

Articles - Year 1999 - Volume 14 -
Semiology of the Abdominal Wall: its Value in Planning Abdominoplasty
Semiologia da Parede Abdominal: Seu Valor no Planejamento das Abdominoplastias
ABSTRACT
The main purpose of this paper is to determine the integrity and alterations of the abdominal wall through methodized, systematized semiology, in order to establish a direct, objective relationship with the technical and surgical tactics for each individual case. It stresses the importance of assessing the abdominal region in a regular, standardized manner within a whole-body context, offering the surgeon a clear; logical line of thinking that aims at choosing the best surgical conduct to be followed.
Keywords:
RESUMO
Este trabalho tem como objetivo principal determinar a integridade ou as alterações da parede abdominal através da semiologia metodizada e sistematizada, para estabelecer relação direta e objetiva com as técnicas e táticas cirúrgicas para cada caso individualmente. Ressalta a importância de se avaliar de modo padronizado e constante a região abdominal dentro de todo o contexto corporal, possibilitando ao cirurgião um raciocínio lógico e claro, levando-o à escolha segura da melhor conduta cirúrgica a seguir.
Palavras-chave:
The abdomen plays a leading role in the anatomical image of the human body, and is of outstanding importance in defining the body contour and the aesthetic standard of the individual.
The form of the abdominal wall is given by the skeletal structure, as well as the quantity and distribution of fat, the appearance and condition of the skin, the integrity of the aponeurotic and muscular system, and the intra-abdominal organs. Each of these components constitutes an independent variable within the diagnosis of deformity of the abdominal wall which will determine the type of treatment indicated for the patient.
Sheldon(1) classifies the human form in terms of somatotypes: mesomorphic, ectomorphic and endormophic, represeming different body types. Mesomorphic individuals have a squarish appearance with heavy muscle, bone and connective tissue. Ectomorphs are characterized by their length and fragility, with minimal development of muscular and fatty tissue. Endormorphs feature excessive fat, a protuberant abdomen and short limbs. There is naturally a high level of variability among the three types, and most of the populace falls into a middle range, with the ectomorphic and endomorphic extremes being rare.
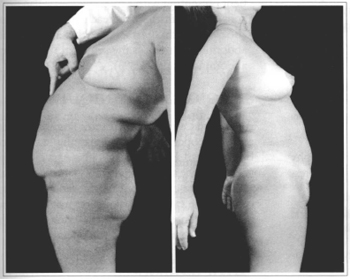
Lewis(2-5)describes three different types of abdominal wall: pendulous, globose and flaccid. The pendulous abdomen presents an accumulation of fat in the inferior abdomen and around the umbilicus, with the skin folding back over the pubis due to excess weight (Figs. 1a - 1c). The globose abdomen is rounded with generalized distention and a variable quantity of fat, with or without flaccidity of the aponeurosis and muscle system (Figs. 2a - 2c). The flaccid abdomen features surplus skin that is loose and flabby, often with stretch marks or striae (Figs. 3a - 3c).
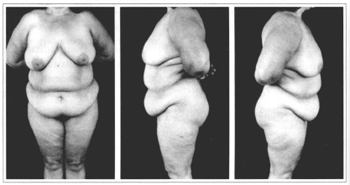
Figs. 1a-1c - Pendulous Abdomen.
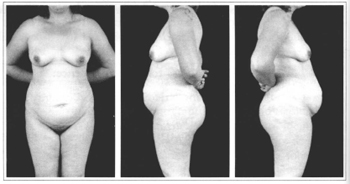
Figs. 2a-2c - Globose Abdomen.

Figs. 3a-3c - Flaccid Abdomen.
Pitanguy(6) divides abdominal deformities into two categories: aesthetic and functional alteration. Aesthetic defects are those that modify the outline of the body, due mainly to the flaccidity of the abdominal wall, accumulation of fat, and weakening of the aponeurosis and muscle system. Defects such as hernias adversely affect the functional aspect of the abdominal wall, which is no longer able to contain the viscera within the cavity. Dehiscences from sutures may occur during the initial phases of tissue healing (postoperative days 1-21) due to bruising, infections or inadequate production of collagen tissue, increase in intracavity pressure resulting in a rupture of the line of the incision, and spreading of the wound, leading to the appearance of an incisional hernia. These dehiscences may also appear later, even after the first month postoperative, for the same reasons. However, those linked to a loss of resistance in the scar are more common, due to a sudden, acute increase in intracavity pressure caused by improper strains during the postoperative period. Other after effects such as unesthetic scars due to improper positioning of incisions or infections may confer an unpleasant, deformed appearance on the abdomen. Finally, possible lesions of peripheral nerves may cause atrophy of muscle groups, resulting in weakened areas of the abdominal wall(6).
Abdominal plastic surgery is intended to correct alterations of the abdominal wall, ranging from those that affect the integument (skin and loose subcutaneous cellular tissue) to those affecting the aponeurosis and muscle structure. The goal of surgery is to achieve standards compatible with what is considered as normal for body contours(7-11).
These alterations may be summed up as: cutaneous (redundancies, stretch marks, scars, flaccidity and retractions); loose subcutaneous tissue (lipodystrophy); and those affecting the musculo-aponeurotic system (diastasis, hernia, eventration and convexity).
Based on a meticulous serniological assessment, the physical examination is vital for gathering all important data that can help establish a didactic, easily-understood classification(5,6,12-14). This classification results in the highly accurate selection of the most appropriate surgical procedure to be adopted for each case, ensuring treatment with better aesthetic and functional results. This is the scope of this work: to establish a reliable relationship between a methodized, systematized and standardized semiology, adapting the data found to the classification proposed by Professor Ivo Pitanguy, in order to indicate the best surgical procedure for the correction of alterations of the abdomen in a specific and global manner.
ANATOMY
GENERAL REMARKS
The anterior abdominal wall consists of skin, loose subcutaneous connective tissue (subcutaneous layer) and an aponeurotic-fascial-muscular system. Through the removal and/or replacement of these structures, the plastic surgeon attempts to sculpt the trunk. Consequently, knowledge of the anatomy of the anterior abdominal wall is of the utmost importance.
The anterior abdominal wall is a diamond-shaped polygonal area limited on the top by the xiphoid appendix and the edges of the rib-cage, on the side by the obligue muscles and the iliac crest, and below by the external inguinal ligaments(5).
The ectoscopy shows various "hills and valleys" representing areas of shadow and reflection of light which together offer a harmonious aspect to the abdominal contour, conferring the appearance of beauty on this aesthetic unit(6).
The natural protuberances are produced by the edges of the rib-cage, the rectus abdominis muscles, the iliac crests, the pubis and part of the suprapubic region. The "valleys" are represented by the supraumbilical mid-line, the umbilicus, the small infraumbilical mid-area, the iliac fossae, the semilunar arcades (insertion areas of the rectus and obligue muscles) and the supraumbilical transverse insertions of the rectus muscles(5,12,15,16).
The circumferential strip between the base of the thorax and the apex of the pelvic region (iliac crests) is known as the waist, and is of the utmost importance in the configuration of the silhouette of the human body, particularly among women. Its height varies by biotype (normolinear, brevilinear, longilinear). This means that it is the skeleton that determines the outline of the body with more or less "waist", according to the biotype. Consequently, a longilinear biotype favors a better-defined waist, as it allows a long, gentle line with a bilateral concavity, resulting in a slimmer silhouette. The width of the pelvis also contributes to harmony of shape in this region, as the female pelvis is broader in relation to the thorax.
The link between the fetus and the mother takes place through the umbilicus. After birth, the umbilicus represents a secondary scar. Over the past few years, the umbilicus has taken on increasing importance from the aesthetic, social and sexual viewpoints. Fashion has emphasized it to an increasing extent, exposing it with the utmost naturalness. Old-fashioned incisions of the abdominal wall even permitted its extirpation. Current techniques continue to conserve and respect it, and may even attempt to improve its appearance(17-21).
The umbilicus seems to be the only scar on the body that people make a point of retaining, complaining when it is not present or eliminated. Its absence produces severe dysmorphia, and may even undermine the body image, with psychological implications that should not be ignored.
The histological study of the umbilicus zone in the abdominal wall proves the absence of permeable vessels that could nourish the umbilical area, or neighboring zones in the abdominal wall, in addition to the corresponding fibrous ring(16).This nutrition is guaranteed by minor vessels, or by absorption through peritoneal structures, allowing the preservation of the umbilical scar even in cases where it is "skeletized", such as surgery involving the myocutaneous flap of the rectus abdominis muscle. In this condition, the umbilical pedicule is literally peeled away, held only by its base to the posterior aponeurosis, and coated internally by the peritoneal layer.
The umbilical scar is rounded in shape, depressed and more profound in its superior part. Its outer and superior parts are limited by the cutaneous ring. This is why its edges are raised, with the inferior edge being flatter, forming a gentle transition to the skin of the abdominal wall. At the bottom of the cavity in the mid-zone is a raised portion (nipple or mammila), whose center corresponds to the scar of the umbilical cord. Around this nipple is a circular depression called the umbilical groove separating the mammilla from the cutaneous ring(5,20,22,23) (Fig.4).
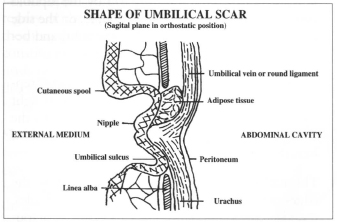
Fig. 4 - Shape of umbilical scar.
The umbilical scar allows the demarcation of the abdomen into two segments: the superior and inferior abdomen. Both are accentuated by the depression caused by the umbilical zone, and in most young women the inferior abdomen is slightly more protuberant and raised.
According to Goss(22), the umbilical scar is at the level of vertebras L3 and L4. Dubuo(5,24) studied the location of the umbilicus in 100 non-obese persons selected on a random basis when lying supine and concluded that in 96% of the cases this coincided with an imaginary horizontal line joining the iliac crests.
The pubic region is the inferior point of the abdominal polygon between the inguinocrural regions and Dumm's line. Known as the Mound of Venus, it is important in the harmony of the abdominal region, and it is vital that its shape, volume, pilosity and height should all be taken into account, determined by the distance between the vulvar furculum and its border with the inferior abdomen (Dumm line). This distance corresponds to an average of around six centimeters in accordance with current parameters, which is the ideal minimum distance that should be found after a classic abdominoplasty, avoiding distortion.
SKIN
The skin in the abdominal region is approximately 2-4 mm thick, containing the annexes normal to other parts of the body (hair, sweat glands and sebaceous glands). Its great elasticity allows appreciable alterations in the volume of the abdomen (pregnancy, obesity, etc).
The skin's insertion in the fascia is fragile, except in the area of the umbilical scar, where it is more strangly connected to the underlying structures, meeting the aponeurosis of the rectus muscles and the linea alba.
It is noted that the hairs are distributed in an oblique pattern converging downwards towards the mid-line, where they tend to spread longitudinally from the xifoid appendix to the pubic region.
In the pubic region, hair distribution tends to be lower and more triangular in women. In men this continues over the abdominal region as such, with more diffuse, less polygonal distribution.
The correct positioning of the flap during an abdominoplasty must avoid shifting of the midline to one side, which could cause distortions in the hair distribution, resulting in an unpleasant appearance for the abdomen.
The mid-line should correspond to exactly the projected linea alba, which divides the abdominal wall into two rigorously symmetrical halves.
LOOSE SUBCUTANEOUS
CONJUNCTIVE TISSUE
(SUBCUTANEOUS CELLULAR TISSUE)
Markman and Barton(25)describe the subcutaneous tissue of the trunk and the area near the lower limbs, confirming the data of Gray & coll.(23),with regard to the existence of one layer of superficial adipose tissue and a deeper layer. The superficial layer is divided into compartments formed by fibrous septa,in contrast to the deeper layer which is distributed at random, with little separation. Fatty deposits in man varies according to sex, age and race. The two main types of distribution of fat tissue are termed gynecoid (female) and android (male). Women tend to have a higher percentage of fatty tissue than men, typically those with an accumulation of fat in the inferior part of the trunk, hips and gluteal region. The areas where fat builds up in men are reflected in an increase in the abdominal circumference and the thorax, as well as the submental region. Changes secondary to aging are basically due to an increase in the volume of adipose tissue in the trunk. The adipose tissue in the limbs diminishes with age, being transferred to the intramuscular and intermuscular spaces.
Persons belonging to the Negro race tend to feature larger deposits of fat in the gluteal region compared to Orientals and Caucasians. This factor is magnified by a marked lombar lordosis, also noted in many of these patients(21,27).
SURFACE FASCIA (CAMPER-SCARPA FASCIA)
The superficial fascia plays an important role in maintaining the appearance of the abdomen. Its inferior portion (infraumbilical) is more clearly visible, particularly in the region of the iliac fossae, where it may appear as a true fascia, thinner than the muscle fascia. It is also present in the semilunar lines, yet less evident, as is true in the pubic area. Although it is less obvious than in other areas, this fascia may always be distinguished. It may be concluded that in areas where the skin and subcutaneous tissue slip more easily over the aponeurosis of the muscles, the surface fascia becomes more dense and is more clearly apparent. In patients that have undergone a laparotomy with a Pffannestiel incision, for instance, if the fascia is not re-sutured this may result in a superior retraction, causing a suprapubic transversal depression that may result in an undesirable appearance(12). This stresses the need to proceed with suturing by planes in a proper manner, strengthening the continuity of the fascia itself, particularly in abdominoplasties where the best possible effect is desired.
VASCULARIZATION
Two primary arterial plexi are responsible for the vascularity of the abdominal wall: a subdermic superficial system and a deep, more profound musculo-aponeurotic system. Many blood vessels form anastomotic connections between the two levels, particularly in the periumbilical region.
At the deeper layer, the superior and inferior epigastric blood vessels run longitudinally within the anterior rectus muscle, forming a capillary network in the midabdomen. In the superior abdomen the xifoid branches run parallel to the superior epigastric blood vessels. The blood vessels located in the periumbilical region basically originate in the subdermic superficial plexus. There are also branches coming from the inferior superficial epigastric arteries, as well as the circumflex iliac artery and the superior branches of the external pudenda, which help form this system(5,16,23).
Hunger(28) describes three vascular zones in the abdominal wall (Fig. 5).
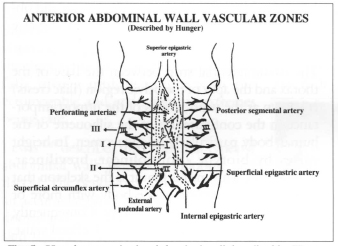
Fig. 5 - Vascular zones in the abdominal wall described by Hunger.
The venous drainage depends on the thoracoepigastric system located at the subcutaneous level, draining the axillary and femoral blood vessels, as well as the veins in the profound epigastric system.
Lymphatic drainage consists of two networks: one superficial and the other deeper, each of which drains into the axillary and inguinal lymphatic gangliar collector system (Fig. 6). The inguinal lymphatic ganglia drains all the lymphatic vessels of the lower limbs, external genitalia, perineal and gluteal regions and the zones of the abdomen and trunk below the umbilicus. They are divided into surface subinguinal lymphatic ganglia (located above the fascia) and profound (located under the fascia). The axillary lymphatic ganglia constitute the center of countless lymphatic vessels running from the arm, shoulder, chest, superior abdominal wall, and mammary glands. They are divided into superficial, brachial, chest and subscapular, and profound or infraclavicular(16,23).
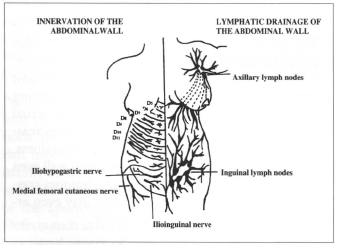
Fig. 6 - Innervation and lymphatic drainage of the abdominal wall.
Lymphatic drainage is necessarily channeled to the axillary ganglia during the immediate postoperative period after abdominoplasty, due to the section of the lymphatic channels draining the inguinal ganglia. The systems tend to repair themselves over time.
INNERVATION
The innervation of the abdominal wall includes the intercostal nerves (ie. D5-D12), as well as the major and minor abdominocrural nerves coming from L1(16,23)(Fig.6).
The distribution of nerves in the abdominal wall alters after an abdominoplasty(16,23,29). The D5 - D 12 dermatomas are moved downward in a caudal direction. Most of the inferior dermatomas (D10, D11, D12) are resectioned with the skin in a conventional abdominoplasty. The superior dermatomes are expanded after surgery so that D9 is located immediately above the incision.
APONEUROSIS & MUSCLE SYSTEM(16,23)
The abdominal wall consists of three large muscles on each side: the external oblique, the internal oblique and the transversus abdominis, which is reinforced at the mid-line by the rectus and pyramidalis muscles. These muscles are vital for maintaining posture, locomotion and intestinal functions, constituting the primary elements in establishing the tone of the abdominal wall.
PHYSIOPATHOLOGY OF ALTERATIONS IN THE ABDOMINAL WALL
Many factors may alter the form and function of the abdominal wall to the point that these alterations become unpleasant for the patient and may even cause difficulties in normal bodily hygiene. Perhaps the best way of studying these multiple factors is to consider each component in the abdominal wall separately.
SKIN
The skin of the abdominal wall may suffer alterations secondary to trauma, pregnancy, obesity, excessive weight loss or the normal aging process. These factors may produce temporary or permanent damage to the skin. The elastic nature of the abdominal wall is important from the functional view point, as in pregnancy, and this factor is an advantage that should be taken into account during abdominoplasty. However, the elasticity of the skin is not unlimited. If stretched to excess, it may result in the formation of stretch marks (striae caused by sheering and separation of collagen fibers which is replaced by scar tissue). This phenomenon may occur over the entire abdomen, being more frequent in the hypogastric region below the umbilicus. Flaccidity and skin redundancy, frequent after pregnancy, may be reversible to a certain point. Should they not be reverted within the first six months after birth, these alterations may be considered permanent.(5,6,9,12-14,30-32).
These deformities may also be caused by drastic alterations in weight, as is the case in patients with morbid obesity. On the other hand, the abdominal wall may be affected by injuries of traumatic or surgical origin, with visible secondary scars that can be treated or removed during abdominoplasty(5,6,12,30-33).
Maceration, intertrigo and dermatitis found in some patients, secondary to constant moisture and rubbing of skin folds caused by skin redundancy, is found particularly in patients with apron-like abdominal flaps.
LOOSE SUBCUTANEOUS CONJUNCTIVE TISSUE (SUBCUTANEOUS CELLULAR TISSUE)
The Brazilian Endocrinology Society and the International Endocrinology and Diabetes Society define obesity as an increase in body weight, due to excess adipose tissue, of 15 - 20% abov ethe ideal weight for men and 25 - 30% above the ideal weight for women.
There are two principal types of obesity. In hypertrophic obesity, there is a congenital increase in the capacity to store fat in the adipocytes for the same population of fat calls (ie. the cells increase in volume) compared to hyperplasic obesity, where there is production of new adipocytes to reaccommodate storage of excess lipids. This occurs when the total body fat is greater than 40 kg(5,6, 25, 27, 34).
Obesity may cause hyperlordosis with consequent stretching of the anterior rectus muscles and diastasis, added to the accumulation of fat on the abdomen. After weight loss, it is frequent to find atrophic alterations in these patients, with secondary flaccidity and skin redundancy, as well as diastasis of the previously stretched muscles(33,34).
It is worth emphasizing that in plastic surgery, in most cases obesity is a condition that normally precludes an aesthetic surgical procedure. Only under very special conditions should a "hygienic" procedure be carried out on patients with this type of metabolic and body contour alteration. In these cases, surgery is intended to remove large amounts of excessive skin and adipose tissue, with minimal undermining, in order to reduce the volume of redundant tissue, seeking to enhance patient comfort.
MUSCLES AND APONEUROSES
The muscles, fascia and aponeurosis of the abdominal wall form a type of constrictive belt that keeps the intra-abdominal organs in place and helps establish normal intestinal functions. These muscles also participate in movements of the trunk and physiological processes requiring an increase in intra-abdominal pressure(6,12-14,31,32,35,36).
Specific areas of the abdominal wall present a normal degree of weakness. These are the linea alba, the semilunar line, the umbilical ring and the inguinal region. Trauma (not necessarily surgical) and stress (situation of tissue tension such as during pregnancy or intracavity distention) may result in aponeurotic and muscular diastasis. When this occurs in the rectus abdominis muscles, it will cause an increase in globosity. When diastasis affects the external oblique muscles, this results in an increase in the circunference of the abdomen, known as the "waist" and/or herniation of the abdominal contents(5,15,16,23,37).
PATIENTS AND METHODS
In order to obtain a standardized semiological assessment for determining the integrity or alterations of the abdominal wall, a study was carried out of a group of thirty consecutive patients, not previously selected, over a period of eight months (March - November 1996) at the 38th Infirmary of the Santa Casa da Misericórdia Hospital in Rio de Janeiro, (Plastic Surgery Service of Ivo Pitanguy). A basic protocol was prepared and adopted for the entire group under study (Fig. 7).
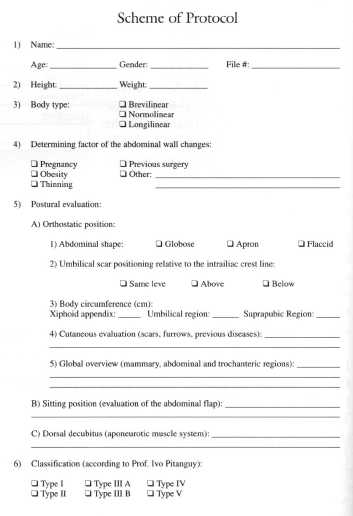
Fig. 7 - Scheme of protocol.
RESULTS
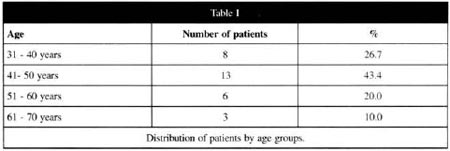
AGE
Patients' age ranged from 34 - 63 years. The fifth decade represented the largest number of patients, which is similar to the references and the literature on this topic (Table I).
SEX
All patients were women.
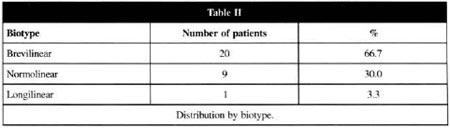
BIOTYPE
Three types of patients were identified: brevilinear, normolinear and longilinear. The brevilinear group was characterized as the morphological type classified by short limbs and large trunk; longilinear was the morphological type classified as those patients having limbs longer than the trunk, with the normolinear being intermediate in shape.
The predominant biotype was brevilinear with 20 patients (66.7%) followed by normolinear with 9 patients (30%) and longilinear with 1 patient (3.3%) Table II.
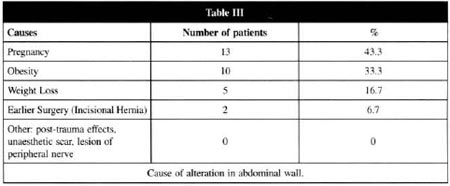
CAUSES OF ALTERATION TO ABDOMINAL WALL
Each patient was asked what had been the cause of the structural alterations in her abdominal wall: 13 patients (43.3%) related that this was caused by pregnancy, resulting in lipodystrophy of the hypogastrium, hypogastric and periumbilical stretch marks and flaccidity of the abdominal wall; 10 patients (33.3%) stated that this was dueto obesity which began in adolescence; 5 patients (16.7%) related their abdominal deformity to weight-loss causing the flaccidity of the abdominal wall and 2 patients (6.7%) had incisional hernias secondary to previous surgery. No other forms of alteration in the abdominal wall were related (Table III).
POSTURAL EVALUATION
ORTHOSTATIC POSITION
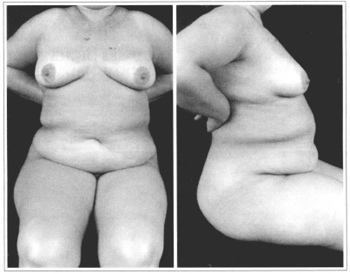
With the patient unclothed, and with her prior authorization, the authors took a front and profile view to assessthe shape of the abdominal wall, the position of the umbilical scar in relation to the interiliac crest line, comparative measurement of the circumference of the trunk, assessment of the skin and an overall view of the mammary, abdominal and trochanteric regions (Figs. 8a & 8b).
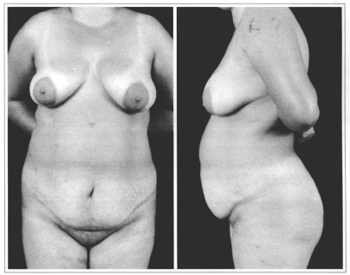
Figs. 8a & 8b - Orthostatic position, anterior view (a) and profile view (b).
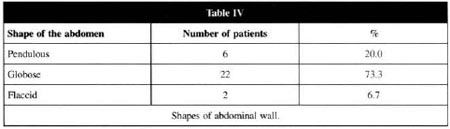
SHAPES OF THE ABDOMINAL WALL
Based on the classification of Lewis(3,4), the shape of the abdominal wall was classified into three types: pendulous, globose and flaccid. The globose form predominated, and was found in 22 patients (73.3%). This type was characterized as a rounded, protruding abdomen with generalized distention, supra and infraumbilical lipodystrophy, with or without flaccidity of the aponeurotic system. The pendulous abdomen was found in 6 patients (20.0%) and the flaccid abdomen in 2 patients (6.7%) (Table IV).
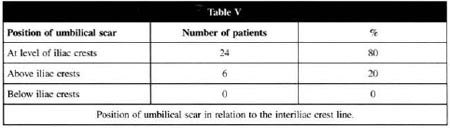
POSITION OF THE UMBILICAL SCAR IN RELATION TO INTERILIAC CREST LINE
With the iliac crests as a reference, an evaluation of the umbilical scar was made in the orthostatic position, tracing an imaginary horizontal line between the iliac crests. In 24 patients (80%) the umbilical scar was visually well positioned, coinciding with the line drawn between the iliac crests. In 6 patients (20%) the umbilical scar was more superiorly positioned (in two cases, this line ran through the inferior half of the umbilicus and in four cases it ran above the umbilical scar).
In the group studied, no case was found where the umbilical scar was below the interiliac line, even in the most severe cases of "apron-like" or pendulous abdomen. This was in contrast to what the authors expected, whereby the umbilical scar would have slipped down due to the weight of the abdominal flap (Table V).
COMPARATIVE MEASUREMENT OF BODY CIRCUMFERENCE (DORSOABDOMINAL)
Standardized measurements were taken preoperatively and during the third posroperative month. (This postoperative period was considered the smallest interval sufficient for accommodation of the flap, regression of edema, postural adjustment of patients etc). A reduction in the circumference at the level of the xifoid appendix and the umbilical region varied from 4%-8%. This was particularly related to the classic abdominoplasty and lipoaspiration of the flanks. Measurement at the suprapubic level remained stable, with no modifications noted in the sacropubic circumference. It is worthwhile recalling that even for "apron-like" abdomens, the volume caused by the redundant flap over the pubis was not included in the measurement as it does not form part of the pubic structure (Figs. 9a-9c).
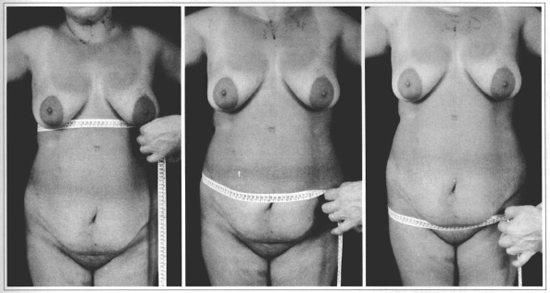
Fig. 9 - Standardized measurement of body circumference (dorsoabdominal) in the abdominal region with measuring tape. Xiphoid appendix level (a), umbilical level (b) and pubic level (c).
EVALUATION OF THE SKIN
The assessment of the condition of the skin in the abdominal region showed stretch marks in most patients, located especially in the periumbilical and hypogastric region (29 patients), unesthetic secondary scars due to surgical procedures such as laparotomy, colectomy and appendectomy in 6 patients. In 4 patients with pendulous abdomen an erythematous lesion was noted, due to maceration caused by skin rubbing (intertrigo) which responded well to topical treatment with anti-inflammatory and bactericide creams during the preoperative phase.
OVERALL VIEW OF THE MAMMARY, ABDOMINAL AND TROCHANTERIC REGION
This evaluation was intended to check the relationship between the abdomen, the breasts and the trochanteric region, allowing the authors to decide on whether or not an associated surgical procedure was necessary in order to ensure better harmonization of the body as a whole. Associated procedures may include, for instance, lipoaspiration of the hips and flanks, reduction mammoplasty etc. Although combined procedures are not included in the routine of the 38th Infirmary, this evaluation offers the surgeon a future overview of the results and an idea of probable operations that may be required at a later time.
EVALUATION IN THE SEATED POSITION
The abdomen is divided into two segments:
1. Mesoepigastric, which extends from the xifoid appendix and edge of the rib-cage to a horizontal line at the level of the umbilical scar;
2. Mesohypogastric segment, which extends from the edge of the pubis to a horizontal line at the level of the umbilical scar.
This position allows the surgeon to observe the degree of lipodystrophy and flaccidity of the abdominal wall, with the presence of one or more skin folds, seen from both the frontal and side views (Figs. 10a & 10b). A pinching maneuver of the flap at the level of the mesoepigastric segment evaluates the degree of elasticity in this area. It is the mesoepigastric region that will provide the flap that will drape over the dissected abdominal wall after resection of the redundant tissue. Through this maneuver, the length, elasticity and adhesions to underlying structures are analyzed (Figs. 11a & 11b).
Figs. 10a & 10b - Evaluation of front (a) and profile (b) in seated position, noting the mesogastric cutaneous fold, redundancies and the Dumm line.
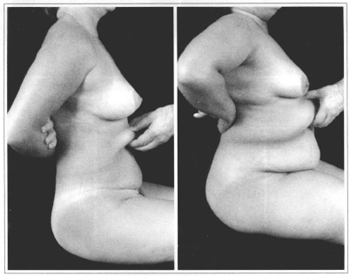
Figs. 11a & 11b - Manual pinch maneuver to assess the mesoepigastric region in two different patients.
It should be stressed that the view of the mesohypogastric region in the seated position gives an approximate estimation of the quantity of redundant tissue, and is not an accurate assessment for calculating the volume and extent of tissue to be resected of the inferior abdomen.
It is also in this position that the Dumm line can be determined. This anatomical element is vital for ensuring the ideal positioning of the final scar (Figs.10a & 10b).
EVALUATION OF THE ABDOMEN IN THE SUPINE POSITION
Valsalva maneuvers are carried out with the active participation of the patient, designed to increase intra-abdominal pressure, such as: forced bending of the thorax and forced bending of the lower limbs in extension. These maneuvers serve to evaluate the aponeurosis and the muscles, and help locate areas of weakness or fragility that may be found at the level of linea alba, umbilical region, semilunar line, inguinal regions and scarred areas (Figs. 12 & 13).
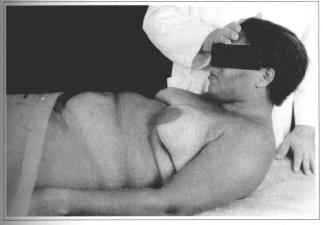
Fig. 12 - Forced bending of trunk with resistance in the frontal region.
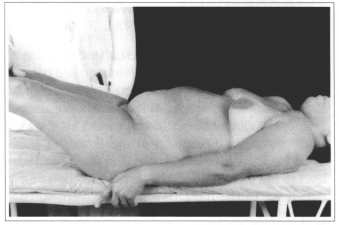
Fig. 13 - Forced bending maneuver of the lower limbs with resistance in the region of the knees.
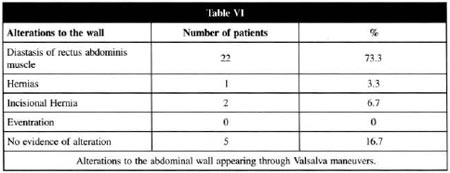
APONEUROSIS & MUSCLE SYSTEM
Diastasis of the anterior rectus abdominis muscles was clearly identifiable in 22 patients, corresponding to 73.3%. Location of this diastasis during the physical examination was supraumbilical, and was also shown in the forced extension of the thorax in an orthostatic position (Figs. 14a & 14b). In 1 patient an umbilical hernia was noted, while 2 patients presented an incisional hernia in the supra and infraumbilical midline resulting from previous laparotomies, which was easily noted during the physical examination. In 5 patients (16.7%) there was no alteration noted in the aponeurotic abdominal system during the physical examination (Table VI).
Figs. 14a & 14b - Forced extension of the thorax maneuver in orthostatic position, seeking evidence of convexity along the midline due to diastasis of the anterior abdominal muscles in two different patients.
During the operation, diastasis of the rectus abdominis muscles was corrected at both the supra and infraumbilical levels in all patients. This proved that although mesohypogastric diastasis was present during the physical examination, the degree of muscle separation could not be evaluated due to the volume of redundant mesohypogastric tissue. Typical signs of muscular diastasis, particularly the vertical convexity at the midline during the Valsalva maneuvers, may therefore be undetectable preoperatively.
ADDITIONAL EVALUATION TO THE STUDY OF THE ABDOMINAL FLAP
Lying supine, the patient is asked to bend the knees and support the feet on the bed, to ensure complete abdominal muscle relaxation. At this time the flap is pinched at the level of the mesohypogastric segment, pulling it towards the pubis. This allows an approximate evaluation of the length of the mesoepigastric flap, its elasticity and the estimated level of the incision. This maneuver also allows for the choice of the most favorable treatment to be adopted for the umbilical scar and the shape of the final periumbilical scar. Similarly, this gives a more accurate idea of the extent and volume of the mesohypogastric tissue to be removed (Fig. 15).
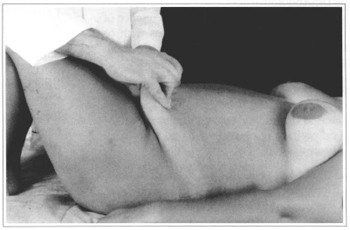
Fig. 15 - Patient lying supine with lower limbs flexed, and abdominal musculature relaxed. The tissue pinch maneuver is undertaken at the mesoepigastric level, pulled longitudinally in a caudal direction.
PITANGUY'S CLASSIFICATION OF ABDOMINAL DEFORMITIES(6)
Type I: Abdominal lipodystrophy without skin flaccidity; absence of diastasis or hernia, umbilical scar in normal anatomical position.
Type II: Infraumbilical abdominal lipodystrophy with discreet cutaneous flaccidity, presence or absence of diastasis, umbilical scar in normal anatomical position.
Type III: Generalized abdominal lipodystrophy with moderate cutaneous flaccidity, and presence or absence of diastasis.
Type IIIA: Umbilical scar in normal anatomical position.
Type IIIB: Umbilical scar in excessively high anatomical position.
Type IV: Abdominal lipodystrophy accompanied by marked cutaneous flaccidity. Presence of muscular diastasis or eventrations with or without associated scar; umbilical scar in normal anatomical position.
Type V: Marked abdominal cutaneous flaccidity with or without lipodystrophy; presence of scar at the midline ofthe abdomen. Umbilical position in normal or altered anatomical position.
Type 0: Marked generalized abdominal lipodystrophy and flaccidity. These patients are generally not considered good candidates for an aesthetic surgical procedure. Patients in this group should undergo a strict clinical treatment to lose weight, frequently needing the attention of a multidisciplinary team (eg. endocrinologist, physiotherapist, nutritionist, physiologist etc).
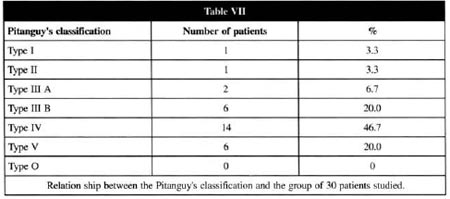
SUMMARY OF PREVALENT DATA IN SEMIOLOGICAL METHODIZATION
In this group of 30 patients, the prevalent data, meaning those with the highest percentage were: patients in the fifth decade of life (43.3%); female (100%); a brevilinear biotype (66.7%) with pregnancy as the principal determinant cause of alteration in the abdominal wall (43.3%); the globoseshaped abdomen (73.3%) with the umbilical scar at the level of the interiliac crest line (80%); patient presenting with a mesoepigastric flap that was considered sufficient to reach the line of incision (66.7%) with diastasis of the anterior rectus abdominis muscles as the principal alteration in the abdominal wall (73.3%).
SURGICAL TECHNIQUES
All patients were classified semiologically as detailed above. Preoperative surgical planning was carried out by the Head Professor (IP), the Assistant Professor (CAJ) and the accompanying resident. All surgical procedures were carried out by the senior residents, except for one case of incisional hernia, due to the volume and content of the hernial sack, where the instructor in charge handled the operation.
The surgical techniques used were:
ISOLATED SUCTION-ASSISTED LIPECTOMY (SAL) OF THE ABDOMINAL WALL(6, 29, 38, 39)
Simple lipoaspiration, or suction-assisted lipectomy (SAL) of the abdominal region was indicated for patients with Type I deformities in the Pitanguy Classification. These are mostly young patients with localized or generalized lipodystrophy of the abdomen whose skin has good elasticity and turgur with no aponeurotic and muscular flaccidity. One patient in our study underwent this procedure (3.3%).
MINI-ABDOMINOPLASTY(3,6,40-42)
This procedure was indicated for patients with weakened aponeuroses and muscles at the mid-line of the abdomen, infraumbilical lipodystrophy and moderate cutaneous flaccidity (Types II and III of the Pitanguy Classification).
Three patients (10%) underwent this procedure. Another 6 patients (20%) for which a miniabdominoplasty would theoretically have been indicated underwent a classic abdominoplasty according to the Pitanguy techniques, as this was considered a safer procedure with fewer potential complications than those related and noted in miniabdominoplasty (ie. high incidence of seromas, prologed postoperative pain and vascular embarrassment of the abdominal flap, unaesthetic scar and cutaneous redundancies). In these cases, the final scar was an inverted "T" with the vertical midline of minimal size.
CLASSIC ABDOMINOPLASTY BY THE PITANGUY TECHNIQUE(6,7,11,13,30,31,43,44)
This technique was indicated for patients with moderate or accentuated cutaneous flaccidity associated with localized or generalized lipodystrophy with or without eventrations or hernias of the abdominal wall, with Type IV, V and some Type III cases being indicated for this procedure. In these latter cases, the resulting scar may consist of a vertical component in the shape of an inverted "T". Eighteen patients (60%) in our study underwent this procedure.
ABDOMINOPLASTY ASSOCIATED WITH LIPOASPIRATION(6,7,8,10,28,30,33,38,45,46)
The association of this technique with lipoaspiration is becoming increasingly common and indicated above all for treating the flanks and hips, areas which were previously located beyond the reach of the surgeon during abdominal plastic surgery. Six patients (20%) were submitted to these associated procedures.
In no case was lipoaspiration carried out of the undermined area of the abdominal flap, due to the increase in morbidity that may result from this procedure, including lipolysis or necrosis resulting from damage to vascularization in the area treated.
ATYPICAL ABDOMINOPLASIY(6,19,30,32,36,44,47)
This was indicated for patients with a supra and infraumbilical scar at the midline, accentuated lipodystrophy, cutaneous flaccidity and incisional hernia. Two patients (6.7%) underwent this procedure, with the use of an alloplastic mesh (Marlex mesh) for reinforcement of the aponeuroses and muscles, resulting in a midline vertical xiphopubical transumbilical scar combined with a curved horizontal scar located at the level of Dumm's line, with a slightly superior concavity.
The unaesthetic aspect of the vertical midline scar precludes its use in the majority of cases, yet this would perhaps be the best way of effectively slimming the "waist" and improving the anteroposterior silhouette. In patients where this is not feasible, plication of the rectus abdominis muscles is partly effective, particularly for improving the profile, correcting the protrusion of the abdominal wall.
CONCLUSIONS
REFERENCES
1. SHELDON WH. The variety of Human Physique. New York : Hafner, 1963.
2. LEWIS JR, Jr. Atlas of Aesth. Plast. Surg. Boston : Little, Brown, 1973.
3. LEWIS JR, Jr. Miniabdominoplasty. Aesth. Plast. Surg. 1979;3:195.
4. LEWIS JR, Jr. The Art of Aesthetic Plastic Surgery. Boston : Little, Brown, 1989.
5. THEIMOURIAN BE, MAROFAT S. Cirurgia del contorno de la parte media del tronco. In: COIFFMAN, F., Cirugia Plástica Reconstructiva Estetica. Barcelona : Masson-Salvat, 1994. Vol. IV, p. 3117.
6. PITANGUY I et al. Classificação e técnicas cirúrgicas. Rev. Bras. Cir. 1995;85(1):23.
7. BAROUDI RJ, KEPPKE EM, TOZZI NETTO F. Abdominoplasty. Plast. Reconstr. Surg. 1974;54:161.
8. CASTAÑARES S, GOETHEL AJ. Abdominal lipectomy: A modification in technique. Plast. Reconstr. Surg. 1967;40:378.
9. DARDOUR JC, VILAIR R. Alternatives to the classic abdominoplasty. Plast. Reconstr. Surg. 1978;61:291.
10. HAKME F. Abdominoplasty: Peri and supra-umbilical lipectomy. Aesth. Plast. Surg. 1983;7:213.
11. JAIMOVICH CA. Sistematização em Abdominoplastias. In: Tournieux, AAB., Atualização em Cirurgia Plástica e Estética. São Paulo : Robe, 1994. p. 423.
12. BOZZOLA RJ. Abdomen. Classificación y análisys de los tratamientos cirúgicos. In: COIFFMAN F. Cirugia Plástica Reconstructiva Estetica. Barcelona : Masson-Salvat, 1994. Vol. IV, p. 3086.
13. BOZZOLA RJ. Abdominoplastias. In: MÉLEGA JM, ZANINI AS, PSILLAKIS JM. (ED). Cirurgia Plástica Reparadora e Estética. Medsi, 1988. p. 801.
14. BOZZOLA RJ, PSILLAKIS JM. Abdominoplasty: A new concept and classification for treatment. Plast. Reconstr. Surg. 1988;82:893.
15. REZENDE JM DE. Parede e cavidades abdominais. In: PORTO CC. - Semiologia Médica. 2. Ed. Rio de Janeiro : Guanabara Koogan, 1944. p. 667.
16. SPALTEHOLZ W. Atlas de Anatomia Humana, Barcelona : Labor, 1970. Vol. 2, p. 360.
17. AVELAR JM. Cicatriz umbilical: Da sua importância e da técnica de confecção nas abdominoplastias. Rev. Bras. Cir. 1979;69(1-2):41.
18. BAROUDE R. Umbillicoplasty. Clin. Plast. Surg. 1975;2:431.
19. JURI J. Reconstruction of the umbilicus in abdominoplasty. Plast. Reconstr. Surg. 1979; vol. 3, no 4.
20. MARCO AR. El ombligo. Situación e importancia. In: COIFFMAN F. Cirugia Plástica Reconstructiva y Estética, Barcelona: Masson-Salvat, 1994. Vol. IV, p. 3098.
21. WILKINSON TS, SWARTZ BE. Individual modifications in body contour surgery the "limited" abdominoplasty. Plast. Reconstr. Surg. 1986;77(5):779.
22. GOSS CM. Grays Anatomy of the Human Body. Philadelfia : Lea and Fabinger, 1965.
23. GRAY H, CLEMENTE C. Anatomy of Human Body. Philadelfia : Lea and Fabinger, 1985.
24. DUBUO RT. Chirurgie Plastique de L'Abdomen. Paris : Mason, 1971.
25. MARKMAN B, BARTON FE, Jr. Anatomy of the subcutaneous tissue of trunk and lower extremity. Plast. Reconstr. Surg. 1987;80:248.
26. BORKAN G et cols. Age changes in body composition revealed by computed tomography. J. Gerontol. 1983;38:673.
27. MARKMAN BS. Anatomic and metabolic aspects of adipose tissue. Perspect. Plast. Reconstr. Surg. 1987;1(2):258.
28. HUGER WE Jr. The anatomic rationale for abdominal lipectomy. Am. Surg. 1979;45:612.
29.COURTISS EH, MATHIAS B. Skin sensation after suction lipectomy. A prospective study of 50 consecutive patiens. Plast. Reconstr. Surg. 1988;81:550.
30. PITANGUY I. Abdominal Lipectomy: An approach to it through an analysis of 300 consecutive cases. Plast. Reconstr. Surg. 1967;40(4):384.
31. PITANGUY I. Abdominoplasty. In: Aesth. Plast. Surg. of Head and Body. Springer-Verlag, Berlim, 1981.
32. PSILLAKIS JM. Plastic surgery of the abdomen with improvement in the body contour, physiopathology and treatmente of the aponeurotic muscle. Clin. Plast. Surg. 1984;11:465.
33. ELSAHY N. Abdominoplasty combined with correction of the flabby of the lateral lower abdomen and the flanks. Aesth. Plast. Surg. 1985;9:33.
34. CLARKSON P et cols. The contribution of plastic surgery to the treatament of obesity. Mod. Trends. Plast. Surg. 1966;2:315.
35. BRUCK H. Method of reconstructing whole abdominal wall. Br. J. Plast. Surg. 1956;9:108.
36. DE PINA DP. Aesthetic abdominal deform: A personal approach to the posterior rectus sheath and rectus muscles. Plast. Reconstr. Surg. 1985;75:660.
37. RAMOS JR J. Propedêutica física do abdome. In: Semiotécnica da Observação Clínica. São Paulo : Sarvier, 1986. p. 531.
38. FOURNIER PF, OTTENI FF. Lipodissection in body sculpturing. The dry procedure. Plast. Reconstr. Surg. 1983;72:598.
39. AVELAR J. Fat suction versus abdominoplasty. Aesth. Plast. Reconstr. Surg. 1985;9:265.
40. CARDOSO DE CASTRO C, BRANCO A, CINTRA A. Limited incisions in abdominoplasty. Ann. Plast. Surg. 1987;19,5,43.
41. GRAZER FM. The miniabdominoplasty (discussion). Plast. Reconstr. Surg. 1987;79:365.
42. GREMINGER RF. The mini-abdominoplasty. Plast. Reconstr. Surg. 1987;79(3):356.
43. GRAZER MF. Abdominoplasty, in: Mc. Carty JG, Plast. Surg. Philadelphia : WB Saunders, 1990. Vol. 6, p. 3929.
44. SINDER R. Cirurgia Plástica do Abdomen. Rio de Janeiro : Ramil Sinder, 1979.
45. COURTISS EH. Our experience with combined procedures in aesthetic plastic surgery (discussion). Plast. Reconst. Surg. 1983;71:64.
46. GUERRERO-SANTOS J. Some problems and solutions in abdominoplasty. Aesth. Plast. Surg. 1980;4:227.
47. REBELLO C, FRANCO T. Abdominoplastia por Incisão Submamária. Rev. Bras. Cir.Plast. 1972; 62:244.
I - Associate Professor of the Plastic Surgery Postgraduate Course of the Pontifícia Universidade Católica do Rio de Janeiro and Carlo Chagas Postgraduate Medical Institute. Titular Member of the Brazilian Society of Plastic Surgery, of the Brazilian Academy of Militar Medicine, of the Iberian Latin-American Federation of Plastic Surgery and the Brazilian College of Surgeons. FISPRS, FICS.
II - Associate Professor of the Plastic Surgery Postgraduate Course of the Pontifícia Universidade Católica do Rio de Janeiro and Carlos Chagas Postgraduate Medical Postgraduate Medical Studies.
III - Graduate Senior Resident in Plastic Surgery, the Carlos Chagas Postgraduate Medical Studies.
IV - Head-Professor of the Plastic Surgery Postgraduate Course of the Pontifícia Universidade Católica do Rio de Janeiro and Carlo Chagas Postgraduate Medical Institute. Titular Member of the Brazilian Society of Plastic Surgery., of the National Academy of Medicine, and the Brazilian Academy of Letters. FICS, FACS.
Address for correspondence:
Centro de Estudos Ivo Pitanguy
R. Dona Mariana, 65
22280-020 - Rio de Janeiro - RJ Brazil
Phone: (55 21) 532-4455 - Fax: (55 21) 286-4991
e-mail: ceip@visualnet.com.br


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter