

Original Article - Year 2018 - Volume 33 -
Alternative technique for the treatment of osteonecrosis in breasts: description and results
Alternativa técnica para tratamento de esteatonecrose em mama: descrição e resultados
ABSTRACT
Introduction: This work describes and presents the results of an
alternative technique for treating steatonecrosis by liposuction
using a specific cannula, with good physical and imaging results.
Steatonecrosis is a complication that frequently occurs during
mammary surgeries, especially during mammary reconstructions
and in conservative surgery or TRAM. Steatonecrosis is
characterized initially by hardening of the tissue that may
develop into nodules of different sizes in any mammary region
with oily cysts and fibrosis; consequently, steatonecrosis is
a constant concern for patients, oncologists, breast cancer
specialists, and plastic surgeons due to the possibility of tumor
recurrence.
Method: A retrospective review of the medical
records of the patients undergoing procedures related to the
breast, either reconstructive or aesthetic, was performed.
Patients who developed steatonecrosis and were treated by
liposuction, similar to the bone drilling technique performed by
orthopedic surgeons for the treatment of bone necrosis, were
included in the study.
Results: Eight patients from the study
period reviewed were selected. The mean age was 56 years.
Most of the patients showed deformity in the affected breast,
with oily cysts, reported in 5 patients (62.5%), being the most
common deformity. Breast cancer history was reported for
75% of the patients.
Conclusion: The individualization of the
patient is the key to successful treatment of steatonecrosis and
an essential tool to satisfy the expectations and desires of the
patient after this complication. Each technique has its indications,
advantages and limitations, which should be thoroughly
discussed with the patient to obtain the best possible result.
Keywords: Fat necrosis; Breast implants; Mammaplasty; Breast neoplasms; Mastectomy, segmental
RESUMO
Introdução: Este trabalho descreve e apresenta os resultados de uma técnica alternativa
para tratamento da esteatonecrose, a lipoaspiração com cânula específica,
com bons resultados observados no exame físico e de imagem. A esteatonecrose
é uma complicação que ocorre com alguma frequência nas cirurgias mamárias,
principalmente nas reconstruções mamárias, nas cirurgias conservadoras ou
TRAM, caracterizando-se, inicialmente, por endurecimento de uma região, que
evolui para uma nodulação de tamanhos variados, em qualquer região mamária,
com cistos oleosos e fibrose, que traduz uma preocupação constante por parte
das pacientes, do oncologista, do mastologista e do cirurgião plástico
devido à ocorrência de recidiva tumoral.
Método: Foi realizada uma revisão retrospectiva dos prontuários das pacientes
submetidas a procedimentos nas mamas, seja reconstrução ou estética, e
evoluíram com esteatonecrose, sendo submetidas ao tratamento com
lipoaspiração, inspirada na técnica de perfuração óssea para tratamento de
necrose óssea, realizado por ortopedistas.
Resultados: No período englobado, 8 pacientes foram selecionadas. A idade média foi de 56
anos. Grande parte possuía alguma deformidade na mama acometida, sendo o
cisto oleoso o mais comum - 5 pacientes (62,5%). 75% possuíam história de
neoplasia mamária.
Conclusão: A individualização do paciente é a chave para o sucesso do tratamento da
esteatonecrose e uma ferramenta essencial para atender às expectativas e
anseios da paciente após essa complicação. Cada técnica tem suas indicações,
vantagens e limitações, que devem ser amplamente discutidas com o paciente
visando o melhor resultado possível.
Palavras-chave: Necrose gordurosa; Implantes de mama; Mamoplastia; Neoplasias da mama; Mastectomia segmentar
INTRODUCTION
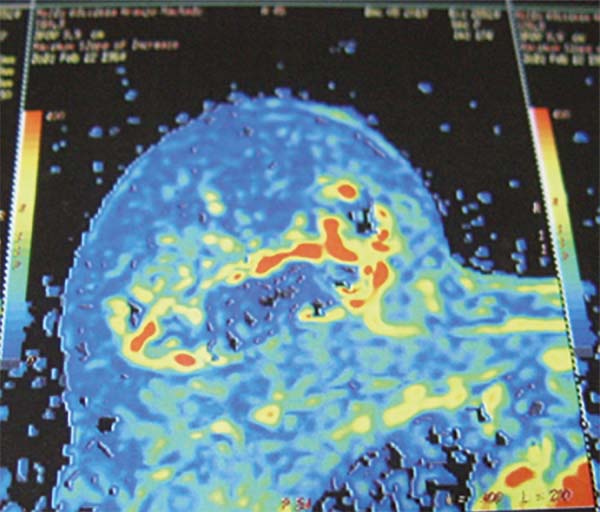
Steatonecrosis is a common benign condition that may be asymptomatic or may manifest as a palpable mass, pain, or associated findings, such as skin thickening or nipple retraction. Steatonecrosis can have several mammographic aspects. Common and characteristic findings are circumscribed radiolucent masses or mixed density masses with fat and soft tissues, with or without a calcified border; these masses are known as lipid or oily cysts1,2 (Figure 1).
These are observed after any breast trauma, including surgery. Steatonecrosis is commonly observed after nodule resection and radiotherapy for breast carcinoma and after extensive surgery3. It is a complication that occurs frequently during breast surgeries, especially in breast reconstructions and in the conservative surgeries or TRAM. Steatonecrosis is initially characterized by hardening of the tissue that may develop into a nodule of different sizes in any mammary region with oily cysts and fibrosis. This condition is a constant concern for the patients, oncologists, mastologists, and plastic surgeon, due to the possibility of tumor recurrence.
Pathology
The initial change is the disruption of fat cells, where vacuoles with the remains of necrotic fat cells are formed, as observed under a microscope. The cells then become surrounded by lipid-laden macrophages, multinucleated giant cells, and acute inflammatory cells. Fibrosis develops during the repair phase, peripherally enclosing a possibly palpable area of necrotic fat and cellular debris at the surgical site. Fibrosis may eventually replace the degenerated fat area by a scar or the degenerated fat may persist for years within a fibrotic scar4,5 (Figure 2).
Radiological Findings
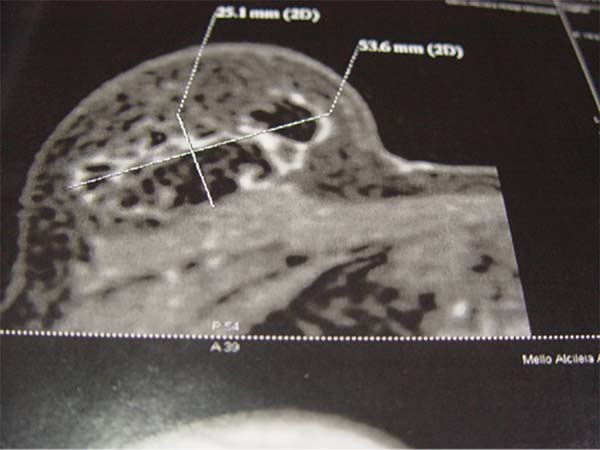
The density and spicules, common in recent extensive surgeries associated with radiotherapy, disappear or become radiolucent and circumscribed nodules (oily cysts; Figure 3) over a variable period of time, lasting up to 4 years. In addition, amorphous and nonspecific calcifications become more peripheral and coarse. Coarse calcifications associated with steatonecrosis should be described as dystrophic6-9.
In subcicritrial recurrence, the mammographic findings become more suspicious compared to previous examinations. The density of the tissue and the number of spicules and/or amorphous calcifications increase10,11.
The markings of the surgical scar by appropriate radiopaque marker may be useful for the spatial correlation between the mammographic findings and the scar. The linear radiopaque marker is usually standardized for surgical scarring in the breast12.
OBJECTIVE
To describe an alternative technique for the treatment of steatonecrosis after aesthetic and reconstructive mammoplasty.
METHODS
The medical records of the patients admitted for breast surgery, either for the treatment of breast neoplasia and adjuvant therapies or cosmetic surgery, during the period of 2012-2016 were retrospectively reviewed. Patients who developed steatonecrosis and were treated by liposuction, similar to the technique performed by orthopedists for the treatment of bone necrosis, were included.1,2
All patients signed an informed consent form authorizing the use of their records and information about their treatment, as well as their photographs and examination findings for scientific purposes.
The data analyzed included the characteristics of the skin (deformities), previous surgeries performed, and the aesthetic results associated with the surgical technique for the alternative treatment of steatonecrosis.
The treatment of steatonecrosis was defined by the plastic surgeon, preceptor author, inspired by the technique of bone perforation for the treatment of bone necrosis, performed by orthopedics (forage)1,2. A lipped aspiration cannula was developed for the treatment of hydroadenitis and hyperhidrosis. It was decided to experiment with the perforation and aspiration of steatonecroses which are develop frequently in mammary reconstructions and mammoplasties.
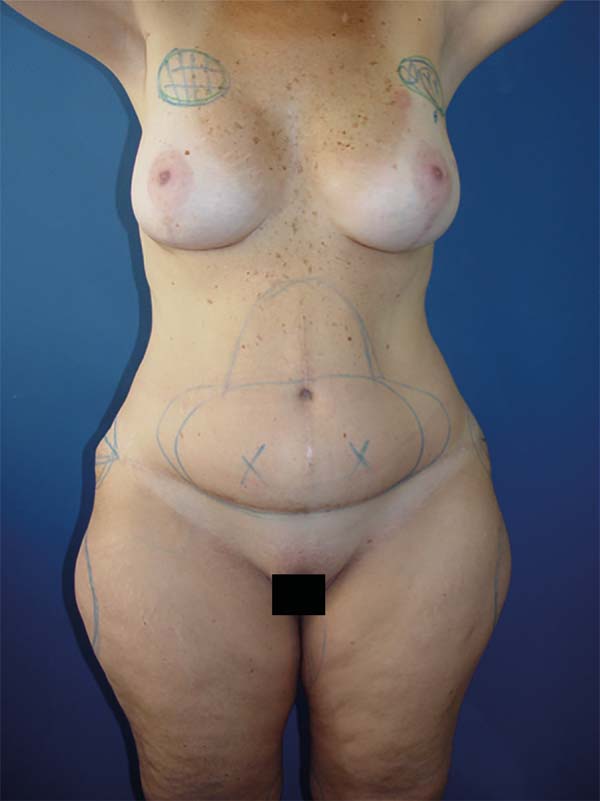
We delimited the area of necrosis (Figure 4), and after routine infiltration of the region, we introduced the cannula inside the necrotic nodule and made several perforations with it; the cannula was connected to the liposuction device, which sucked part of the necrotic tissue and the surrounding oily contents that eventually develop into cysts in these nodules.
We believe that there is neovascularization in these areas; the areas are softened, thus, preventing the development of deformities due to surgical resection in these areas.
All procedures were performed by the same surgeon. The method chosen was based on the careful analysis of the case by the assistant plastic surgeon, and the procedure was explained to the patient.
All patients underwent postoperative follow-up for at least 10 months.
RESULTS
Eight patients were selected from the study period reviewed.
The mean age of the patients was 56 years.
All patients showed some deformity in the affected breast that was detected by nuclear magnetic resonance; the average size of the nodule was 1.8 cm, with oily cysts, reported in 5 patients (62.5%), being the most common.
Of the total number of patients, 75% had a history of breast neoplasia.
DISCUSSION
The classic treatment consists of removing the nodules and fibrosis, which often lead to deformity of the breast, with loss of volume and the shape of the reconstructed breast. The technique proposed in this work proposes to minimize these effects of the classical resection technique by liposuction and stimulation of neovascularization.
This study is one of the pioneering works in the national literature on the evaluation of an alternative method for the treatment of steatonecrosis.
When searching for articles from other countries on this subject, we noticed a few specific works.
Characteristics of the skin
The long-term evaluation, with a minimum follow-up of 12 months, showed complete regression of the palpable nodules. No superficial deformities or retractions were observed in the areas subjected to liposuction.
Treatment proposed and adopted
All patients underwent the proposed surgery, involving the perforation and aspiration of the steatonecroses, delimiting the area of necrosis, and after routine infiltration of the region, the cannula was inserted inside the necrotic nodule and several perforations were made. The cannula was connected to the liposuction device, which sucked part of the necrotic tissue and the oily contents that eventually develop into cysts.
Aesthetic results of the surgical technique for the alternative treatment of steatonecrosis
All patients were satisfied with the final aesthetic result; there were no complaints of depression, palpable nodule, or retractions.
Additional studies are required to better characterize this treatment modality and to conduct a more detailed analysis of this sample group, in addition to the increase in the number of patients submitted. Our work is the basis for future studies on the subject with greater n, using a questionnaire designed to document patient satisfaction.
CONCLUSIONS
We conclude that the individualization of the patient is the key to the successful treatment of steatonecrosis and an essential tool to satisfy the expectations and wishes of the patient after this complication. Each technique has its indications, advantages and limitations, which must be widely discussed with the patient to obtain the best possible result. The advantages of the proposed technique include absence of deformities and patient satisfaction.
COLLABORATIONS
|
LDPB |
Analysis and/or interpretation of data; statistical analyses; conception and design of the study; completion of surgeries and/ or experiments; writing the manuscript or critical review of its contents. |
|
OMC |
Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study. |
|
MCC |
Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript. |
|
LMCD |
Analysis and/or interpretation of data; statistical analyses; writing the manuscript or critical review of its contents. |
|
MCAG |
Analysis and/or interpretation of data; statistical analyses; writing the manuscript or critical review of its contents. |
|
IRJ |
Analysis and/or interpretation of data; statistical analyses. |
REFERENCES
1. Althoff FP, Petrelli ASC. Correlação dos achados mamográficos com o sistema BI-RADS. [Monografia]. Rio de Janeiro: Curso de Pós-Graduação da Santa Casa de Misericórdia do Rio de Janeiro; 2005.
2. American College of Radiology. ACR BI-RADS Mammography. 4th ed. In: ACR Breast Imaging Reporting and Data System, Breast Imaging Atlas. Reston: American College of Radiology; 2003.
4. Bargum K, Nielsen SM. Case report: fat necrosis of the breast appearing as oil cysts with fat-fluid levels. Br J Radiol. 1993;66(788):718-20. DOI: 10.1259/0007-1285-66-788-718 DOI: http://dx.doi.org/10.1259/0007-1285-66-788-718
5. Taboada JL, Stephens TW, Krishnamurthy S, Brandt KR, Whitman GJ. The many faces of fat necrosis in the breast. AJR Am J Roentgenol. 2009;192(3):815-25. DOI: 10.2214/AJR.08.1250 DOI: http://dx.doi.org/10.2214/AJR.08.1250
6. Bekler HI, Erdag Y, Gumustas SA, Pehlivanoglu G. The Proposal and Early Results of Capitate Forage as a New Treatment Method for Kienböck's Disease. J Hand Microsurg. 2013;5(2):58-62. DOI: http://dx.doi.org/10.1007/s12593-013-0098-y
7. Godinho ER, Koch HA. Submissão às recomendações do BI-RADS(tm) por médicos e pacientes: análise preliminar de 3.000 exames realizados em uma clínica particular. Radiol Bras. 2004;37(1):21-3. DOI: http://dx.doi.org/10.1590/S0100-39842004000100006
8. Aguillar V, Bauab S, Maranhão N. Relatório mamográfico e ultra-sonográfico segundo o BI-RADS. Guia e dúvidas. In: Aguillar V, Bauab S, Maranhão N, eds. Mama: diagnóstico por imagem. 1ª ed. Rio de Janeiro: Revinter; 2009. p. 301-4.
9. Kopans DB. Analisando a mamografia. In: Kopans DB, ed. Imagem da mama. 2ª ed. Rio de Janeiro: Medsi; 1998. 332 p.
10. Jackson VP, Jahan R, Fu YS. Lesões benignas da mama. In: Basset LW, Jackson VP, Jahan R, Fu YS, Gold RH, eds. Doenças da mama. Diagnóstico e tratamento. 1ª ed. Rio de Janeiro: Revinter; 2000.
11. Sickles EA, D'Orsi CJ, Bassett LW. ACR BI-RADS® Mammography. In: ACR BI-RADS® Atlas, Breast Imaging Reporting and Data System. Reston: American College of Radiology; 2013.
12. http://www.indatasus.gov.br/siscam/siscam.php
1. Sociedade Brasileira de Cirurgia Plástica, São
Paulo, SP, Brazil.
2. Hospital Daher Lago Sul, Brasília, DF,
Brazil.
3. Hospital das Forças Armadas, São Paulo, SP,
Brazil.
Corresponding author: Ognev Meireles Cozac, SGA/L2 Sul Quadra 616, Conjunto A, Loja 06. Centro clínico Linea Vitta - Brasília, DF, Brazil. Zip Code 70200-760. E-mail: ognev@terra.com.br
Article received: December 1, 2016.
Article accepted: May 17, 2018.
Conflicts of interest: none.






 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter