

Original Article - Year 2018 - Volume 33 -
Analysis of risk factors for the formation of seroma in classical abdominoplasty
Análise dos fatores de risco na formação de seroma em abdominoplastia clássica
ABSTRACT
Introduction: Abdominoplasty is one of the most common cosmetic surgeries in Brazil. The
complications of this procedure are diverse, with seroma being one of the
most frequent. The objective of this study was to identify the risk factors
for the formation of seroma, such as increased body mass index,
comorbidities, age, habits, and time of drain permanence.
Methods: This was a retrospective study in which the medical records of 94 patients
who underwent abdominoplasty at the Plastic Surgery and Burns Service of
Santa Casa de Misericórdia de São José do Rio Preto-SP between November 2010
and November 2013 were reviewed. The risk factors for the formation of
seroma were analyzed using Fisher's exact test and the Chi-square test, with
the significance level set at p < 0.05.
Results: Seroma was identified in 16 (17.02%) of the total patients (n = 94). No
statistical significance was observed between increased incidence of seroma
and increased BMI and other risk factors analyzed. Nevertheless, the time of
drain permanence showed a clinical relevance. The patients who were
maintained on the drain for > 1 day had a lower incidence of seroma.
Conclusion: The causes of seroma should be considered multifactorial. The risk factors
analyzed were not significantly related to the increased incidence of
seroma. However, drain permanence for >1 day was effective in the
prevention of seroma.
Keywords: Abdominoplasty; Seroma; Postoperative complications; Body mass index; Risk factors
RESUMO
Introdução: A abdominoplastia é uma das cirurgias estéticas mais realizadas no Brasil. As
complicações deste procedimento são diversas, sendo o seroma uma das mais
frequentes. O objetivo do trabalho é identificar fatores de risco para
formação de seroma tais como: índice de massa corporal (IMC), comorbidades,
idade, hábitos e tempo de permanência de dreno.
Métodos: Trata-se de um estudo retrospectivo com revisão de 94 prontuários de
pacientes submetidos à abdominoplastia clássica no Serviço de Cirurgia
Plástica e Queimados da Santa Casa de Misericórdia de São José do Rio
Preto-SP, entre novembro de 2010 e novembro de 2013. Os fatores de risco
para formação do seroma foram analisados utilizando-se o teste exato de
Fisher ou Qui-quadrado. Considerou-se como resultado estatisticamente
significativo o valor de p < 0,05.
Resultados: O seroma foi identificado em 16 pacientes (17,02%) do total da amostra (n =
94). Não se observou significância estatística ao relacionar a elevação na
incidência de seroma com o aumento do IMC, assim como os demais fatores de
risco analisados. Houve relevância clínica quanto ao tempo de permanência do
dreno. Pacientes que mantiveram o dreno por um período maior que um dia
tiveram incidência menor de seroma.
Conclusão: A formação do seroma deve ser considerada uma causa multifatorial. Os fatores
de risco analisados não demonstraram estatisticamente aumento na incidência
de seroma. Todavia, a permanência do dreno de sucção por um período maior
que um dia demonstrou ser eficaz na prevenção do seroma.
Palavras-chave: Abdominoplastia; Seroma; Complicações pós-operatórias; Índice de massa corporal; Fatores de risco
INTRODUCTION
Brazil ranks the highest in plastic surgeries worldwide, when nonsurgical procedures are also considered, second only to the United States. According to recent data from a study conducted by the International Society of Aesthetic Plastic Surgery (ISAPS) and published by the Brazilian Society of Plastic Surgery (SBCP), more than 23 million plastic surgeries were performed worldwide in 2013, of which 1,491,721 were performed in Brazil. Abdominoplasty accounts for 7.1% of these surgeries, second only to rhinoplasty, blepharoplasty, liposuction, and breast augmentation1.
Abdominoplasty is an effective and specific procedure for the improvement of body contour2. It has evolved over the years with the improvement of techniques that initially had high complication rates. Currently, it is considered safe and refined and with optimal results, and research is aimed at improving the performance of the procedure, reducing the occurrence of complications, and obtaining better results in the long term3. Small details, such as omphaloplasty, muscle plication, association with liposuction, and the development of techniques for detachment and treatment of the abdominal flap are now considered important in this procedure.
However, even with the evolution of the operative technique, seroma remains the most frequent early complication of this procedure. This fact motivated the study and practice of several methods such as the use of aspiration drains, reduced flap manipulation, fixation of the flap to the abdominal wall using quilting sutures, and use of postoperative (PO) compression sleeves to reduce this complication4.
OBJECTIVE
The objective of this study was to compare the development of seroma after abdominoplasty in patients operated using the Baroudi-Ferreira technique.
METHODS
This is a retrospective study conducted according to the principles established by the Declaration of Helsinki. Twenty patients undergoing abdominoplasty were evaluated at the Gaffrée and Guinle University Hospital (HUGG) of the Federal University of the State of Rio de Janeiro (UNIRIO) between April 2016 and September 2016. All patients were female, with ages ranging from 22 to 51 years.
All patients underwent a preoperative evaluation consisting of anamnesis, physical examination, and complementary exams. The exclusion criteria were as follows: age below 18 and more than 70 years, hematocrit below 37%, smoking, body mass index (BMI) ≥30 kg/m2, large amount of weight losses, abdominal wall hernias, surgeries and/or previous abdominal scars (except cesarean section/Pfannenstiel incision), and surgical risk higher than ASA II.
After signing the Informed Consent Form, the patients were alternately distributed into two groups in order of arrival:
- Group A (n = 10): Abdominoplasty with the use of quilting sutures (Baroudi-Ferreira technique).
- Group B (n = 10): Abdominoplasty without the use of quilting sutures
Student’s t-test was used for statistical analysis, considering p-values < 0.05 as statistically significant.
Operative technique
All patients were administered general anesthesia, and preventive care for deep venous thrombosis (DVT) was implemented according to individual risk factors.
Subsequently, abdominoplasty was performed with a periumbilical incision, followed by suprapubic incision, extending laterally almost to the iliac crests in a previously demarcated area.
A dermis-fat flap of the muscle aponeurosis was detached in both groups using electrocautery at 40 watts for dissection and coagulation throughout the supra-aponeurotic plane. The central and lateral regions of the flap, extending almost to the anterior axillary line in the infraumbilical region, were detached. Subsequently, regions up to 3 cm inferior to the xiphoid appendix and 4 cm lateral to the medial margins of the rectus abdominis muscles were detached, similarly to that described by other authors3,4.
Muscle diastasis was corrected by plication of the anterior lamina of the rectus abdominis sheath in a single plane with three inverted “X” supraumbilical and two infraumbilical “X” points followed by “lock-stitch suture” throughout the plication area, using a 2-0 nylon monofilament.
After resection of the dermis-fat flap excess, marking of the neoumbilicus position, and checking for bleeding, quilting sutures were made in 16 patients in Group A, as recommended by Baroudi-Ferreira5,6. Four of them were made in the supraumbilical midline, and 12 were evenly distributed in the infraumbilical region, different from the procedure performed in Group B. The suture was followed by planes and surgical dressing.
It is important to point out that no liposuction was performed and no aspiration or any other drain was used in the patients in this study. Furthermore, low-molecular-weight heparin was not regularly used in the preoperative and PO periods, but calf massaging and early ambulation were performed after the surgical procedure.
Antibiotic medication such as cefadroxil and analgesia were used in the PO period. The dressings were applied during medical consultation. Lymphatic drainage was recommended from the 5th PO day (POD), and the patients were recommended to use a girdle for 30 days.
PO evaluation consisted of consultations on the following PODs: 7th, 15th, 21st, 45th, and 60th. The presence of seroma was evidenced by symptoms such as pain, sensation of fluid and “weight” in the abdomen and the presence of bulging or fluctuation detected during palpation upon physical examination or by active inspection using the aspiration method with a syringe in suspected cases.
The presence of seroma was considered positive when the volume of aspirated fluid was ≥10 mL. Other signs such as hyperemia, edema, and local heat and complications such as dehiscence and epitheliolysis, associated or not with the presence of seroma, were also considered for the analysis.
Photographic documentation was performed preoperatively, on the 45th, 90th, and 180th PODs.
RESULTS
Twenty female patients were studied, all of them not meeting the exclusion criteria mentioned above.
In Group A, the age of the patients ranged from 22 to 47 years (mean = 33.6 years), BMI ranged from 21 to 25.4 kg/m2 (mean = 23.7 kg/m2), and mean time of surgery was 170 min. In Group B, the age of the patients ranged from 25 to 51 years (mean = 39.1 years), BMI ranged from 20.3 and 25.5 kg/m2 (mean = 23.8 kg/m2), and mean time of surgery was 163 min, as shown in Table 1.
| Group A | Group B | Total | |
|---|---|---|---|
| Age (years) | 33.6 ± 8 | 39.1 ± 7.6 | 36.4 ± 8.1 |
| BMI (kg/m2) | 23.7 ± 1.34 | 23.8 ± 1.6 | 23.7 ± 1.45 |
| Surgical time (min) | 170 ± 17.2 | 163 ± 25 | 166 ± 21.1 |
There was no statistical difference between the two groups regarding age (p = 0.09), BMI (p = 0.78), and time of surgery (p = 0.45).
Two patients (20%) in Group A had seroma, which was significantly lower (p = 0.05) than that in Group B, in which seven patients (70%) were diagnosed with seroma. The mean volume observed was 26.5 mL in Group A but 146.5 mL in Group B. The highest volume aspirated in Group A was 130 mL, on the 15th POD, whereas in Group B, it was 230 mL, on the 21st POD of a total of 590 mL aspirated over 21 days postoperatively from the same patient, who had the largest seroma of not only the group but also the whole sample. From the 21st POD, seroma was no longer detected in this patient.
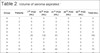
Whereas the highest mean volume in Group A (16 mL) was observed on the 15th POD, the highest mean volume in Group B (59.5 mL) was observed on the 7th POD. However, no statistical difference was observed regarding the total volume of seroma aspirated (p = 0.12) when comparing both groups. From the 45th POD, seroma was no longer observed in Group A, whereas in Group B, only one patient had seroma on the 45th POD. Then, 45 mL of serous fluid was aspirated in that time, and on the 60th POD, no seroma was observed, as shown in Table 2.
| Group | Patients | 7th POD (mL) | 15th POD (mL) | 21st POD (mL) | 45th POD (mL) | 60th POD (mL) | Total (mL) |
|---|---|---|---|---|---|---|---|
| A | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| A | 2 | 0 | 0 | 0 | 0 | 0 | 0 |
| A | 3 | 0 | 0 | 0 | 0 | 0 | 0 |
| A | 4 | 0 | 0 | 0 | 0 | 0 | 0 |
| A | 5 | 0 | 0 | 0 | 0 | 0 | 0 |
| A | 6 | 20 | 130 | 45 | 0 | 0 | 195 |
| A | 7 | 0 | 0 | 0 | 0 | 0 | 0 |
| A | 8 | 0 | 0 | 0 | 0 | 0 | 0 |
| A | 9 | 0 | 0 | 0 | 0 | 0 | 0 |
| A | 10 | 0 | 30 | 40 | 0 | 0 | 70 |
| B | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| B | 2 | 200 | 160 | 230 | 0 | 0 | 590 |
| B | 3 | 130 | 80 | 0 | 0 | 0 | 210 |
| B | 4 | 0 | 0 | 0 | 0 | 0 | 0 |
| B | 5 | 40 | 0 | 0 | 0 | 0 | 40 |
| B | 6 | 20 | 0 | 0 | 0 | 0 | 20 |
| B | 7 | 10 | 0 | 0 | 0 | 0 | 10 |
| B | 8 | 195 | 100 | 30 | 0 | 0 | 325 |
| B | 9 | 0 | 135 | 90 | 45 | 0 | 270 |
| B | 10 | 0 | 0 | 0 | 0 | 0 | 0 |
One patient in Group A (10%) had a hematoma detected and drained on the 1st POD. This patient also had the earliest development of seroma and the greatest volume aspirated in this group. One patient in Group B (10%) had a hematoma detected and drained on the 7th POD. This patient also had the greatest volume of seroma aspirated of not only the group but also the whole sample.
Concerning the presence of other complications, in Group A, umbilical stenosis was observed in 2 patients (20%), scar hypertrophy/hyperchromia in 3 (30%), scar dehiscence in 1 (10%), epitheliolysis in 1 (10%), and dog ear in 1 (10%), while in Group B, it was observed in 2 (20%), 2 (20%), 4 (40%), 3 (30%), and 1 patient (10%), respectively. Patients in both groups who had umbilical stenosis and scars with unsatisfactory aesthetic appearance underwent a new surgical procedure and had to wait six months postoperatively to have their scars retouched.
No anesthetic complications were recorded in any of the operated cases. The only systemic complication was observed in a patient in Group B, who was diagnosed with DVT on the 13th POD by clinical examination and in whom resolution of symptoms after medical treatment was confirmed by Doppler ultrasonography. This patient had no seroma or any other complication.
DISCUSSION
Seroma is characterized by the accumulation of exudative fluids under the abdominal flap. It is considered the most frequent early complication of this procedure, with an incidence ranging from 1 to 57% and a mean of 10% reported in most studies7,8. The mechanisms associated with seroma formation are section of lymphatic channel, dead space due to the detachment of the dermis-fat flap, shear forces between the flap and aponeurosis, and release of inflammatory mediators9-11.
Bozola and Psillakis12 reported that the incidence of seroma is associated with the extension of surgery, i.e., the greater the complexity of the surgery, the greater the predisposition to this complication. Nahas et al.7 evaluated 21 individuals undergoing abdominoplasty and quilting sutures with ultrasonography and found a mean volume of 8.2 mL of seroma after two weeks of surgery.
The main factors predisposing to seroma formation are obesity or a large amount of weight loss, leading to changes in the lymphatic system (38% in obese versus 19% in normal weight individuals)13; extension of the abdominal flap detachment area, causing an increase in the dead space; previous supraumbilical scar, hindering lymphatic drainage; and liposuction14.
Seroma accumulation causes an increase in local pressure, which can lead to other complications such as operative wound dehiscence, necrosis, spontaneous surgical wound drainage, and infection15,16, in addition to the possibility of chronic untreated seromas evolving with the formation of a fibrous capsule around them (pseudobursa), leading to deformities of the abdominal wall17, a condition that requires surgical treatment15,16.
Because of this frequent complication, several studies aimed at reducing the incidence of seroma and, consequently, other complications that, if not directly related, are associated with it have been conducted. The use of quilting sutures, as recommended by Baroudi and Ferreira5,6, have been associated with the reduction of both the incidence and volume of seroma drained in abdominoplasty.
This is possible due to the reduction of the “dead space” created by the detachment of the dermis-fat flap and reduction of the flap sliding on the aponeurotic plane, eliminating two of the main predisposing factors to the development of seromas. Moreover, the attachment of the dermis-fat flap to the aponeurosis muscle reduces the tensile forces exerted by the flap on the pubic scar, reducing the prevalence of dehiscences and poorly positioned and enlarged scars3.
Considering the statement of Borile et al.18 and Nahas et al.7 that the use of drains did not reduce the incidence of seroma, as it is a phenomenon occurring between the 2nd and 3rd PO week, this study aimed to compare the development of seroma in abdominoplasty with and without quilting sutures without the use of drains of any kind.
Although studies have indicated that ultrasonography has been the method of choice for the diagnosis of seroma after abdominoplasty, this examination was not included in the follow-up because of the difficulty of its standardization and performance in the patients of this study. Thus, the presence of seroma was verified by clinical examination, which may have reduced diagnostic sensitivity, especially in the case of small seromas, as described by other authors4.
The incidence of seroma was significantly lower in Group A than in Group B, and both groups had a mean above that accepted by most authors, which is around 10%7,8. Although the mean volume of seroma aspirated in Group A was lower than that in Group B, no statistical significance was found when this item was evaluated.
It was observed that the patients in both groups with the earliest development of seroma (7th POD) and greater volume of seroma aspirated were those who had hematomas, suggesting an association of this complication with onset time and volume of seroma aspirated.
The highest volume of seroma aspirated in Group A was observed later and for a shorter duration than in Group B, indicating that quilting sutures not only decrease the volume of seroma produced but are also associated with later onset and earlier resolution with a lower number of stitches (16 stitches) than that reported in other studies (40 to 45 points)3.
Similar to the findings of other studies, there was no statistical difference regarding BMI and age in both groups4, and even with data showing that the use of quilting sutures increases the time of surgery by 30 min3, no statistical difference was observed between the groups in the time of surgery, justifying their use when the incidence of complications such as dehiscence and epitheliolysis of scars was reduced.
CONCLUSION
In this study, the development of seroma in abdominoplasty was significantly lower in the group in which the Baroudi-Ferreira technique was used.
COLLABORATIONS
|
RGSC |
Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents. |
|
AMSA |
Final approval of the manuscript; writing the manuscript or critical review of its contents. |
|
RKAF |
Conception and design of the study; writing the manuscript or critical review of its contents. |
|
RCR |
Analysis and/or interpretation of data; writing the manuscript or critical review of its contents. |
REFERENCES
1. Sociedade Brasileira de Cirurgia Plástica. Pesquisa ISAPS; 2014 [acesso 2018 Mar 5]. Disponível em: http://www2.cirurgiaplastica.org.br/2014/07/29/de-acordo-com-a-isaps-brasil-lidera-ranking-de-cirurgias-plasticas-no-mundo/
2. Baroudi R, Soncini JA. Revisão da técnica de abdominoplastia com dissecção reduzida e fixação com pontos de Baroudi. Rev Bras Cir Plást. 2016;31(2):166-71.
3. Boggio RF, Almeida FR, Baroudi R. Pontos de adesão na cirurgia do contorno corporal. Rev Bras Cir Plást. 2011;26(1):121-6. DOI: http://dx.doi.org/10.1590/S1983-51752011000100022
4. Di Martino M, Nahas FX, Novo NF, Kimura AK, Ferreira LM. Seroma em lipoabdominoplastia e abdominoplastia: estudo ultrassonográfico comparativo. Rev Bras Cir Plást. 2010;25(4):679-87. DOI: http://dx.doi.org/10.1590/S1983-51752010000400021
5. Baroudi R, Ferreira CA. Seroma: how to avoid it and how to treat it. Aesthet Surg J. 1998;18(6):439-41. PMID: 19328174 DOI: http://dx.doi.org/10.1016/S1090-820X(98)70073-1
6. Baroudi R, Ferreira CA. Contouring the hip and the abdomen. Clin Plast Surg. 1996;23(4):551-72.
7. Nahas FX, Ferreira LM, Ghelfond C. Does quilting suture prevent seroma in abdominoplasty? Plast Reconstr Surg. 2007;119(3):1060-4.
8. Grazer FM, Goldwyn RM. Abdominoplasty assessed by survey with emphasis on complications. Plast Reconstr Surg. 1977;59(4):513-7. PMID: 847027
9. Kulber DA, Bacilious N, Peters ED, Gayle LB, Hoffman L. The use of fibrin sealant in the prevention of seromas. Plast Reconstr Surg. 1997;99(3):842-9. DOI: http://dx.doi.org/10.1097/00006534-199703000-00034
10. Hafezi F, Nouhi A. Safe abdominoplasty with extensive liposuctioning. Ann Plast Surg. 2006;57(2):149-53. DOI: http://dx.doi.org/10.1097/01.sap.0000215246.49308.17
11. Trufino AJ. Estudo comparativo de abdominoplastias com drenagem a vácuo e sem drenagem, mas com pontos de adesão. Rev Bras Cir Plást. 2015;30(4):522-32.
12. Bozola AR, Psillakis JM. Abdominoplasty: a new concept and classification for treatment. Plast Reconstr Surg. 1988;82(6):983-93. PMID: 2974166 DOI: http://dx.doi.org/10.1097/00006534-198812000-00008
13. Kim J, Stevenson TR. Abdominoplasty, liposuction of the flanks, and obesity: analyzing risk factors for seroma formation. Plast Reconstr Surg. 2006;117(3):773-9. DOI: http://dx.doi.org/10.1097/01.prs.0000200056.57357.3f
14. Matarasso A. Liposuction as an adjunct to a full abdominoplasty. Plast Reconstr Surg. 1995;95(5):829-36. DOI: http://dx.doi.org/10.1097/00006534-199504001-00010
15. Keramidas EG, Rodopoulou S, Khan U. Pseudo-cyst formation after abdominoplasty combined with liposuction: a case report and review of the literature. Eur J Plast Surg. 2006;28:400-2. DOI: http://dx.doi.org/10.1007/s00238-005-0796-1
16. Ersek RA, Schade K. Subcutaneous pseudobursa secondary to suction and surgery. Plast Reconstr Surg. 1989;85(3):442-5. PMID: 2304996
17. Zecha PJ, Missotten FE. Pseudocyst formation after abdominoplasty--extravasations of Morel-Lavalleé. Br J Plast Surg. 1999;52(6):500-2. DOI: http://dx.doi.org/10.1054/bjps.1999.3154
18. Borile G, Pavelecini M, Dreher R, Chem E, Chem RC. The use of suction drains in abdominal dermolipectomy: a randomized clinical trial. Plast Reconstr Surg. 2008;121(4):228e-9e. PMID: 18349614 DOI: http://dx.doi.org/10.1097/01.prs.0000305389.29451.b0
1. Universidade Federal do Estado do Rio de
Janeiro, Rio de Janeiro, RJ, Brazil.
2. Hospital Universitário Gaffrée e Guinle, Rio de
Janeiro, RJ, Brazil.
Corresponding author: Rafael Garrido Souza
Costa
Rua Mariz e Barros, 775 - Maracanã
Rio de Janeiro, RJ, Brazil
Zip Code 20270-001
E-mail: rgscosta@gmail.com
Article received: November 27, 2017.
Article accepted: May 17, 2018.
Conflicts of interest: none.



 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter