper refers to a young female patient with extensive nevus comedonicus at left inframammary region submitted to lesion surgical exeresis using sliding flap technique.
Keywords: Nevus comedonicus; surgical treatment; sliding-flap
RESUMO
O nevo comedônico é uma anomalia cutânea rara, caracterizada clinicamente por pápulas agrupadas, levemente elevadas, com tampão ceratótico escuro e firme. Trata-se de lesão de conformação linear ou zosteriforme, que tem sido tratada por meio de métodos conservadores ou cirúrgicos.
A presente publicação refere-se a uma paciente jovem com extenso nevo comedônico em região inframamária esquerda, submetida a exérese cirúrgica da lesão, com a utilização de técnica de retalho por deslizamento.
Palavras-chave: Nevo comedônico; tratamento cirúrgico; retalho por deslizamento
Nevus comedonicus is a rare cutaneous abnormality described for the first time by Kofmann(1)in Germany, in 1895. Selhorst(2) described the first case in British literature in 1896 and Cohite(3) in American literature in 1914. Few reports were made since then(4,5,6). It consistsin an abnormal pilosebaceous apparatus resulting in a structure unable to produce hair, but capable of forming keratin(4,7). This entity has already received more than 16 denominations in literature, but "nevus comedonicus" is the most accepted one(4).
It is clinically characterized by slightly prominent grouped papules with a dark and firm keratotic pad, similar to comedos(8). Lesions usually present a linear or zosteroid distribution; however, cases have been described with extensive bilateral involvement(9,10). The most frequently affected site is the face, followed by the cervical region, trunk and upper limbs(1), but palmar, plantar and scalp lesions have already been described(9,12). Nevus comedonicus is present at birth in most cases but may become visible in any life period (10). There is no evidence of gender preference and white race seems to be the most frequently affected one(4). This entity may be associated to other skin lesions or central nervous system, musculoskeletal system and eye abnormalities(13).
Nevus comedonicus therapeutic approaches have included the use of topical keratolytic agents, comedo's manual extraction, dermabrasion and surgical excision of lesions(1,4,8).
The present paper refers to a young female patient with extensive nevus comedonicus at left inframammary region.
CASE REPORT
White fifteen years old female patient was referred to assessment and treatment of skin lesion compatible with nevus comedonicus. Lesion located at left inframammary site appeared when she was 6 years old as small grouped papules similar to comedos that started at sternum region and extended up to anterior axillary line, forming a zosteroid-distributed extensive lesion. Patient reported intermittent infection episodes with cyst and pustule formation that were treated with systemic and topical antibiotic therapy in addition to drainage. Atrophic scars were formed after these episodes. Patient denied other systemic pathologies and did not present other cutaneous changes. Surgical ablation of lesion was chosen due to infection relapse in spite of conservative treatments performed.
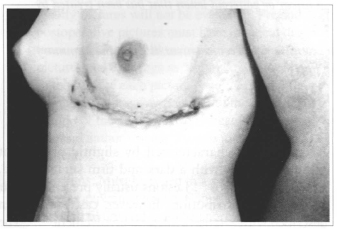
Fig. 1 - Postoperative aspect: left inframammary region lesion extending from anterior axillary line to presternum region.

Fig. 2 - Plate lesion with dilated follicles filled up by corneal plugs. Presence of atrophic-cicatricial areas and abscess areas.
Horizontal ellipse-shaped surgical planning for complete resection of lesion, comprehending skin and subcutaneous cellular tissue was performed. As lesion affected also mamma lower pole base all care was taken aiming at its shape preservation. An ample sliding flap at the left of epigastric region was made such as to allow occlusion of resection bloody area. Epigastric flap edge was anchored to muscle aponeurosis before being sutured to mamma to reduce tension and consequent distortion of mammary cone. A two-plane suture was performed at subcutaneous and skin levels. Antibiotic therapy with cephalexin started 24 hours before surgery and continued during the postoperative period. Drains were drawn on the third postoperative day presenting small collection in its orifices.
Healing process was normal, presenting, however, moderate scar enlargement at major mobility points and drain sites.
Anatomicpathologic study confirmed nevus comedonicus clinical diagnosis, showing presence of diffusely distributed brownish porosities at lesion surface. Small cystic cavities filled out with brownish and pasty material were observed upon section.
DISCUSSION
Nevus comedonicus is a rare pathology. A retrospective study carried out at St. George and St. Johns Hospitals, in London, for 20 years revealed an incidence of 1:45,000 cases(14). Another study published by Marcus and col.(4) revealed an incidence of 12 cases in a review of 100,000 skin biopsies.
Lesions, in general, are present at birth or develop during puberty. Lesion appearance during puberal phase is likely to be due to greater activity of pilosebaceous structures induced by hormones occurring during this phase(10). Cases of later appearance in patients up to 67 years old have been described(4).
Nevus comedonicus typically appears as a dilated hair follicle aggregation, filled up with pigmented keratinous material. Linear- or zosteroid-distributed unilateral or bilateral lesions may be encountered(9,10). There may be involvement of any part of the body, including face, scalp, cervical region, trunk, limbs and palmar and plantar regions. As to the present case, lesion had zosteroid unilateral configuration localized at left inframammary region. The nevus comedonicus may be clinically divided into two groups: one, in which comedos formation occurs with no suppurative predominance and the other, in which cystic formations, recurrent infections, fistulas, abscesses and scars are the predominant findings. Case reported fits into this latter group.
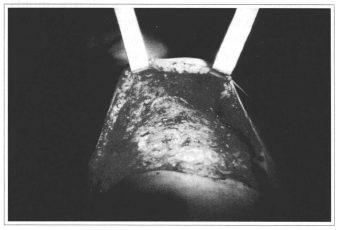
Fig. 3 - Sliding flap with ample dissection of upper abdomen.
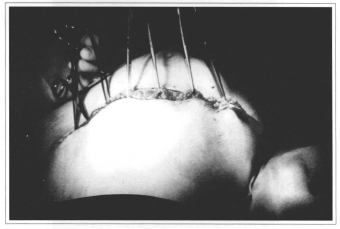
Fig. 4 - Upper abdomen flap traction for repairing postresection bloody area.

Fig. 5 - Subdermic, subcutaneous and intradermic suture at submammary fold preserving mammary cone.
Patient's anamnesis and physical examination did not show any associated pathology though there are several reports of other abnormalities accompanying nevus comedonicus in literature(8,9,13). Associated pathologies described include cataract, ichthiosis, basal cell linear nevus, trichilemmal cyst, intrapapillary elastoma, vascular abnormalities, absence of fifth finger, in addition to other central nervous system and musculoskeletal system changes(8,9,11,13,15).
Nevus comedonicus comes up spontaneously in general, but cases of this lesion appearance after herpes zoster, plain lichen, vaccination, furuncle or local traumatism episodes have been described. Patient of the case in question denied presence of previous lesions or traumatisms.
The main histological characteristics of nevus comedonicus include ample and deep epidermis invaginations, filled out by corneal material(16), such as in the case in question. Capillary bulbs, thin hair or small sebaceous gland lobules may be encountered at lower-portion invaginations(8,9,12).
Nevus comedonicus must be treated not only for cosmetic reasons, but also to prevent complications (suppurative infections and residual scars) (5). Different therapeutic approaches include topical retinoids, keratolitic agents, oral retinoids, antibiotic therapy, manual extraction of comedos, dermabrasion and surgical resection of lesion(4,8,11). Complete excision of lesion seems to be the most appropriate treatment(1,4,5). However, its extension and location many times limit procedure, which makes nevus comedonicus becoming a therapeutic problem(5,6). Patient in the present case was submitted to several conservative treatments with no significant improvement. Surgical approach with complete excision was the treatment of choice. In addition to the concern of completely resecting lesion, care was taken with other esthetic aspects. Upon resection, mammary cone shape was preserved. Epigastric flap anchorage was performed at major pectoral muscle aponeurosis upon resection area closure to avoid traction on mammary cone.
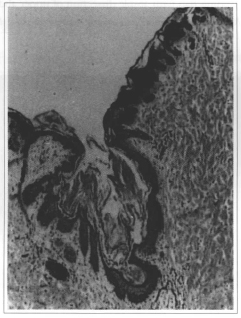
Fig. 6 -Lesion anatomicpathologic examination.
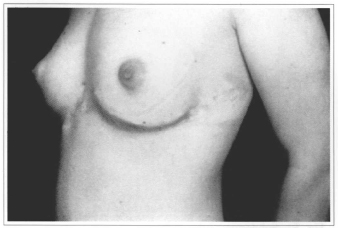
Fig. 7 - Postoperative aspect (2 months).
REFERENCES
1. KOFMANN S. Ein Fall von seltener Lokalisation und Verbreitung von Komedon. Arch. Dermatol. Syphilis. 1895;32:177-8.
2. SELHORST SB. Naevus acneiformis unilateralis. Br. J. Dermatol. 1896;8:419-21.
3. WHITE CJ. Nevus follicularis Keratosus. J. Cutan. Dis. 1914;32:187-90.
4. MARCUS J, ESTERLY NB, BAUER BS. Tissue expansion in a patient with extensive nevus comedonicus. Ann. Plast. Surg. 1992;29:362-6.
5. GONZALEZ-MARTINEZ R, MARIN-BERTOLIN S, MARTINEZ-ESCRIBANO J, AMORRORTU-VELAYOS J. Nevus comedonicus: report of a case with genital involvement. Cutis. 1996;58(6):418-9.
6. AGUADO IH, BERNAL AMP, RESINA MO, MARTÍNEZ FC. Nevus comedoniano. Med. Cut. ILA. 1984;12:439-41.
7. ALOI FG, MONERO A. Nevus comedonicus with epidermolytic hiperkeratosis. Dermatoligica. 1987;174:140-3.
8. KIM SC, KANG WH. Nevus comedonicus associated with epidermal nevus. J. Am. Acad. Dermatol. 1993;28:2734.
9. BECK MH, DAVE VK. Extensive nevus comedonicus. Arch. Dermatol. 1980;16:1046-50.
10. GRIMALT R, CAPUTO R. Posttraumatic nevus comedonicus. J. Am. Acad. Dermatol. 1993;28:273-4.
11. AL-ABOOSI M, ABALKHAIL A. Nevus comedonicus in Jordanian girl (letter). Int. J. Dermatol. 1994;33:521-2.
12. RESNIK KS, KANTOR GR, HOWE NR, DITRE CM. Dilated pore nevus. A histologic variant of nevus comedonicus. Am. J. Dermatopathol. 1993;15(2):169-71.
13. ENGBER PB. Nevus comedonicus syndrome (letter). Arch. Dermatol. 1982;118(1):1.
14. LEPPARD B, MARKS R. Comedone naevus: a report of nine cases. Trans. St. Johns. Hosp. Dermatol. Soc. 1973;59(1):45-51.
15. HAPPLE R. Epidermal nevus syndromes. Semin. Dermatol. 1995;14(2):111-21.
16. NILLES M, de VIRAGH PA, MOSSMANN H, HEINRICHS C, ECKERT F. Naevus follicularis Keratosus: clinical aspects, histology and histogenesis. Hautarzt. 1992;43:205-9.
I - Titular Professor of Plastic Surgery Discipline of Universidade de Caxias School of Medicine. Honorary Member of the Brazilian Society of Plastic Surgery.
II - Dermatology Resident at ISCMPA.
III - Academics of Medicine - 6th grade at FFFCMPA/ISCMPA.
Address for correspondence:
Luiz Carlos Celi Garcia, MD
R. Ernesto Alves, 581
95020-360 - Caxias do Sul - RS Brazil


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter