

Original Article - Year 2018 - Volume 33 -
Analysis of the participation of a university hospital in a national program for breast reconstruction
Análise da participação de hospital universitário em um mutirão nacional de reconstrução mamária
ABSTRACT
Introduction: Despite advances in conservative surgeries,
mastectomy is still a commonly performed procedure. However,
many patients are unable to undergo immediate reconstruction.
Such patients are integrated into a growing queue for restorative
surgery. With the intention of reducing this demand, surgical
Task Force programs were created. The objective of this study
was to analyze the results of the second National Task Force
of Breast Reconstruction (NTFBR), performed at the Plastic
Surgery Service of Walter Cantídio University Hospital (SCPMRHUWC).
Method: A prospective cohort study was conducted, in
which 16 patients underwent breast reconstruction at SCPMRHUWC.
The patients were followed up for 6 months, and their
data were tabulated and analyzed.
Results: All 16 female
patients underwent breast reconstruction after mastectomy.
The patients' ages ranged from 39 to 72 years. Among the
early complications, seroma in the dorsal region (13%), partial
necrosis of the mastectomy skin (6%), partial dehiscence of the
operative wound (13%), and necrosis of the large dorsal flap
(6%) were observed. None of the patients had late complications.
The period of hospitalization ranged from 1 to 5 days. All
patients who were in the SCPMR-HUWC queue for surgery
were operated on.
Conclusions: In this study, a high degree
of satisfaction was verified by the operated patients, and good
results were obtained with few functional complications. Thus,
we conclude that the Task Force of breast reconstruction after
mastectomy is a viable alternative in terms of public health.
Keywords: Reconstructive surgical procedures; Mastectomy; Mammaplasty; Health expenditures
RESUMO
Introdução: Mesmo com os avanços das cirurgias conservadoras, a mastectomia ainda é uma
cirurgia bastante realizada. Todavia, muitas pacientes não conseguem
submeter-se à reconstrução imediata, passando a integrar uma crescente fila
à espera da cirurgia reparadora. Com o intuito de diminuir tal demanda,
foram criados os programas de mutirão cirúrgicos. O objetivo deste trabalho
é analisar os resultados referentes ao 2º Mutirão Nacional de Reconstrução
Mamária (MNRC), realizado no Serviço de Cirurgia Plástica do Hospital
Universitário Walter Cantídio (SCPMR-HUWC).
Método: Estudo de coorte prospectiva, no qual foram avaliadas as 16 pacientes
submetidas à reconstrução mamária no 2º MNRM no SCPMR-HUWC. As pacientes
foram acompanhadas pelo período de 6 meses e os dados obtidos foram
tabelados e analisados.
Resultados: 16 pacientes, todas mulheres, foram submetidas à reconstrução mamária
pós-mastectomia. A idade variou entre 39 e 72 anos, com média de 49 anos.
Dentre as complicações precoces, foram observados seroma em região dorsal
(13%), necrose parcial da pele da mastectomia (6%), deiscência parcial da
ferida operatória (13%) necrose do retalho de grande dorsal (6%). Nenhuma
das pacientes apresentou complicações tardias. O período de internação
variou de 1 a 5 dias. Todas as pacientes que estavam na fila do SCPMR-HUWC
de cirurgia foram operadas.
Conclusões: Foi verificado alto grau de satisfação por parte das pacientes operadas e
bons resultados obtidos, com poucas repercussões funcionais. Assim,
concluímos que os mutirões de reconstrução mamária pós-mastectomia são uma
alternativa viável em termos de saúde pública.
Palavras-chave: Procedimentos cirúrgicos reconstrutivos; Mastectomia; Mamoplastia; Gastos em saúde
INTRODUCTION
Breast cancer is currently one of the most common health problems in the world. In Brazil, its incidence has been increasing gradually. Excluding skin cancer, breast cancer is the most frequent type of cancer that affects women worldwide1.
Total mastectomy, especially in some developing countries and centers further away, is still widely employed for the treatment of breast cancer. This surgery and other adjuvant therapies may contribute to the development of physical and psychological complications, which can negatively influence patients’ quality of life2-4. After mastectomy, the loss of breast alters the body image of women and yields a feeling of mutilation and loss of femininity and sensuality5,6.
In an attempt to reduce the negative feelings related to the disease and its treatment, improve self-esteem, and address the loss of breast, many women opt for surgical reconstruction7. This is a safe procedure, which does not increase the risk of recurrence, interfere with detection of the disease, or lead to delay in adjuvant therapies. There are several surgical procedures such as conservative techniques, adjacent flaps, alloplastic materials, and myocutaneous pedicle flaps microcirúrgicos8-12.
Law 12, 802/2013 requires the Unified Health System (SUS) to provide reconstructive plastic surgery of the breast soon after mastectomy when clinical conditions permit. However, there is often no structure in public hospitals to perform such procedures. Further, there are deficiencies ranging from lack of operating rooms to the absence of qualified medical personnel and suitable material. Thus, reconstruction is for the second half. However, owing to the high demand of the SUS, many of these patients are waiting for reconstruction in rows, which often seem intermináveis12.
The Brazilian Society of Plastic Surgery (SBCP) estimates that the average waiting time for reconstruction is 10 years; in 2015, only 1100 breast reconstructions were performed by the SUS12.
Many civil institutions, such as the SBCP, in partnership with the NHS, often offer solutions to mitigate these situations. Among these solutions, we can mention Mutirões12.
From October 24 to 29, 2016, the SBCP promoted the 2nd National Task Force of Breast Reconstruction (NTFBR), which included the participation of more than 800 professionals in the specialized area. Approximately 840 women who underwent mastectomy were operated on for free by plastic surgeons, aiming at the possibility of rebuilding mamária12.
The Plastic Surgery Service of Walter Cantídio University Hospital (SCPMR-HUWC) also collaborated on this project in 2016, with heterogeneous participation of plastic surgeons and completion of 16 breast reconstructions.
OBJECTIVE
The objective of this study was to analyze the results of the 2nd NTFBR, held in October 2016 in SCPMR-HUWC, with a heterogeneous group of plastic surgeons.
METHODS
A prospective cohort study was conducted, in which 16 patients who underwent breast reconstruction in SCPMR-HUWC and were included in the second NTFBR held in October 2016, were evaluated.
The study was approved by the Ethics in Research CAAE: 69439917.0.0000.5045 and was conducted in accordance with Resolution 466/12 of the National Health Council, which approved the regulatory guidelines and standards for research involving humans.
The Task Force in question included all patients who were in the queue for breast reconstruction surgery in SCPMR-HUWC. We collected the following data: age, waiting time in the queue, type of breast reconstruction performed, length of hospital stay, and postoperative complications.
The patients were followed up for 6 months; their data were tabulated and analyzed by the investigators using the statistical software Epi-Info®, and were considered significant at p < 0.05 with a confidence interval of 95%.
RESULTS
A total of 16 female patients were subjected to post-mastectomy breast reconstruction and cardiovascular and surgical risk evaluations; all patients were found to be fit for reconstruction.
No patient was under treatment with chemotherapy (QMT) or radiotherapy (RTX). All patients were to undergo delayed reconstruction (more than 1 year after mastectomy and free from any adjuvant procedure like QMT and RTX for more than a year).
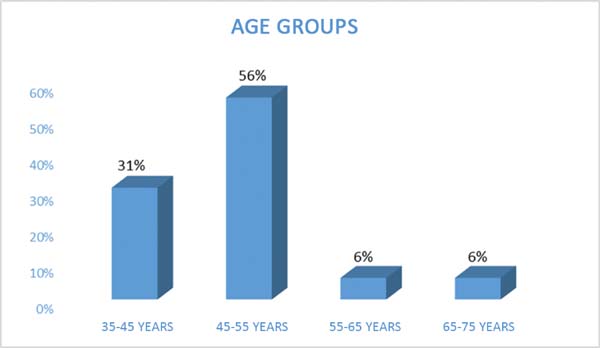
The patients’ ages ranged from 39 to 72 years, mean 49 years for the reconstruction (Figure 1).
None of the patients presented with skin disorders, radiodermatitis, pyoderma, tumors, or significant deformities in the surgical site.
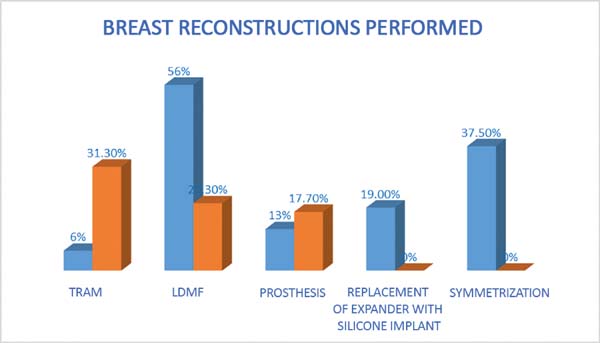
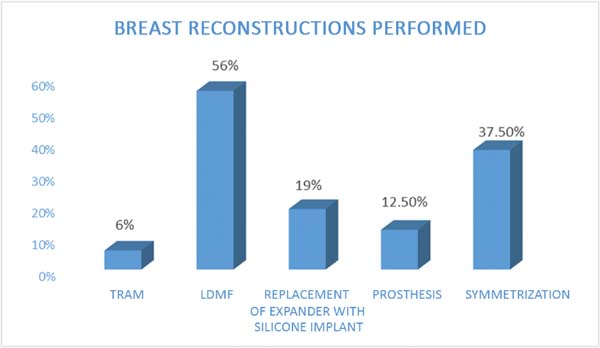
The following types of reconstruction were performed: one (6%) rectus muscle myocutaneous flap (TRAM) creation, nine (56%) latissimus dorsi muscle myocutaneous flap (RGD) creations, five prosthesis [three (19%) with exchange with unilateral prosthesis expanders and two (12.5%) with unilateral prosthesis (right)] implantations, and six (37.5%) symmetrizations (Figures 2 to 6).
The length of hospital stay ranged from 1 to 5 days; approximately 82% of the patients passed 4 days or less.
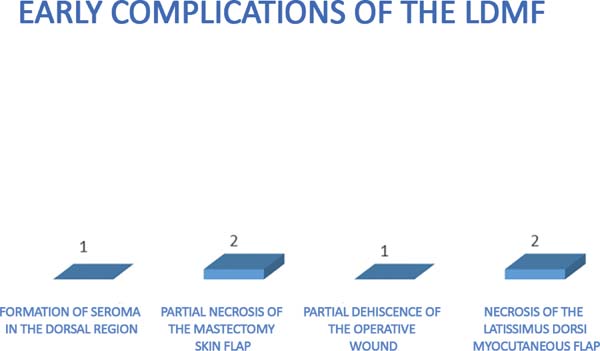
The complications were divided into early (those that occurred within 30 days after surgery) and late (those that occurred after 30 days). The earliest complications observed were seroma in the dorsal region (13%), partial necrosis of the mastectomy skin (6%), dehiscence of the operative wound (13%), and necrosis of the latissimus dorsi flap (6%) (Figures 7 and 8).
None of the risk factors (i.e., hypertension, diabetes mellitus, smoking, BMI, and age) was significantly associated with the early complications. All early complications occurred only in the patients with RGDs.
None of the 16 patients had any late complications such as implant coverage changes, capsular contraction, or muscle and skin atrophies.
DISCUSSION
Breast reconstruction is gaining an increasingly important role in the treatment of breast cancer because of the proven psychological and physical benefits for patients. This procedure favors faster return of these patients to social life, improves immunity, and thus offers better prognosis in the treatment of the disease13,14.
Many reconstruction techniques have been developed over the years. The most commonly used procedures are as follows:
Creation of myocutaneous pedicle flaps, such as latissimus dorsi muscle flaps;
Creation of retail transverse rectus abdominis muscle flaps;
Implantation of alloplastic materials, such as temporary or permanent tissue expanders;
Implantation of silicone.
In this scenario, there is evidence of indications of breast reconstruction with the use of local flaps, and the alloplastic materials RGD over the TRAM, which has a higher morbidity and systemic site15.
In the study by Cosac et al.16, the most used technique was TRAM reconstruction (31.3%), followed by RGD (30%), and prosthesis (17.7%). However, reconstruction using exchange expander prosthesis and symmetrization were not studied. In our study, the type of reconstruction performed constituted TRAM (6%), RGD (56%), 13% and symmetrization prosthesis (37.5%) (Figure 9).
For the treatment for breast cancer, adjuvant radiation therapy is often performed after mastectomy in women diagnosed with breast cancer stages II and III. This increases local control, disease-free survival, and survival globally17-20.
Despite the improvement of the oncological results, adjuvant radiation therapy in women with breast cancer may worsen the aesthetic results due to tissue atrophies and capsular contractures and increase the risk of loss of rebuilding mamária21.
Seroma in the donor area of the latissimus dorsi muscle is the most common complication of the procedure, with a reported rate of 16% to 79%22-25.
However, the significance of seroma as a major complication requiring further surgery is low. In the present study, we observed a rate of 13% seroma. Gart et al.15 reported that 1079 patients from the database of American College of Surgeons National Surgical Improvement Program (ACS-NSQIP) undergoing RGD, showed early complications like reoperations (5.7%), cutaneous infections (3.3%), necrosis (1.3%), surgical wound dehiscence (0.6% ), and other complications (3.2%) 26.
Early complications were observed in this joint Task Force of the case 1 (6%) partial mastectomy skin necrosis and 2 cases (13%) partial dehiscence of the surgical wound. These complications occurred probably due to the ineffective surgical procedure resulting in patchwork, thin mastectomy, and hypoperfused skin. There was 1 case of necrosis of the flap of latissimus dorsi, but no cases of infection or other clinical complications.
In a case series of 100 cases, Perdikis et al.22 observed a capsular contracture rate of in patients undergoing RGD and 6% in those with silicone implants. In another series of 53 cases, Venus & Prinsloo26 observed 7.4% of capsular contracture in cases that required capsulotomy and 33% of capsular contracture in those that did not require surgery.
In the present study of 16 patients, none showed any changes in implant coverage like muscle and skin atrophy.
We note that five days were enough to clear the queue of the 16 SCPMR-HUWC patients waiting for breast reconstruction.
The vast majority of patients were discharged in less than four days, which shows that this kind of a joint Task Force does not hinder the operation of the hospital hotel structure.
The surgeries were performed on 2 consecutive weekends, and the surgical operation was also unaffected, because the SCPMR-HUWC elective surgeries are mostly performed during the week.
Because the task forces comprised of a heterogeneous group of plastic surgeons from other institutions, it encouraged an exchange of experiences and innovations in techniques, as well as established new partnerships and strengthened old ties.
Plastic surgery has an important role in the treatment of patients with breast cancer. In this work, a high degree of satisfaction in patients was observed due to the results and few complications. However, in spite of the surgeries being elective and performed by senior plastic surgeons, we had a high number of complications. This rate was consistent with that in the literature, probably in the study in question, of a fortuitous nature. Thus, we conclude that the joint Task Forces of breast reconstruction for post mastectomy cases are a viable alternative in terms of public health.
COLLABORATIONS
|
AM |
Analysis and/or interpretation of data; statistical analyses; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents. |
|
SGPP |
Analysis and/or interpretation of data; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents. |
REFERENCES
1. Brasil. Ministério da Saúde. Instituto Nacional de Câncer. José Alencar Gomes da Silva (INCA). Estimativa 2012: Incidência de Câncer no Brasil. Rio de Janeiro: INCA; 2011.
2. Cheville AL, Tchou J. Barriers to rehabilitation following surgery for primary breast cancer. J Surg Oncol. 2007;95(5):409-18. DOI: http://dx.doi.org/10.1002/jso.20782
3. Ribeiro RVE, Silva GB, Augusto FV. Prevalência do transtorno dismórfico corporal em pacientes candidatos e/ou submetidos a procedimentos estéticos na especialidade da cirurgia plástica: uma revisão sistemática com meta-análise. Rev Bras Cir Plást. 2017;32(3):428-35.
4. Ching AW, Costa MP, Brasolin AG, Ferreira LM. Influência das complicações pós-operatórias no insucesso da reconstrução de mama imediata com implante de silicone. Rev Bras Cir Plást. 2015;30(2):182-9.
5. Alves VL, Sabino Neto M, Abla LEF, Oliveira CJR, Ferreira LM. Avaliação precoce da qualidade de vida e autoestima de pacientes mastectomizadas submetidas ou não à reconstrução mamária. Rev Bras Cir Plást. 2017;32(2):208-17.
6. Sheppard LA, Ely S. Breast cancer and sexuality. Breast J. 2008;14(2):176-81. DOI: http://dx.doi.org/10.1111/j.1524-4741.2007.00550.x
7. Keith DJ, Walker MB, Walker LG, Heys SD, Sarkar TK, Hutcheon AW, et al. Women who wish breast reconstruction: characteristics, fears, and hopes. Plast Reconstr Surg. 2003;111(3):1051-6. DOI: http://dx.doi.org/10.1097/01.PRS.0000046247.56810.40
8. Cammarota MC, Galdino MCA, Lima RQ, Almeida CM, Ribeiro Junior I, Moura LG, et al. Avaliação das simetrizações imediatas em reconstrução de mama. Rev Bras Cir Plást. 2017;32(1):56-63.
9. Oliveira LD. Análise retrospectiva da casuística pessoal em mamoplastia redutora utilizando a técnica de pedículo inferior em suas diferentes indicações. Rev Bras Cir Plást. 2016;31(3):321-7.
10. Miranda RE, Pereira JB, Gragnani Filho A. Uso de duas telas de polipropileno na área doadora do TRAM para reconstrução mamária: avaliação na incidência de hérnia e abaulamento abdominal. Rev Bras Cir Plást. 2015;30(4):560-6.
11. Tavares-Filho JM, Franco D, Moreto L, Porchat C, Franco T. Utilização do retalho miocutâneo de grande dorsal, com extensão adiposa, nas reconstruções mamárias: uma opção para preenchimento do polo superior. Rev Bras Cir Plást. 2015;30(3):423-8.
12. Saldanha Filho OR, Saldanha O, Cação E, Menegazzo MR, Cazeto D, Canchica AC, et al. Reconstrução de mama com miniabdominoplastia reversa. Rev Bras Cir Plást. 2017;32(4):505-12.
13. Sociedade Brasileira de Cirurgia Plástica (SBCP). Câncer de mama: mutirão de reconstrução mamária vai realizar 842 cirurgias. São Paulo; 2016. [acesso 2017 Abr 16]. Disponível em: http://www2.cirurgiaplastica.org.br/2016/10/20/cancer-de-mama-mutirao-de-reconstrucao-mamaria-vai-realizar-842-cirurgias/
14. Veiga DF, Veiga-Filho J, Ribeiro LM, Archangelo I Jr, Balbino PF, Caetano LV, et al. Quality-of-life and self-esteem outcomes after oncoplastic breast-conserving surgery. Plast Reconstr Surg. 2010;125(3):811-7. PMID: 20195109 DOI: http://dx.doi.org/10.1097/PRS.0b013e3181ccdac5
15. Bellino S, Fenocchio M, Zizza M, Rocca G, Bogetti P, Bogetto F. Quality of life of patients who undergo breast reconstruction after mastectomy: effects of personality characteristics. Plast Reconstr Surg. 2011;127(1):10-7 PMID: 21200194 DOI: http://dx.doi.org/10.1097/PRS.0b013e3181f956c0
16. Gart MS, Smetona JT, Hanwright PJ, Fine NA, Bethke KP, Khan SA, et al. Autologous options for postmastectomy breast reconstruction: a comparison of outcomes based on the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg. 2013;216(2):229-38. DOI: http://dx.doi.org/10.1016/j.jamcollsurg.2012.11.003
17. Cosac OM, Camara Filho JPP, Barros APGSH, Borgatto MS, Esteves BP, Curado DMDC, et al. Reconstruções mamárias: estudo retrospectivo de 10 anos. Rev Bras Cir Plást. 2013;28(1):59-64. DOI: http://dx.doi.org/10.1590/S1983-51752013000100011
18. Overgaard M, Hansen PS, Overgaard J, Rose C, Andersson M, Bach F, et al. Postoperative radiotherapy in high-risk premenopausal women with breast cancer who receive adjuvant chemotherapy. Danish Breast Cancer Cooperative Group 82b Trial. N Engl J Med. 1997;337(14):949-55. DOI: 10.1056/NEJM199710023371401 DOI: http://dx.doi.org/10.1056/NEJM199710023371401
19. Saliba GAM, Carvalho EES, Silva Filho AF, Alves JCRR, Tavares MV, Costa SM, et al. Reconstrução mamária: análise de novas tendências e suas complicações maiores. Rev Bras Cir Plást. 2013;28(4):619-26.
20. Ragaz J, Jackson SM, Le N, Plenderleith IH, Spinelli JJ, Basco VE, et al. Adjuvant radiotherapy and chemotherapy in node-positive premenopausal women with breast cancer. N Engl J Med. 1997;337(14):956-62. DOI: 10.1056/NEJM199710023371402 DOI: http://dx.doi.org/10.1056/NEJM199710023371402
21. Clarke M, Collins R, Darby S, Davies C, Elphinstone P, Evans E, et al.; Early Breast Cancer Trialists' Collaborative Group (EBCTCG). Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005;366(9503):2087-106. DOI: http://dx.doi.org/10.1016/S0140-6736(05)67887-7
22. Shah C, Kundu N, Arthur D, Vicini F. Radiation therapy following postmastectomy reconstruction: a systematic review. Ann Surg Oncol. 2013;20(4):1313-22. DOI: 10.1245/s10434-012-2689-4 DOI: http://dx.doi.org/10.1245/s10434-012-2689-4
23. Perdikis G, Koonce S, Collis G, Eck D. Latissimus dorsi myocutaneous flap for breast reconstruction: bad rap or good flap? Eplasty. 2011;11:e39. PMID: 22031843
24. Farah AB, Nahas FX, Mendes JA. Reconstrução mamária em dois estágios com expansores de tecido e implantes de silicone. Rev Bras Cir Plást. 2015;30(2):172-81.
25. Delay E, Gounot N, Bouillot A, Zlatoff P, Rivoire M. Autologous latissimus breast reconstruction: a 3-year clinical experience with 100 patients. Plast Reconstr Surg. 1998;102(5):1461-78. DOI: http://dx.doi.org/10.1097/00006534-199810000-00020 DOI: http://dx.doi.org/10.1097/00006534-199810000-00020
26. Bonomi S, Settembrini F, Salval A, Gregorelli C, Musumarra G, Rapisarda V. Current indications for and comparative analysis of three different types of latissimus dorsi flaps. Aesthet Surg J. 2012;32(3):294-302. DOI: 10.1177/1090820X12437783 DOI: http://dx.doi.org/10.1177/1090820X12437783
27. Venus MR, Prinsloo DJ. Immediate breast reconstruction with latissimus dorsi flap and implant: audit of outcomes and patient satisfaction survey. J Plast Reconstr Aesthet Surg. 2010;63(1):101-5. DOI: 10.1016/j.bjps.2008.08.064 DOI: http://dx.doi.org/10.1016/j.bjps.2008.08.064
1. University of Belgrade, Belgrade,
Serbia.
2. Hospital Universitário Walter Cantídio,
Universidade Federal do Ceará, Fortaleza, CE, Brazil.
Corresponding author: Aleksandra Markovic, Av. Beira Mar, 4260 - Praia de Mucuripe - Fortaleza, CE, Brazil. Zip Code 60165-121. E-mail: 19quepasa19@gmail.com
Article received: September 27, 2017.
Article accepted: June 22, 2018.
Conflicts of interest: none.
















 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter