

Original Article - Year 2018 - Volume 33 -
McGregor flap: an alternative for lower eyelid and periorbital region reconstruction
Retalho de McGregor: uma alternativa para reconstrução de pálpebra inferior e região periorbital
ABSTRACT
Introduction: Lower eyelid reconstruction is a challenge for plastic surgeons. It requires
knowledge of various surgical techniques and anatomy. In 1973, McGregor
published the lateral periorbital zetaplasty technique, which proved to be
an excellent alternative within the therapeutic reconstructive arsenal. The
objective is to demonstrate the clinical applicability of the McGregor flap
as an option for reconstruction of lower eyelid and periorbital region
defects.
Methods: In this retrospective, descriptive, and analytical study, seven patients
underwent excision of cutaneous malignant tumors of the lower eyelid and
adjacent regions and reconstruction using the McGregor flap between April
2010 and October 2016 at the Plastic Surgery Clinic of Hospital Felício
Rocho, Belo Horizonte, MG.
Results: The age of the patients ranged from 38 to 79 years, with an average of 65.4
years. Five of the seven patients (71.4%) were women. At the
anatomopathological examination, 85.7% of the cutaneous tumors were basal
cell carcinoma, and 14.3% (n = 1) were adnexal microcystic carcinoma. Four
patients underwent Mohs micrographic surgery for excision of the lesions. In
one patient, the Matsuo technique was used for palpebral reconstruction of
the posterior lamella. In the follow-up averaging 36.3 months, the
conditions of the six patients (85.7%) progressed well without
complications, with satisfactory results; one patient developed
postoperative ectropion owing to the deformation of the cartilage graft of
the ear used in the reconstruction.
Conclusion: The McGregor flap presented adequate clinical applicability, making it an
excellent alternative for reconstruction of lower eyelid defects and
adjacent tissues with good aesthetic and functional results.
Keywords: Surgical flaps; Reconstructive surgical procedures; Eyelids
RESUMO
Introdução: A reconstrução da pálpebra inferior é um desafio para o cirurgião plástico.
Exige um conhecimento das variadas técnicas cirúrgicas e da anatomia. Em
1973, McGregor publicou a zetaplastia periorbital lateral que se mostra como
excelente alternativa dentro do arsenal terapêutico reconstrutivo. O
objetivo é demonstrar aplicabilidade clínica do retalho de McGregor como
opção para reconstrução de defeitos da pálpebra inferior e região
periorbital.
Métodos: Estudo retrospectivo, descritivo e analítico de sete pacientes que foram
submetidos à excisão de neoplasias cutâneas da pálpebra inferior e regiões
adjacentes, sendo utilizado para reconstrução do defeito cirúrgico o retalho
de McGregor, entre abril de 2010 e outubro de 2016, na Clínica de Cirurgia
Plástica do Hospital Felício Rocho, Belo Horizonte, MG.
Resultados: A idade dos pacientes variou entre 38 e 79 anos, com média de 65,4 anos,
sendo cinco (71,4%) do sexo feminino. Ao exame anatomopatológico, 85,7% das
neoplasias eram carcinoma basocelular e um caso (14,3%) correspondia a
carcinoma microcístico anexial. Quatro pacientes foram submetidos à cirurgia
micrográfica de Mohs para excisão da lesão. Em um caso foi utilizada a
técnica de Matsuo para reconstrução palpebral da lamela posterior.
Seguimento com média de 36,3 meses, seis pacientes (85,7%) evoluíram bem sem
intercorrências com resultado satisfatório, um paciente evolui com ectrópio
no pós-operatório por deformação do enxerto de cartilagem da orelha
utilizado na reconstrução.
Conclusão: O retalho de McGregor apresentou aplicabilidade adequada, sendo uma excelente
alternativa para reconstrução de defeitos da pálpebra inferior e tecidos
adjacentes, com bons resultados estético e funcional.
Palavras-chave: Retalhos cirúrgicos; Procedimentos cirúrgicos reconstrutivos; Pálpebras
INTRODUCTION
Reconstruction of the lower eyelid is a challenge for plastic surgeons. It requires knowledge of various surgical techniques and anatomy to obtain satisfactory functional and aesthetic results1-3.
Eyelid defects can be divided into congenital and acquired and can be due to diverse etiologies, with cutaneous tumors being one of the most prevalent, especially the non-melanoma type4-8.
Basal cell carcinoma (BCC) is the most prevalent of the non-melanoma cutaneous tumors and has a slow growth rate. Although it is not aggressive, BCC can cause important sequelae in adjacent tissues when treated late or inappropriately9.
Periorbital tumors represent 10% of cutaneous tumors. BCC is the most common neoplasm in the periorbital region, accounting for 80-90% of palpebral tumors. The lower eyelid and the medial canthus are the most commonly affected regions. These periorbital cutaneous tumors can be difficult to manage; nevertheless, they are commonly treated with surgical excision10.
Several lower eyelid reconstruction techniques have been developed over the last decades. The choice of the reconstruction technique should be guided by the size of the defect and involvement of the anterior and posterior lamellae. Simple closure should be conducted when possible, and lateral canthotomy may aid in the medial advancement of tissues11-13.
In 1966, Mustardé14 used several techniques according to the principle of advancement of the lateral skin of the face in the medial direction for correction of defects of the lower eyelid. There is sagging skin in the lateral region of the face. Its advancement is limited, and if no measures are taken to reduce tension in the flap, it will tend to return to the original position.
In 1973, McGregor15 proposed a technique for lower eyelid defects consisting of lateral periorbital zetaplasty to advance the tissues medially with the intention of reducing the tension in the flap. It is shown as an excellent alternative within the therapeutic reconstructive arsenal for complex lower eyelid defects.
OBJECTIVE
To demonstrate the clinical applicability of the McGregor flap as an option for reconstruction of defects of the lower eyelid and periorbital region.
METHODS
This retrospective, descriptive, and analytical study was based on the review of medical records and photographic documentation of seven patients submitted to excision of cutaneous tumors of the lower eyelid and adjacent regions. The surgical defects were reconstructed using the McGregor flap between April 2010 and October 2016 at the Plastic Surgery Clinic of Hospital Felício Rocho, Belo Horizonte, MG.
The following criteria were analyzed: age at the date of surgery, sex, lesion topography, pathological diagnosis of the lesion, date of and adopted surgical procedure, follow-up, and any complications related to the procedure.
Data were entered into the Microsoft Office Excel spreadsheet software for statistical analysis. The related literature was reviewed, and the databases consulted were PubMed and LILACS.
The principles of the Declaration of Helsinki revised in 2000 and Resolution 196/96 of the National Health Council were followed, and the patients analyzed completed the informed consent form. No conflicts of interest were observed, and there were no sources of financing.
Surgical technique
With the patients under mild sedation and local anesthesia, the surgical procedure began with creation of a lateral incision following the curvature of the eyelid, which extended to the anterior region of the pre-auricular hair-line, with the length of the incision being dependent on the width of the defect to be compensated. The curvature of the incision was important to provide a vertical length appropriate to the flap.
Zetaplasty was performed at the lateral end of the incision, with the width of the defect corresponding to the central limb of the Z. The lateral descending limb and the ascending limb of the Z had the same length as the common limb and formed an angle of 60º with the latter (Figure 1).
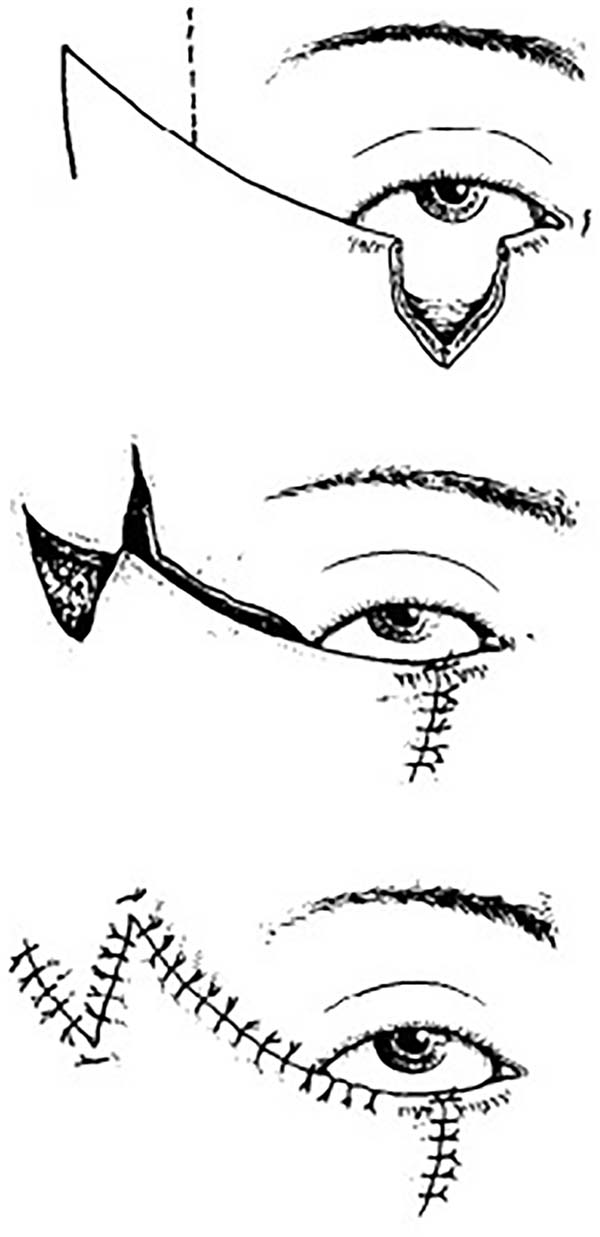
The detachment of the flaps followed the subcutaneous dissection plane. Lateral canthotomy was performed for advancement of the flap and covering of the eyelid defect. After interpolation of the flaps, any excess skin was trimmed.
RESULTS
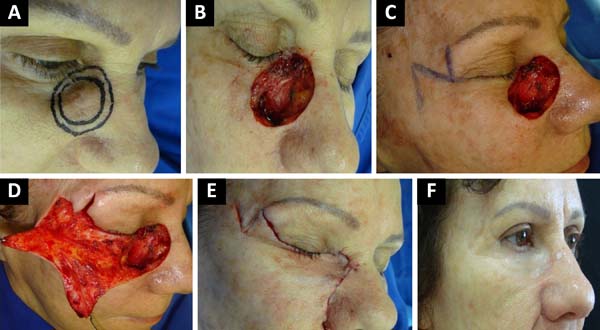
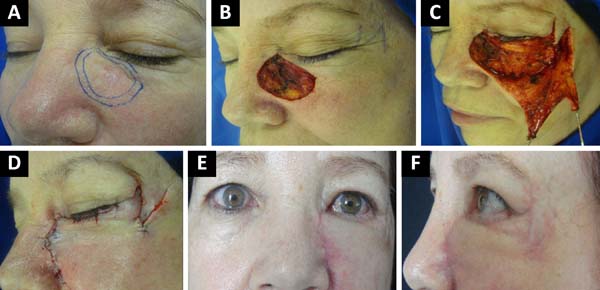
Between April 2010 and October 2016, seven patients underwent excision of cutaneous malignant tumors of the lower eyelid and reconstruction of the surgical defect using the McGregor flap (Table 1 and Figure 2, 3 and 4). The patients’ age ranged from 38 to 79 years, with an average of 65.4 years. The study included five female patients (71.4%) and two male patients (28.6%).
| Patient | Age (Years) |
Sex | Lesion location | Anatomopathological Diagnosis | Surgery | Follow-up/ Complications |
|---|---|---|---|---|---|---|
| 1 | 79 | Male | Lower right eyelid | Nodular BCC | 08/04/2010 Excision of the lesion with sacrifice of the catheterized lacrimal canaliculus + McGregor flap |
52 months Without complications |
| 2 | 69 | Female | Lower right eyelid | Sclerodermiform BCC | 30/03/2011 Excision of the lesion + Matsuo's technique + McGregor flap |
14 months Ectropion from deformation of the cartilage graft |
| 3 | 66 | Female | Lower right eyelid and nasal region | Adnexal microcystic carcinoma | 11/04/2011 Mohs micrographic surgery + McGregor flap |
71 months Without complications |
| 4 | 77 | Male | Right lateral region of the nasal dorsum | Sclerodermiform BCC | 04/10/2013 Mohs micrographic surgery + McGregor flap |
44 months Without complications |
| 5 | 59 | Female | Left medial orbital zygomatic margins | Solid BCC | 16/12/2013 Mohs micrographic surgery + McGregor flap |
42 months Without complications |
| 6 | 38 | Female | Lower right eyelid | Nodular BCC | 24/09/2015 Mohs micrographic surgery + McGregor flap |
22 months Without complications |
| 7 | 70 | Female | Lower left eyelid | Solid BCC | 21/10/2016 Excision of lesion + McGregor flap |
9 months Without complications |
In relation to the topography of the lesions, one was located on the left medial orbital zygomatic margin (14.3%), one on the right lateral region of the nasal dorsum (14.3%), one on the right lower eyelid and nasal region (3%), three on the lower right eyelid (42.8%), and one on the lower left eyelid (14.3%).
Based on the pathological examination findings, two lesions were diagnosed as solid BCC (28.6%), two as sclerodermiform BCC (28.6%), and two as nodular BCC (28.6%) (85.7% BCC in total) and one as adnexal microcystic carcinoma (AMC) (14.3%).
Four patients underwent Mohs micrographic surgery for lesion excision and reconstruction using the McGregor flap (57.1%); the other three patients underwent conventional lesion excision and reconstruction using the McGregor flap (42.9%). In one patient, the lacrimal canaliculi had to be sacrificed and catheterized.
In another patient, the Matsuo et al.16 technique was used for palpebral reconstruction of the posterior lamella using a cartilaginous graft of the ear concha.
The patients were followed up for periods varying from 9 to 71 months with an average of 36.3 months. During the follow-up, there were no cases of tumor recurrence. The conditions of the six patients progressed well without complications, with satisfactory results (85.7%); however, one patient evolved with postoperative ectropion (14.3%) due to deformation of the graft cartilage of the ear used in the Matsuo technique for reconstruction. This patient refused correction of the complication.
DISCUSSION
The number of diagnoses of non-melanoma skin cancer is higher than that of all other malignancies combined; this has become a relevant public health issue owing to the increasing incidence and costs associated with this type of cancer17. This fact brings our attention to the possibility of risk reduction associated to preventive measures and promotion of healthy sun exposure.
One patient was diagnosed with AMC, which is an uncommon tumor with approximately 700 cases described in the literature worldwide. It is a neoplasia of the eccrine sweat glands with a slow growth and a low index of metastases that affect the head and neck. Owing to its subclinical evolution, AMC is often confused with benign cutaneous tumors, resulting in late diagnoses and higher rates of incomplete treatment. Recurrences may occur up to 30 years after excision; therefore, prolonged follow-up is recommended18.
The histological distribution of the tumors excised in this study was similar to that in the literature on periorbital tumors with predominance of BCC (85.7% of the cases). The most common site of the tumors also coincided with that of the literature, with 71.4% of the tumors being found in the lower eyelid, 14.3% in the zygomatic margin, and 14.3% in the nasal dorsum18.
BCC affecting the periorbital region has a higher rate of recurrence than other topographies, most of which are not locally aggressive and invasion of the orbit occurs in less than 5% of cases19. In this study, no case of tumor recurrence was identified, although some patients had a short-term follow-up.
The preservation of healthy tissues as well as the high cure rates are important considerations in the surgical treatment of periorbital cutaneous tumors. The surgical treatment of BCC commonly includes techniques, such as curettage, conventional excision, cryosurgery, laser-associated cryosurgery, and Mohs micrographic surgery.
The conventional resection of the cutaneous tumor lesions in this series represented 43% of the cases. The literature reveals that this modality remains the most commonly used procedure, accounting for 75% of surgeries performed on BCC20.
In the present study, Mohs micrographic surgery was performed in four patients (57%). Surgical indications depend on histology, size, and topography of the lesion and previous treatments21. Studies show that this approach has higher cure rates. The rate of BCC recurrence 5 years after conventional surgery is 10 to 17%, whereas that of tumors resected by Mohs micrographic surgery is 1 to 5.6%22.
Eyelid reconstruction aims to protect the cornea, preserve sight, and maintain facial symmetry. The choice of the technique to be used should take into account the size and position of the defect and the quality of the adjacent skin. Options for reconstruction include grafts and various flaps. It is important to consider the traction vectors of the flaps over the eyelid to avoid complications, such as lagophthalmos and ectropion. The color and texture of the skin selected for grafts and flaps should also be considered to preserve the function and aesthetics of the eyelid23-25.
The technique described in 1973 by McGregor was originally indicated for the reconstruction of V-shaped defects up to two thirds of the width of the eyelid, being applied to both the lower and upper eyelids. After 15 years of using the flap, McGregor presented good surgical results, with good-quality scars and lateral eyelids with a natural appearance15. This study used the technique presented by McGregor as a basis for reconstruction of the lower eyelid and adjacent regions with satisfactory results.
This flap minimizes the tension of the lower eyelid, recruiting tissue laterally to the defect and not below. Since it involves minor detachment of the tissues, this flap has shown lower risks of seroma, hematoma, and necrosis than the technique of Mustardé.
In 2010, Chedid et al.26 conducted a retrospective study that analyzed 137 patients who underwent resection of neoplastic lesions of the lower eyelid and immediate reconstruction at the National Cancer Institute in Rio de Janeiro between 2005 and 2010. In 11.2% of the patients, the selected reconstruction technique was the McGregor flap.
In 2013, Tomassini et al.27 investigated seven patients who underwent periorbital tumor excision and reconstruction with periorbital zetaplasty and observed good functional and aesthetic results, with no need for reoperation in any of the cases.
In 2015, Mukundan et al.28 described a series of nine patients with successful reconstructed malar eyelid defects using the McGregor technique associated with postoperative hyperbaric oxygen therapy.
In 2016, Özkaya Mutlu et al.19 and Uemura et al.29 each showed a case of reconstruction with lateral periorbital zetaplasty, obtaining satisfactory results.
In addition to the lateral periorbital zetaplasty for anterior lamellar reconstruction, the technique described by Matsuo et al.16 in 1987 was used in one patient in this study to reconstruct the posterior lamella using a cartilage graft from the ear concha. In this technique, the cartilage in contact with the bulbar conjunctiva undergoes spontaneous epithelization, eliminating the need for mucosal grafting to reconstruct the conjunctiva.
The epithelization of the cartilage accompanied by the perichondrium is faster and more effective than that when the bare cartilage is used. Consequently, this technique reduces the surgical time and morbidity associated with the mucosal graft donor area. Furthermore, the choice of the cartilage of the ear shell is interesting because of the shape of the structure that adapts well to the palpebral region, delicacy of the tissue, and ease of obtaining the graft.
Preservation of eyelid function is one of the main objectives of reconstruction, allowing protection of the eyeball and tear system. Thus, measures should be taken during surgical planning to avoid complications, such as ectropion, entropion, epiphora, lagophthalmos, and exposure of the cornea. Among the patients included in this study, one developed ectropion. In this patient, the Matsuo technique was used; the complication may be related to late deformation of the cartilage graft.
Ectropion increases exposure of the palpebral and bulbar conjunctivae, predisposing patients to dry eye and tearing. As previously mentioned in the surgical technique of the McGregor flap, the ascending curvature of the incision and the direction of the traction vectors horizontally or laterally can reduce the risks of postoperative ectropion.
CONCLUSION
The McGregor flap presented an adequate clinical applicability in the reported series, making it an excellent alternative to compose the arsenal of surgical techniques of plastic surgeons for the reconstruction of defects of the lower eyelid and adjacent tissues with good aesthetic and functional results.
COLLABORATIONS
|
ACMA |
Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents. |
|
JCRRA |
Analysis and/or interpretation of data; final approval of the manuscript; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents. |
|
NAP |
Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents |
|
LCJ |
Analysis and/or interpretation of data; statistical analyses; conception and design of the study; writing the manuscript or critical review of its contents. |
|
EHP |
Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; writing the manuscript or critical review of its contents. |
|
RPLF |
Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript. |
|
AFSF |
Analysis and/or interpretation of data; final approval of the manuscript; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents. |
REFERENCES
1. Iglesias ME, Santesteban R, Larumbe A. Oncologic surgery of the eyelid and orbital region. Actas Dermosifiliogr. 2015;106(5):365-75. PMID: 25701895 DOI: http://dx.doi.org/10.1016/j.ad.2014.11.011
2. Alves JCRR, Liu RP, Silva Filho AF, Pereira NA, Carvalho EES. Reconstrução palpebral com enxerto de cartilagem autóloga de concha de orelha. Rev Bras Cir Plást. 2012;27(2):243-8 DOI: http://dx.doi.org/10.1590/S1983-51752012000200013
3. Holds JB. Lower eyelid reconstruction. Facial Plast Surg Clin North Am. 2016;24(2):183-91. DOI: http://dx.doi.org/10.1016/j.fsc.2016.01.001
4. Apalla Z, Nashan D, Weller RB, Castellsagué X. Skin Cancer: Epidemiology, Disease Burden, Pathophysiology, Diagnosis, and Therapeutic Approaches. Dermatol Ther (Heidelb). 2017;7(Suppl 1):5-19. DOI: http://dx.doi.org/10.1007/s13555-016-0165-y
5. Barton V, Armeson K, Hampras S, Ferris LK, Visvanathan K, Rollison D, et al. Nonmelanoma skin cancer and risk of all-cause and cancer related mortality: a systematic review. Arch Dermatol Res. 2017;309(4):243-51. DOI: http://dx.doi.org/10.1007/s00403-017-1724-5
6. Martín-Garcia E, Arias-Santiago S, Serrano-Ortega S, Buendía-Esman A. Evolución de la incidencia del cáncer de piel y labiodurante el periodo 1978-2007. Actas Dermosifiliogr. 2017;108(4):335-45.
7. Lamberg AL, Sølvsten H, Lei U, Vinding GR, Stender IM, Jemec GB, et al. The Danish Nonmelanoma Skin Cancer Dermatology Database. Clin Epidemiol. 2016;8:633-6. DOI: http://dx.doi.org/10.2147/CLEP.S99464
8. Stein JD, Antonyshyn OM. Aesthetic eyelid reconstruction. Clin Plastic Surg. 2009;36(3):379-97. DOI: http://dx.doi.org/10.1016/j.cps.2009.02.011
9. Lanoue J, Goldenberg G. Basal Cell Carcinoma: A Comprehensive Review of Existing and Emerging Nonsurgical Therapies. J Clin Aesthet Dermatol. 2016;9(5):26-36.
10. O'Halloran L, Smith H, Vinciullo C. Periocular Mohs micrographic surgery in Western Australia 2009-2012: A single centre retrospective review and proposal for practice benchmarks. Australas J Dermatol. 2016;58(2):106-10.
11. Chandler DB, Gausas RE. Lower eyelid reconstruction. Otolaryngol Clin North Am. 2005;38(5):1033-42. PMID: 16214572 DOI: http://dx.doi.org/10.1016/j.otc.2005.03.006
12. Rafii AA, Enepekides DJ. Upper and lower eyelid reconstruction: the year in review. Curr Opin Otolaryngol Head Neck Surg. 2006;14(4):227-33. DOI: http://dx.doi.org/10.1097/01.moo.0000233592.76552.d2
13. Elabjer BK, Petrinovic-Doresic J, Busic M, Elabjer E, Kastelan S. Retrospective analysis of reconstruction techniques after periocular basalioma Excision. Coll Antropol. 2007;31 Suppl 1:91-6.
14. Mustardé JC. The use of flaps in the orbital region. Plast Reconstr Surg. 1970;45(2):146-50. PMID: 5411895 DOI: http://dx.doi.org/10.1097/00006534-197002000-00007
15. McGregor IA. Eyelid reconstruction following subtotal resection of upper or lower lid. Br J Plast Surg. 1973;26(4):346-54. PMID: 4586380 DOI: http://dx.doi.org/10.1016/S0007-1226(73)90038-6
16. Matsuo K, Hirose T, Takahashi N, Iwasawa M, Satoh R. Lower eyelid reconstruction with a conchal cartilage graft. Plast Reconstr Surg. 1987;80(4):547-52. DOI: http://dx.doi.org/10.1097/00006534-198710000-00012
17. Almeida ACM, Silva Filho AF, Alves JCRR, Silva RLF. Cirurgia micrográfica no tratamento do carcinoma microcístico anexial. Rev Bras Cir Plást. 2016;31(3):428-32.
18. Echchaoui A, Benyachou M, Houssa A, Kajout M, Oufkir AA, Hajji C, et al. Prise en charge des carcinomes des paupières: étude bicentrique rétrospective sur 64 cas avec revue de littérature. J Fr Ophtalmol. 2016;39(2):187-94. DOI: http://dx.doi.org/10.1016/j.jfo.2015.05.011
19. Özkaya Mutlu Ö, Egemen O, Dilber A, Üsçetin I. Aesthetic Unit-Based Reconstruction of Periorbital Defects. J Craniofac Surg. 2016;27(2):429-32. DOI: http://dx.doi.org/10.1097/SCS.0000000000002359
20. Broadbent T, Bingham B, Mawn LA. Socioeconomic and Ethnic Disparities in Periocular Cutaneous Malignancies. Semin Ophthalmol. 2016;31(4):317-24. DOI: http://dx.doi.org/10.3109/08820538.2016.1154172
21. Walker E, Mann M, Honda K, Vidimos A, Schluchter MD, Straight B, et al. Rapid visualization of nonmelanoma skin cancer. J Am Acad Dermatol. 2016;76(2):209-216.e9. PMID: 27876303
22. Cortés-Peralta EC, Garza-Rodríguez V, Vázquez-Martínez OT, Gutiérrez-Villarreal IM, Ocampo-Candiani J. Cirugía micrográfica de Mohs: 27 años de experiencia en el Noreste de México. Cir Cir. 2016;85(4):279-83.
23. Almeida ACM, Alves JCRR, Portugal EH, Araujo IC, Fonseca RPL, Andrade Filho JS, et al. Reconstrução em cirurgia micrográfica. Rev Bras Cir Plást. 2015;30(2):235-41.
24. Verity DH, Collin JR. Eyelid reconstruction: the state of the art. Curr Opin Otolaryngol Head Neck Surg. 2004;12(4):344-8. DOI: http://dx.doi.org/10.1097/01.moo.0000130577.04818.1c
25. Murillo WL, Fernandez W, Caycedo DJ, Dupin CL, Black ES. Cheek and inferior eyelid reconstruction after skin cancer ablation. Clin Plastic Surg. 2004;31(1):49-67. DOI: http://dx.doi.org/10.1016/S0094-1298(03)00122-6
26. Chedid R, Santos P, Borges KS, Farias TP, Sbalchiero JC, Dibe M, et al. Reconstrução palpebral inferior no Instituto Nacional do Câncer: estudo de 137 casos. Rev Bras Cir Cabeça Pescoço. 2010;39(4):277-82.
27. Tomassini GM, Ricci AL, Covarelli P, Cencetti F, Ansidei V, Rulli A, et al. Surgical solutions for the reconstruction of the lower eyelid: canthotomy and lateral cantholisis for full-thickness reconstruction of the lower eyelid. In vivo. 2013;27(1):141-5.
28. Mukundan PK, Ambookan PV, Dilliraj VK. Soft tissue defects of eyelid and malar region: an experience with the McGregor flap. Plast Aesthet Res. 2015;2(2):69-72. DOI: http://dx.doi.org/10.4103/2347-9264.153202
29. Uemura T, Yanai T, Yasuta M, Kawano H, Ishihara Y, Kikuchi M. Switch Flap for Upper Eyelid Reconstruction-How Soon Should the Flap Be Divided? Plast Reconstr Surg Glob Open. 2016;4(4):e695. DOI: http://dx.doi.org/10.1097/GOX.0000000000000670
1. Hospital Felício Rocho, Belo Horizonte, MG,
Brazil.
2. Instituto de Cirurgia Plástica Avançada, Belo
Horizonte, MG, Brazil.
3. Hospital e Maternidade Therezinha de Jesus,
Juiz de Fora, MG, Brazil.
4. Hospital Monte Sinai, Juiz de Fora, MG,
Brazil.
5. Sociedade Brasileira de Cirurgia Plástica, São
Paulo, SP, Brazil.
6. Universidade Federal de Minas Gerais, Belo
Horizonte, MG, Brazil.
7. Faculdade de Medicina, Universidade de Itaúna,
Itaúna, MG, Brazil.
Corresponding author: Augusto César de Melo
Almeida
Rua Erê, 23, Sala 1205 - Prado
Belo Horizonte, MG, Brazil
Zip Code 30411-052
E-mail: contato@draugustoalmeida.com.br
Article received: August 06, 2017.
Article accepted: May 17, 2018.
Conflicts of interest: none.








 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter