

Articles - Year 1999 - Volume 14 -
Silicon Palpebral Suspensory Implant for Severe Blepharoptosis Correction
Implante Suspensor Palpebral de Silicone para Correção da Blefaroptose Severa
ABSTRACT
Patients with severe palpebral ptosis and poor suspensory muscle action often benefit from the frontal suspensory method using organic or inorganic material. Studies are known in literature using homologous sclera, dura mater homologous and autologous fascia lata, surgical silk, supramid, goretex, mersilene mesh, prolene, among others. In cases where changes exist that prevent a good eye protection, such as in pair III palsy, progressive chronic ophthalmoplegia, neuroparalysis keratitis, myasthenia gravis, orbital fibrosis syndrome, dry keratoconjunctivitis arpair VII paresis with ptosis, silicon strips have been used although with significant rates of recurrent ptosis in the medium and long term. In order to decrease this occurrence, a Dacron-reinforced premolded silicon palpebral suspensory was developed and used in 45 patients with severe ptosis, in a total of 58 eyelids. This paper discusses the results obtained and arrives to the conclusion that the procedure is easily carried out, offers effective and longlasting results, with the possibility of easy postoperative adjustment, if required. The availability of the sterile and ready-to-use piece facilitates the procedure. Indication to the method extended to all severe ptosis cases and not only to those that presented changes allowing no adequate eye protection.
Keywords: Palpebral ptosis; frontal suspensory; silicon strips
RESUMO
Pacientes com ptose palpebral severa e ação fraca do músculo elevador habitualmente são beneficiados com o método da suspensão frontal utilizando-se materiais orgânicos ou inorgânicos. Na literatura, são conhecidos estudos com esclera homóloga, dura mater, fáscia lata homóloga e autóloga, fio de seda, supramid, goretex, tela de mersilene, prolene, dentre outros.
Nos casos em que existam alterações que impeçam a boa proteção ocular, como paralisia do III par, oftalmoplegia crônica progressiva, ceratite neuroparalítica, miastenia gravis, síndrome da fibrose orbitária, ceratoconjuntivite seca ou paresia do VII par com ptose, têm sido utilizadas tiras de silicone, entretanto com índices significativos de recorrência da ptose a médio e longo prazos.
Para diminuir essa ocorrência, desenvolveu-se um suspensor palpebral pré-moldado de silicone com reforço de Dacron utilizado em 45 pacientes com ptose severa, num total de 58 pálpebras. Neste trabalho discutem-se os resultados obtidos e chega-se à conclusão de que o procedimento é de fácil execução, que oferece resultados efetivos e duradouros, com possibilidade de fácil ajuste pós-operatório, caso seja necessário. A disponibilidade da peça estéril e pronta para o uso facilita o procedimento. A indicação do método ampliou-se para todos os casos de ptose severa e não apenas para aqueles que apresentem alterações que não permitam proteção adequada ao olho.
Palavras-chave: Ptose palpebral; suspensão frontal; tiras de silicone
Upper eyelid is located in the sight primary position, 1 to 2 mm below upper scleral limbus. Palpebral ptosis is defined as a change in the upper palpebral position below usual level. It may be acquired, congenital, one or two-sided. According to Beard(ll) classification, the acquired one may occur due to myogenic, neurogenic, traumatic or mechanical cause and the congenital one due to elevator muscle dystrophy, not associated to other neurological anomalies. Patients bearing congenital ptosis, however, may present other changes such as: upper straight muscle weakness, cross-eye, Marcus Gunn phenomenon or blepharophimosis syndrome. Ptosis degree is mild if equal to or lower than 2 mm, moderate if up to 3 mm and severe if equal to or higher than 4 mm. Elevator muscle function is measured by upper eyelid excursion when performing supra and infraversion with digital blocking of frontal muscle. It is considered good when presenting 11 mm or more, moderate from 5 to 10 mm and weak: when equal to or lower than 4 mm.
Careful analysis of ptosis degree, elevator muscle function and deformity etiology will determine the best surgical choice for the case.
Patients with severe palpebral ptosis (equal to or higher than 4 mm) in which the eyelid elevator muscle function is weak: (4 mm excursion or less) benefit from only frontal suspensory methods. In such cases no good results are achieved with a more physiologic technique such as the elevator muscle aponeurosis shortening.
Several organic and inorganic materials were proposed to connect tarsi to frontal musculature that, when contracted, is able to lift upper eyelid. There are studies in literature on the use of homologous(1) sclera, dura mater(1,2), homologous and autologous fascia lata(2,3,7),fascia temporalis(2), surgical silk(4,5), supramid(6), goretex(1), mersilene mesh(1,2,9), prolene(8), among others.
Fascia lata has been widely used as material of choice to frontal suspensory. Nevertheless, in the event reoperation is required to correct hypo or hypercorrection of ptosis in the medium and long term, the procedure becomes difficult due to cicatricial fibrosis encompassing fascia lata. In addition, when changes exist such as third pair palsy, progressive chronic ophthalmoplegia, neuroparalytic keratitis, myastenia gravis, orbital fibrosis syndrome, dry keratoconjunctivitis or seventh pair paresia with ptosis, that prevent eye protection, the use of fascia lata may predispose to corneal exposure. In these cases, silicon strip(s) has been used(13,16).
Synthetic material offers the advantage of not presenting absorption by organism; but they may, however, lead to foreign body granuloma formation, infection and extrusion.
Tillet and Tillet(10) described frontal suspensory with silicone strips in 1966 and since then various surgical approaches have been used with respect to their disposal (2,12,13,14,15,16).
Silicon is a easily obtained and handled material but, when used only as strip(s), it causes a significant rate of ptosis recurrence in the medium and long term(10).
With the aim at diminishing this problem, this paper proposes the use of a premolded silicon palpebral suspensory with a characteristic format to adapt to palpebral and frontal regions. Thus, the procedure is exceedingly simplified and provides effective and long-lasting results.
METHOD
Forty-five patients with severe palpebral ptosis were operated from 1989 to 1997 at Hospital das Clínicas of University of São Paulo School of Medicine and at private clinic.
From these 45 patients, 58 up per eyelids were operated, 32 being one-sided and 13 two-sided. Twenty-eight patients were male and 17 female, with ages ranging from 2 to 70 years old, average 14.7 years.
All treated subjects had congenital palpebral ptosis.
A premolded soft silicon elastomer device, named palpebral suspensory was developed. It contains two 1 mm diameter by 70 mm length cables, side connected to a Dacron-reinforced silicon lamina, measuring 13 mm by 3.5 mm, presenting three 1-mm diameter holes (Fig. 1).
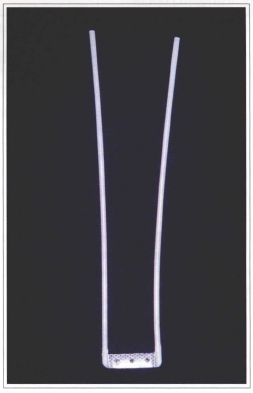
Fig. 1 - Palpebral suspensory implant.
Patients were operated under local anesthesia with vasoconstrictor and sedation or general anesthesia.
SURGICAL TECHNIQUE
Lower and upper palpebral furrow and two segments over eyebrow are demarcated at 10 mm extension located at side and median third level, respectively, such as to form a trapezoid figure (Fig. 2).
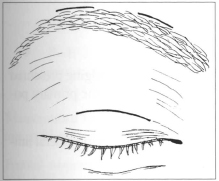
Fig.2 - Demarcation of cutaneous incisions.
Incisions reached eyebrow periosteal plane and eyelid tarsal plane. From the palpebral incision, a 15 mm width by 5 mm height area sufficient to contain silicon lamina is dissected over tarsi. This is adapted and secured to tarsal plate by means of five 5-0 monofilamented nylon stitches with 1 cm cylindrical needle, with 3 stitches comprising the lamina holes and the other 2 comprising the sites were cables are tied to it.
Under blunt dissection, 2 tunnels under orbicular muscle are made in the direction of eyebrow incisions toward tarsi and transposing medial and side silicon cables toward eyebrow (Fig. 7b).
Frontal muscle is identified through eyebrow medial incision and 5-0 monofilamented nylon stitch is taken comprising frontal muscle portion such as to simulate a pulley through which medial cable passes. This goes toward side incision, through tunnel under frontal muscle (Fig. 3).
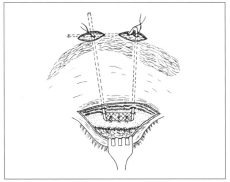
Fig. 3 - Positioning of suspensory implant after tarsal fixation.
Once outward to side incision, cables are fixed among themselves and to frontal muscle by 5-0 monofilamented nylon stitch. This stitch, however, is not completed till palpebral edging is positioned at upper scleral limbus, by cranial traction of silicon cables. Surplus is sectioned, keeping 10 mm only from the said stitch, that are introduced under frontal musculature (Figs. 3 and 4).
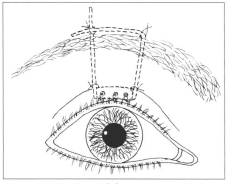
Fig. 4 - Fixation of frontal muscle cables with upper eyelid tangent to scleral limbus.
Palpebral furrow is restored through three 6-0 monofilamented nylon stitches, comprising the lamina 3 holes, the orbicular muscle and dermis, in separate stitches (Fig. 5).
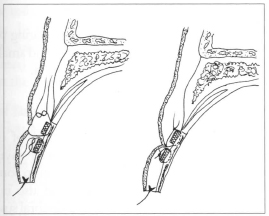
Fig. 5 - Making of upper palpebral furrow.
Cornea is protected with methylcellulose ointment and Frost suture for 24-48 hours (Fig. 6).
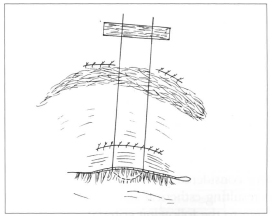
Fig. 6 - Palpebral occlusion with Frost stitch.
Stitches are drawn after 5 to 7 days. Postoperative care is the usual one for blepharoplasty.
In such cases where reoperation is required, incision is made at eyebrow side cicatrix only and two silicon cables are identified to be released to palpebral edging reposition.
Results were considered good, regular and bad according to resulting esthetical and functional aspect, and according to the following criteria:
GOOD:
REGULAR:
BAD:
RESULTS
The 45 cases operated were studied from 1989 to 1997 with 12 to 96 month follow-up.
Results were considered regular when patient presented a good side and another regular one, and good when both sides were good.
According to Table I, the following results were achieved:
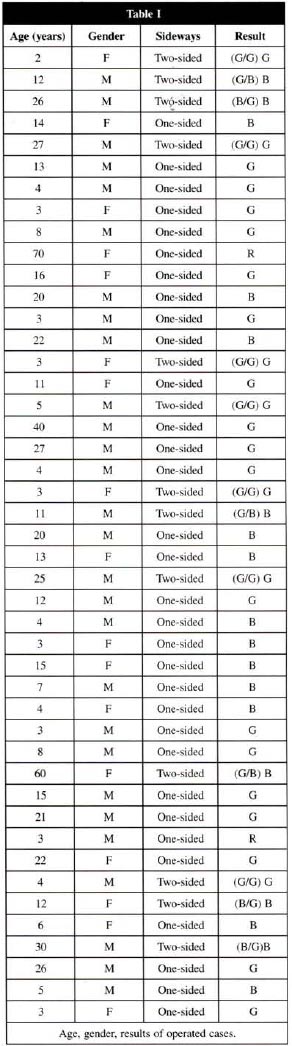
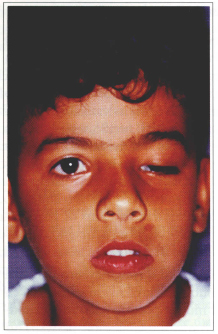
Fig. 7a - Left one-sided severe ptosis.
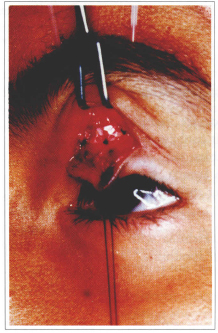
Fig. 7b - Transoperative showing implant tarsal fixation.
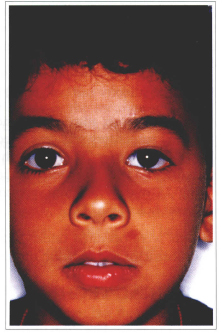
Fig. 7c - 1 year postoperative.

Fig. 8a - Right one-sided severe ptosis.

Fig. 8b - 2 year postoperative.
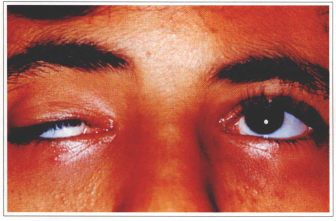
Fig. 8c - Preoperative in supraversion.
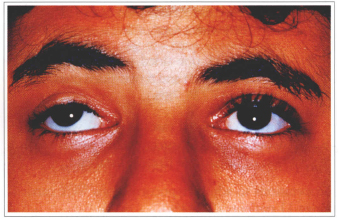
Fig. 8d - Postoperative in supraversion.
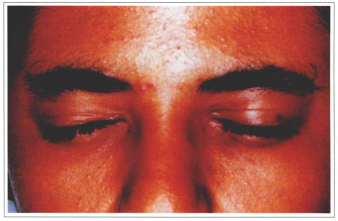
Fig. 8e - Postoperative in occlusion.
Reoperations to adjust hypocorrections were carried out in 11 patients (24.44%).
Frontal suspension method using silicon premolded palpebral suspensory provided 95.56% of good and regular results and 4.44% of bad results.
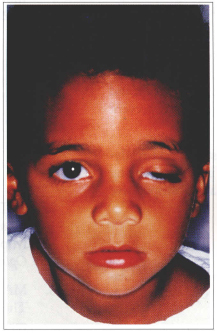
Fig. 9a - Left one-sided severe ptosis.
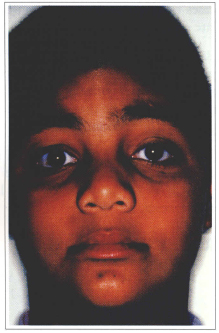
Fig. 9b - 8 year postoperative.
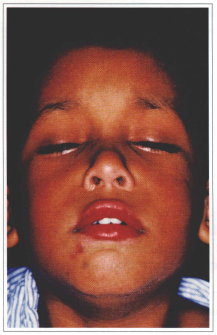
Fig. 10a - Two-sided severe ptosis.
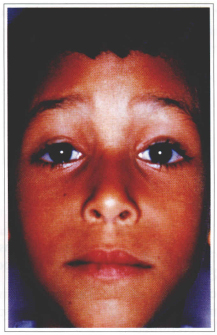
Fig. 10b - 6 year postoperative.
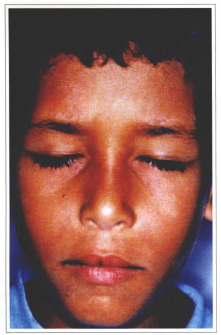
Fig. 10c - Postoperative in occlusion.
DISCUSSION
Non-absorbent threads in general provoke foreign body-type inflammatory reactions, frequently causing extrusions. In theses situations, drawing of threads after a few weeks is indicated; since, however, elevation attained will only depend on fibrosis amount formed in the site, it is, thus, irreversible.
The use of fascia lata does not provoke foreign bodytype reaction as it is an autogenous material. However, a more prolonged surgical time is required to get it, besides causing a scar at donor thigh side face. If by chance reoperation is required due to improper or even overdone correction, fascia lata cannot be identified in the medium and long term since it is embodied by intense fibrosis.
Other materials were proposed(1,2) for palpebral suspension, but all of them presented disadvantages for employment such as infection and extrusion.
With the advent of silicon, surgeons expectations may be met as the technique is simple, operative time is faster and material is well tolerated by organism.
In addition, it would facilitate orbicular muscle action in the palpebral occlusion for presenting a certain elasticity(10).
When first described, silicone had a tubular strip form that provided a slight fixation to tarsi and could cause deinsertion in the early postoperative. Also, depending on the extension to which such strip was fixed, if exiguous, caused palpebral edging groove distortion. Taking into consideration silicon physicochemical advantages and having in view the small inconveniences mentioned, we developed the premolded palpebral suspensory.
This device is made on soft silicon elastomer with Dacron-reinforced horizontal lamina in order to achieve more resistance. The three equidistant holes along the lamina provide the passage of monofilamented nylon threads that harmonically and symmetrically secure it to the tarsal plate. The formed capsule involving the whole suspensory and specially the horizontal lamina helps to maintain late stable results.
One-sided ptosis cases may present a better esthetic result mainly with satisfactory symmetry; if palpebral suspension is performed in both eyelids and if sound side normal elevator muscle is weakened so to achieve full dependence of frontal muscle contraction. Many parents and patients, however, refuse to accept such procedure.
General or local anesthesia depend on patient cooperation. Even when general anesthesia is chosen, 0.5% bupivacaine solution with epinephrine (1:200.000) is infiltrated aiming at minimizing bleeding and prolonging postoperative analgesia. We prefer local anesthesia when patient cooperates, facilitating a better achievement of palpebral positioning. Pathway at palpebral furrow aims at easily reaching tarsal plate as well as disguising scar.
When dissecting palpebral region, tarsal plane on which horizontal lamina is fixed with non-absorbent thread should be reached. At this step it is important to transfix stitches at palpebral conjunctive.
Suspensory must form trapezoid figure in order not to provoke eyelid-edging groove. Pulley made comprising underlying musculature provides easy adjustment in case of reoperation. Maintenance of 10 mm excess of side and medial cables after fixation to frontal muscle aims at allowing adjustments, if required, in cases of hypo or hypercorrection.
Palpebral occlusion difficulty is common to occur with any frontal suspension method. This regresses after a few weeks, but exposure keratopathy is avoided during this period by artificial tear instillation along the day and use of ophthalmic ointment at night.
From the 45 patients assessed, only 2 evolved with complications due to cutaneous ulceration at pretarsal level. This was observed in initial cases where palpebral suspensory presented sharp edgings at horizontal lamina ends. After detecting the problem source, the piece was improved with the edges rounding off. Implant was drawn in these 2 cases and put back after 6 months with the new format with no abnormalities.
Severe palpebral ptosis reparation using premolded palpebral suspensory showed to be efficient, easily performed with long-lasting and efficient results. When required, eventual adjustment of eyelid positioning is easily carried out with reoperation. This procedure shall be performed as soon as possible but there carrying it out lately brings no difficulties. In this case, fixation site of silicone cables is perfectly identified by divulsion of eyebrow side suture in early cases or even by a new incision on previous scar in late cases.
Based on the good results obtained with this method, we have used silicon palpebral suspensory in all severe ptosis cases with elevator muscle weak action and not only for those that present changes that prevent good eye protection.
The availability of the premolded sterile and readyto-use piece greatly facilitates the procedure, being versatile as to allow for early or late postoperative adjustments.
REFERENCES
1. McCARTY T et al. Plastic Surgery. 1. ed. Philadelphia : WB Saunders, 1990. T II, p.1752-1774.
2. TIEN-HSING C, JUI-YUNGY,YU-RAY C. Refined frontalis fascial sling with proper lid crease formation for blepharoptosis. Plast. Reconstr. Surg. 1997;99(1):34-40.
3. CRAWFORD JS. Repair of ptosis using frontalis muscle and fascia lata. Trans. Am. Acad. Ophthalmol. Otolaryngol. 1956;60:672-678.
4. WRIGHT WW. The use of living sutures in the treatment of ptosis. Arch. Ophthalmol. 1922;51:99-102.
5. FRIEDENENWALD JS, GUYTON JS. A simple ptosis operation: utilization of frontalis by means of a single rhomboid-shaped suture. Am. J. Ophthalmol. 1948;31,411-414.
6. KATOWITZ JA. Frontalis suspension in congenital ptosis using a polyfilament, cable-type suture. Arch. Ophthalmol. 1979;97(9):1659-1663.
7. WILSON ME, JOHNSON RW. Congenital ptosis: Long term results of treatment using lyophilized fascia lata for frontalis suspension. Ophthalmology. 1991;98:1234-1237.
8. MANNERS RM, TYERS AG, MORRIS RJ. The use of Prolene as a temporary suspensory material for brow suspension in young children. Eye. 1994;8:346-348.
9. DOWNES RN, COLLIN JRO. The Mersilene mesh sling: A new concept in ptosis surgery. Br. J. Ophthalmol. 1989;73(7):498-501.
10. TILLET CW, TILLET GM. Silicone sling in the correction of ptosis. Am. J. Ophthalmol. 1966;62(3):521-523.
11. BEARD C. Ptosis. 3. ed. St. Louis : CV Mosby Company, 1981.
12. LEONE CR Jr, RYLANDER G. A modified silicone frontalis sling for the correction of blepharoptosis. Am. Jr. Ophthalmol. 1978;85(6):802-805.
13. McCORD CD Jr, SHORE JW. Silicone rod frontalis suspension. Adv. Ophthal. Plast. Reconstr. Surg. 1982;1:213-219.
14. OLDER JJ, DUNNE PB. Silicone slings for the correction of ptosis associated with progressive external ophthalmoplegia. Ophthalmic Surg. 1984;15(5):379-381.
15. LEONE CR Jr, SHORE JW, VAN GEMERT JV. Silicone rod frontalis sling for the correction of blepharoptosis. Ophthalmic Surg.1981;12(12):881-887.
16. GOLDBERGER S, CONN H, LEMOR M. Double rhomboid silicone rod frontalis suspension. Ophthalmic Plast. Reconstr. Surg. 1991;7(1):48-53.
I - Assistant Physician for the Universidade de São Paulo, School of Medicine, Plastic Surgery Division.
II - Postgraduated in Plastic Surgery by Universidade de São Paulo, School of Medicine.
III - Head Professor of Universidade de São Paulo, School of Medicine, Plastic Surgery Division.
Address for correspondence:
Renri Friedhofer, MD
Rua Maranhão, 584 - 72/74
01240-000 - São Paulo - SP Brazil
Phone: (55 11) 825-4300
Fax: (55 11) 3666-8359
e-mail: henrifri@sti.com.br


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter