

Articles - Year 2000 - Volume 15 -
Masseter Muscle Hypertrophy
Hipertrofia do Músculo Masseter
ABSTRACT
Twenty patients presenting masseter hypertrophy and that had undergone surgical treatment were studied. The ages varied from 15 to 30 years, being 13 females and 7 males. The patients' main complaint was the aesthetics related to the increase of volume at he region of the mandibular angle. None of the patients reported a similar case in the family. The patients underwent a surgery with an extraoral approach at the first cases and an intraoral approach at the last 3 years. The performed surgery varied according to the deformity characteristics. We used the following categorization: 1: masseteric (6% of the patients), 2: masseteric-osseous(65%), 3: osseous(29%). Therefore, the surgeries were divided in: Group 1 = muscular ressection; group 2 = muscular ressection e osteotomy (ostectomy) e group 3 = ostectomy (osteotomy). A trismus period is expected, mainly in the patients with the resected muscle. All the patients reported an improvement at the facial aesthetics with the surgical technique used.
Keywords: Masseter hypertrophy; masseter
RESUMO
Foram estudados 20 pacientes com hipertrofia de masseter submetidos a tratamento cirúrgico. A idade variou de 15 a 30 anos, sendo 13 mulheres e 7 homens. A queixa principal dos pacientes era estética relacionada ao aumento de volume na região do ângulo mandibular.
Nenhum dos pacientes referiu caso semelhante na família.
Pacientes foram submetidos a cirurgia com abordagem extra-oral nos primeiros casos e intra-oral nos últimos 3 anos. O tipo de cirurgia realizada variou conforme a característica da deformidade. Usamos a classificação seguinte: 1 - massetérica (6% dos pacientes); 2 - massetérica-óssea (65%); 3 - óssea (29%).
Assim sendo as cirurgias se dividiram em: Grupo 1 = ressecção muscular; grupo 2 = ressecção muscular e osteotomia (ostectomia) e grupo 3 = ostectomia (osteotomia).
É esperado um período de trismo nos pacientes principalmente naqueles em que foi ressecado o músculo. Todos os pacientes relataram melhora na estética facial com a técnica cirúrgica utilizada.
Palavras-chave: Hipertrofia de masseter; masseter
The masseter muscle hypertrophy is the muscle's uni or bilateral excessive development leading, in the majority of the cases, to an aesthetic discomfort to the patients(1).
According to Boyd (1953), appud Sposto et al.(2),the hypertrophy corresponds to an increase of the organ size, which is determined by the increase of the individual size of the cells or bundles with no variation in the quantity.
Several authors acknowledge the first report of masseter hypertrophy, in a 10 years old girl, to Legg (1880), appud Wade et al(3).
The ethiology of the masseter hypertrophy is not clear and has been accredited to unilateral masticatory efforts due to teeth loss, temporomandibular joint disorders, or parafunctional habits, such as bruxism or prolonged use of chewing gum. It affects generally young adults between the second and third life decades.
The masseter hypertrophy is normally follow by an osseous spur, which goes posteriorly to the mandibular angle, producing a square aspect to the patients face (4-6).
Normally, the patients seek for the physician complaining about uni or bilateral volume increase at the mandibular branch region. The pain is rarely reported and, when present, is well defined and located (2).
At the time of the clinical diagnosis, it is very important to ask the patient to tight the teeth and, therefore, during the palpation, it is possible to feel the muscle's hypertonicity. It is also through the palpation that one can verify the irregularity at the mandibular angle, as well as its increase. The presence of the osseous spur at the inferior portion of the affected side can be observed by means of X-ray(1).
The differential diagnosis is performed regarding parotid gland lesions, lipoma or osseous tumors.
We present our experience at the treatment of patients with masseter hypertrophy and a categorization to assist the treatment.
MATERIAL AND METHOD
From 1994 to 1998, 20 patients, 7 males and 13 females, with masseter hypertrophy diagnosis and that had undergone surgical treatment were assessed. The age varied from 15 to 30 years, with an average of 18.94 years.
The patients' complaints were related in 53% of the cases, to the aesthetic, and to the aesthetic related to the pain in 24%, and 23% related only to the pain, where 66% of the women related as a major problem only the aesthetic (Fig. 1).
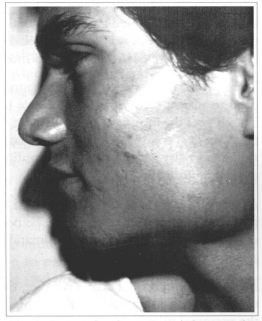
Fig. 1 - Patient showing masseteric hypertrophy due to bony mainly.
All the patients reported the volume increase as slow and progressive. In 72% of the cases, the volume increase was bilateral and, in 28%, unilateral. The patients reported the signals and/or symptoms' onset at an average age of 18 years, the women reported the symptoms earlier, at about 13 years old, and the volumetric increase of the masseter muscle was the first problem signal for the majority of the patients (70%).
None of the patients reported relatives with the same clinical symptoms. The prolonged use of chewing gum was reported in 20% of the cases, and 25% reported bruxism, while 55% of the patients did not report parafunctional habits.
At the preoperative, a panoramic X-ray and mandible PA were requested for all the patients in order to assess the presence of the osseous super.
Approximately 80% of the patients presented assymptomatic masticatory muscles and 20% presented a painful masseter during the palpation. The complaint was reported in 25% of the women and 20% of the men.
The preoperative buccal aperture varied from 36.00 mm to 56.00 mm; with an average of 48 mm. During the occlusion examination, 53% of the patients were completely dentulous; where 42% of the women and 80% of the men were completely dentulous. There were no edentulous patients.
All the patients underwent the surgical procedures under general anesthesia. The surgery was performed via extraoral approach at the first 5 cases and via intraoral approach at the last 15 cases.
The surgical procedure was performed depending on analyzed hypertrophy. Therefore, the patients with a most important osseous component (Fig. 1) underwent the ostectomy; the patients with a muscular component (Fig. 2) underwent the muscular ressection and the composed cases underwent the muscular mass reduction and osteotomy (Figs. 3a & 3b).
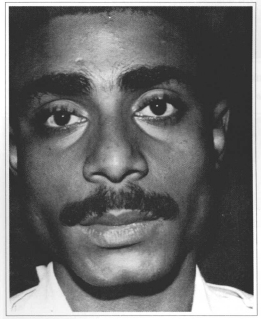
Fig. 2 - Patient showing masseteric hypertrophy due to muscle mainly.
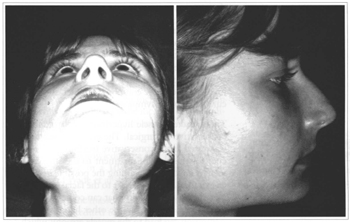
Figs. 3a & 3b - A: Patient with masseteric hypertrophy, notice the difference from right to left side. B: Profile view of the same patient.
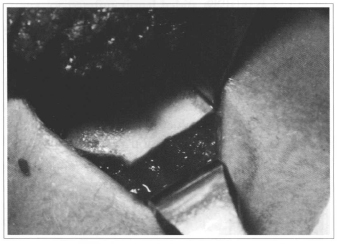
Fig. 4a - Transoperative view after bone and masseter resection.
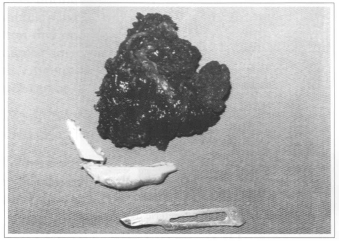
Fig. 4b - Portions of the ressected bone and muscle.
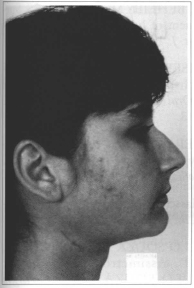
Fig. 5 - 3 months postoperative showing cervical region scar.
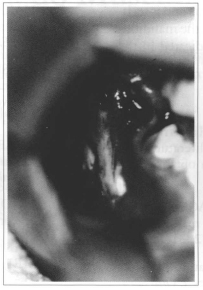
Fig. 6a - Transoperative view of the L ostectomy.
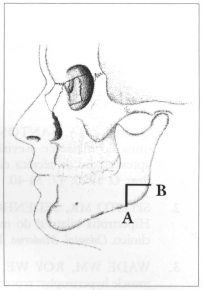
Fig. 6b - Scheme of the L ostectomy.
A bilateral withdrawal of the profound bundle of the masseter muscle and a bilateral osteotamy in inverted L were performed in 41% of the cases.
A bilateral withdrawal of the profound bundle of the masseter muscle and a bilateral oblique osteotamy of the mandibular angle were performed in 24% of the cases and just the bilateral withdrawal of the profound bundle was performed in 6% of the cases.
An osteotomy in inverted L, with minimal ressection of the masseter muscle, was performed in 29% of the cases.
All the muscular tissue samples were submitted to anatomicopathological examination, where 53% were from hypertrophic muscular tissue; 33% of striated rnuscle with no particularities and, in 13%, the result was not conclusive.
At the 2 months, the postoperative buccal aperture varied between 10.00 mm and 44.00 mm, with an average of 31 mm.
Regarding the aesthetic compliant, 87% of the patients were satisfied with the treatment and 13% did not notice any difference. And 100% of the patients with painful complaints reported an improvement of the symptoms. One female patient presented a submandibular scar hypertrophy that required a revision.
DISCUSSION
The masseter muscle hypertrophy is still a pathology with an unclear ethiology and that presents a very important aesthetic component, which is rarely concurrent with the symptoms.
The masseter muscle hypertrophy treatment can be conservative or surgical. The type A botulinus toxin is stressed at me conservative treatment. The preference for this type of treatment ta the surgical treatment is advocated regarding the possible necessity of an extraoral approach, risks to the facial nerve and me postaperative morbidity that can come with me surgical treatment, but, on me other hand, this protein infiltration can lead to the muscle atrophy, which can or not be reversible.
Nevertheless, the surgical treatment for the masseter muscle hypertrophy is the most accepted and effective one.
Giundice et al. (4) suggest a classification for the masseter muscle hypertrophy:
They also suggest the withdrawal of the parafunctional habit as a treatment for type II, the surgical correction for the type III, and the single follow up for the type I.
Hakan et al.(5) obtained a normal buccal aperture after 21 days and did not observed reciclivations and the postoperative edema lasted for 3 months.
There are no doubts regarding the diagnosis and surgical treatment of the masseter muscle hypertrophy. The clinic is the most important element for the diagnosis and it is complemented with the lateral X-ray of the mandibular angle in order to confirm the presence of an osseous spur.
As reported by Garcez & Santos(1), some authors prefer the submandibular, extraoral access because it presents a wider visualization of the mandibular angle and muscle.
Although the extraoral access is easier, the disadvantages of producing a scar at the skin and the risks of the marginal mandibular nerve lesion are clear and, therefore, with the use of the intraoral technique, advocated by Chee & Fei(7) and Wood(8), by means of a linear incision at the second molar sulcus up to the ascendant branch of the mandible, detachment and divulsion, it is possible to reach the profound bundle of the masseter muscle, where part of it is withdrew and, if necessary, this technique is associated to the mandibular's angle ostectomy or osteotomy(5).
In cases where there is no significant increase of the masseter muscle, Manganello et al.(9) advocate the use of the intraoral way followed by an inverted L osteotomy, without bone ressection. Despite the fact that me patient must be informed of the aesthetic characteristic of the deformity and that the skin incision will cause a scar, which also has an aesthetic characteristic and that'll vary according to the patient's tendencies, the extraoral approach must be used at facilities that don't have osteotomy or ostectomy surgical instruments (écarteur and saw) Nishida & Izuda(10) advocate the oblique ostectomy of the mandibular angle associated with the muscle's partial withdrawal by means of the intra-oral access.
Hakan et al.(5) stress the necessity of performing a helmet-like compressive bandage at the immediate postoperative to prevent complications such as hematomas and stress that an important edema is expected.
In our experience, we could notice that the pathology doesn't have a hereditary character and that it was bilateral in 41% of the cases.
The surgical treatment varied according to the presence or absence of an important osseous spur. We agree with Nishida & Izuda(10) regarding the ostectomy necessity but the muscular withdrawal depends on the hypertrophy degree, once it produces edema and mouth opening difficulties that can last for up to 6 months.
Once the surgeon possesses adequate instruments to the retraction and osteotomy, the intraoral access enables the surgeon to perform the surgery without leaving any scars.
CONCLUSION
According to our samples and literature, it was possible to observe that this pathology affects young adults, at an average age of 19 years plus female and white individuals.
The election of the technique to be used is directly related to the clinic and X-ray. Once the extraoral approach technique can leave a scar that affects the aesthetic, it is currently not indicated.
The muscular ressection is performed when the muscle is the responsible for the volume increase (group I); the muscular ressection and osteotomy are performed in the presence of an association of muscular increase and osseous spur (group II); and if the increase is due to an osseous spur, an osteotomy is performed (group III).
Once it satisfies the aesthetic requirements and is technically easy, the inverted L osteotomy at the mandibular angle, and not the ostectomy, is indicated in the majority of the cases.
REFERENCES
1. GARCEZ JA, SANTOS JS. Hipertrofia do músculo masseter. Revisão da literatura com apresentação de técnica cirúrgica optativa. Rev. Bras. O. 1990;47:34-40.
2. SPOSTO MR, SEDENHO N, ACETOZE PA. Hipertrofia bilateral do músculo masseter: caso clínico. Odontol. Moderno. 1983;12:31-4.
3. WADE WM, ROY WE. Idiopathic masseter muscle hypertrophy: report of cases. J. Oral Surg. 1971;29:196-200.
4. GIUNDICE M, MARRA A, BARBA A, PASSARIELLO N, D'ONOFRIO F. Ipertrofia dei masseteri: un raro caso, associato a cardiopatia ipertrofica. Minerva Stomatl. 1992;41:535-42.
5. HAKAN MM, BEHEIRY MG. HELMY ES. Surgical management of benign masseter hypertrophy. Egypt Dent. J. 1995;41:1435-40.
6. KESSEL LJ, ISERLOHN RADC. Benign bilateral masseteric hypertrophy with temporal muscle involvement. Oral Surg. Oral Med. Oral Pathol. 1970;30:450-3.
7. CHEE FL, FEI YJ. Surgical correction of masseter muscle hypertrophy by an intraoral approach. J. Oral Maxillofac. Surg. 1989;47:883-5.
8. WOOD G. Masseteric hypertrophy and its surgical correction. Br. Dent. J. 1982;152:16-7.
9. MANGANELLO-SOUZA LC, FREITAS RR, MERIDA JT. Assimetria de Face. In: MANGANELLO-SOUZA LC - Cirurgia Ortognática. Ed. Santos, 1998, p.146-158.
10. NISHIDA M, IZUDA T. Intraoral removal of the enlarged mandibular angle associated with masseteric hypertrophy. J. Oral Maxillofac. Surg. 1995;53:1476-9.
I - Buccomaxillofacial Head of Santa Casa de São Paulo.
II - Buccomaxillofacial Resident of Santa Casa de São Paulo.
III - Buccomaxillofacial Intern at Santa Casa de São Paulo.
IV - Buccomaxillofacial Assistant of Santa Casa de São Paulo.
Address for correspondence:
Luiz Carlos Manganello-Souza, MD
R. Itapeva, 500 Conj. l-C
01332-000 - São Paulo - SP Brazil
Phone: (55 11) 3176-3210
Work performed at the buccomaxillofacial department of the Santa Casa de São Paulo.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter