

Original Article - Year 2018 - Volume 33 -
Treatment of breast ptosis with submuscular implants and points of attachment of the breast to the pectoralis muscle: technical considerations and outcome assessment
Tratamento das ptoses mamárias com implantes submusculares e pontos de fixação do tecido mamário ao muscular: aspectos técnicos e avaliação de resultado
ABSTRACT
Introduction: Mastopexy associated with implant placement is
challenging for plastic surgeons. The objective is to describe the
placement of a submuscular implant with anatomical detachment
in combination with stable fixation of the breast tissue to the
pectoralis muscle and analyze the aesthetic results.
Method: Twenty-three mastopexy procedures with implants were
performed from April 2015 to July 2017 by the same surgeon,
and surgical markings were made in the breasts of the patients
in a seated position. An incision was made in the inframammary
fold, and the breast tissue was elevated to the upper pole in the
subfascial plane and attached to the pectoralis major muscle
using 9-12 stitches. Subsequently, the inferior margin of the
pectoralis major muscle and the transition from the rectus
abdominis muscle to the serratus muscle were dissected to
expose the muscle. The implant was introduced and mastopexy
was completed. Implant size ranged from 255 mL to 355 mL.
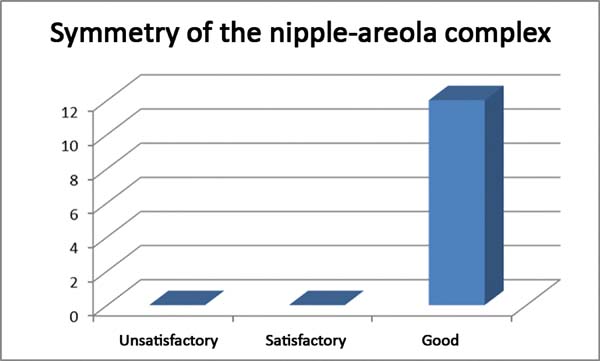
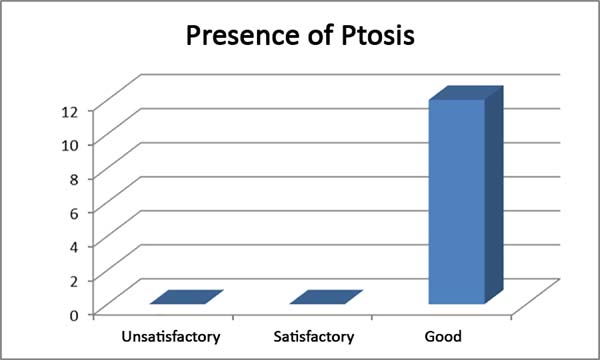
Photographs of the breasts of 12 patients were evaluated by two
plastic surgeons and two non-medical subjects, who considered
the aesthetic results, symmetry of the nipple-areola complex, and
degree of breast ptosis. The results were scored as unsatisfactory,
satisfactory, or good.
Results: The surgical technique was
reproducible; there was only one case of unilateral hematoma,
no implant infections, and only complaints of mild pain. Only
one case was scored as satisfactory by one evaluator, whereas the
results of the other cases were considered good.
Conclusion: The treatment of breast ptosis with the placement of a submuscular
implant in combination with fixation of the breast to the pectoralis
major muscle is reproducible and yields good aesthetic results.
Keywords: Mammoplasty; Breast implant; Reconstructive surgical procedures; Breast; Tissue fixation
RESUMO
Introdução: Mastopexia associada à inclusão de implante é uma situação desafiadora para o
cirurgião plástico. O objetivo é descrever a colocação de implante
submuscular com descolamento anatômico mais pexia firme do tecido glandular
usando pontos de fixação do tecido mamário ao muscular e analisar os
resultados estéticos das pacientes operadas.
Método: Foram realizadas 23 mastopexias com implantes no período entre abril de 2015
e julho de 2017, pelo mesmo cirurgião, sendo as mamas das pacientes marcadas
previamente, na posição sentada. Realizou-se incisão no sulco mamário e
descolamento até o polo superior da mama no plano subfascial, fixação da
glândula ao músculo peitoral maior com 9 a 12 pontos. A seguir, iniciou-se a
dissecção do músculo peitoral maior através de sua origem costal e transição
com os músculos reto abdominal e serrátil, liberando amplamente na porção
inferior. Introduziu-se o implante e completou-se a mastopexia. Os tamanhos
dos implantes variaram de 255ml a 355ml. Fotos das mamas de 12 pacientes
foram avaliadas por dois cirurgiões plásticos e dois leigos, nos seguintes
parâmetros: resultado estético, simetria das aréolas e grau de ptose
mamária. As avaliações podiam ser Ruim, Razoável ou Bom.
Resultados: A técnica cirúrgica mostrou-se reprodutível, apenas 1 caso de hematoma
unilateral, nenhuma infecção, queixas de dor discretas. Apenas um caso foi
considerado, por um único avaliador, como Razoável; as demais avaliações
consideradas como Bom.
Conclusão: O tratamento de ptoses mamárias com colocação de implante submuscular
acrescido de pexia da glândula ao músculo peitoral é uma técnica
reprodutível e com bons resultados estéticos.
Palavras-chave: Mamoplastia; Implante mamário; Procedimentos cirúrgicos reconstrutivos; Mama; Fixação de tecidos
INTRODUCTION
In hypomastia patients with the need for implant placement, mastopexy is a common surgery and may provide satisfactory results for the patient and the surgeon. However, this procedure presents a high rate of poor outcomes and reoperations. Moreover, the implant volumes have increased over the years, which may accelerate postoperative ptosis and increase the patient’s demand for better aesthetic results. Even patients with more evident ptosis and flaccidity expect to achieve results similar to those of patients with normal breasts, which led us to incorporate some technical changes in the procedure.
The development of these technical modifications was based on the cases of significant encapsulation and hypomastia suggesting a change in the location of the implant pocket and closure of the previous pocket by anchoring the breast to the muscle.
Subfascial detachment was performed, and the breast tissue was attached to the pectoralis major muscle using fixation points. The need to attach the lower pole of the breast led us to approach the muscle more inferiorly than in the dual-plane technique and perform anatomical detachment, which helped reduce postoperative pain and increase implant coverage by the muscle.
Several authors1-7 have proposed including implants in submuscular pockets using the dual-plane technique to reduce the tendency of ptosis in the postoperative period, prevent rippling, and provide more natural contours to the implanted breasts.
The presence of breast flaccidity and ptosis limit maintenance of the aesthetic result obtained with implant placement because of the tendency of the breast and the implant to sag, even when fixation is performed adequately and subfascial or subglandular implants are used8-11, especially in cases in which the pectoral fascia is fragile and has limited capacity to support the implants.
The alternative in these cases is placing the implants in the submuscular pocket, which has the advantage of supporting the weight of the implants and concealing the contour of the implants, leading to more natural results, especially for patients with significant hypomastia. The disadvantage of this type of implant is postoperative pain and the possibility of implant dislocation in the upper portion of the breast and/or breast ptosis, resulting in an unsightly appearance (double bubble deformity).
Even a submuscular implant may not prevent ptosis, as skin and glandular sagging is significant in these cases, potentially leading to breast ptosis and compromising the surgical result.
OBJECTIVE
The objective of this study was to describe the technique of placement of submuscular implants with anatomical detachment in combination with tight anchoring of the breast to the pectoralis major muscle using attachment points and to analyze the aesthetic results in those who underwent the operation.
METHOD
A total of 23 mastopexy procedures with inverted T scars combined with the inclusion of submuscular implants were performed from April 2015 to July 2017. All surgeries were executed bilaterally using round-shaped high-profile textured breast implants (volumes of 255-355 mL) in patients with evident breast ptosis and flaccidity. Twenty-two patients from the private clinic and one patient from the University Hospital of the State University of Londrina were included. The same surgeon performed surgery on all patients under thoracic epidural anesthesia following a protocol of prevention of thromboembolism, use of prophylactic antibiotic, and hospitalization for 24 hours.
Surgical procedure
The patients underwent operation in the horizontal dorsal decubitus position with abduction of the upper limbs at 90º. Infusion of epinephrine solution (1:500,000) on the surgical markings allowed for easy removal of excess skin and elevated the nipple-areola complex. These marks were previously performed with the patient in a seated position.
Surgery was initiated with an incision on the inframammary fold and subfascial elevation to the level of the nipple-areola complex with an electrocautery scalpel to preserve blood supply and integrity of the pectoral fascia. From this point, detachment was subglandular by creating a pocket sufficient to accommodate most of the breast base, while attempting to keep the detachment at safe levels to preserve breast sensitivity and blood supply, as proposed by Spear12.
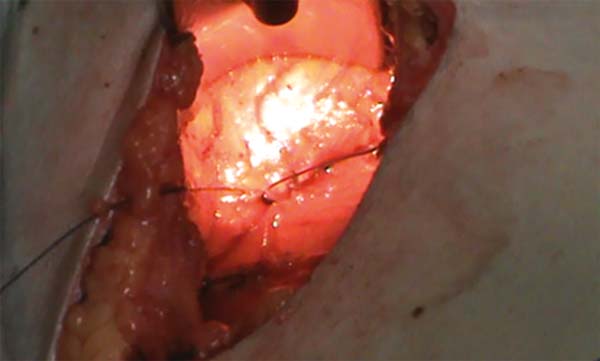
The next step was to attach the breast to the pectoralis major muscle using 9-12 stitches with absorbable 3.0 multifilament thread (Figure 1). During this procedure, the breast was held upright by two 2.0-cotton thread stitches positioned at the apex of the new mammary cone (Figure 2). At the end of the procedure, breast fixation was adequate compared to the non-operated side (Figure 3).
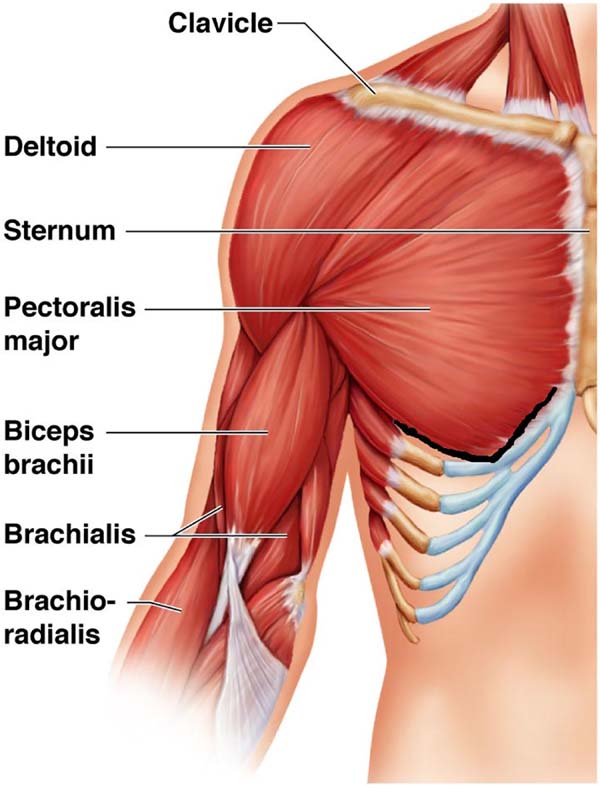
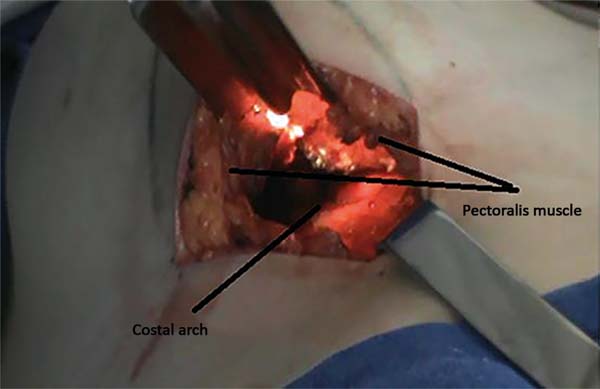
After tissue fixation, the pectoralis major muscle was dissected as anatomically as possible by 1) approaching the muscle from its inferior portion, separating it from the proximal portion of the rectus abdominis muscle; 2) making a small incision in the sternal attachment to preserve the pectoral fascia; and 3) dissecting the pectoralis major muscle in the transition with the serratus muscle in the direction of the muscle fibers.
This surgical approach is intended to expose the muscle (Figures 4 and 5) and leave it as free as possible from the muscle sheath in the lower portion to prevent superior implant dislocation. We emphasize that the muscle was not sectioned extensively. As a routine procedure, drainage was not performed, hemostasis in the detached areas was rigorous, and hypotension was prevented for the safer control of hemostasis.
Submuscular detachment was performed using electrocautery coagulation and an illuminated retractor, limiting the detachment to the superior aspect of the submuscular pocket, and leaving the pectoralis minor muscle intact. In the lateral aspect of the submuscular pocket, the detachment was close to the costal arch, creating a pocket that provided good muscular coverage for the implant.
Following this, excess skin was removed, the nipple-areola complex was repositioned, the margins were suture using 2.0 nylon threads, and cutaneous closure was performed using subdermal and intradermal sutures with absorbable threads.
For an initial evaluation of the results, a file was prepared with photos of the breasts of 12 patients randomly chosen in the following profiles: frontal, oblique, and lateral (right side) in the preoperative period and 3 months after surgery. The evaluations were made by two plastic surgeons and two non-medical individuals, including a patient who underwent abdominoplasty and another patient who received a breast implant without fixation.
The overall aesthetic result, symmetry of the nipple-areola complex, and degree of breast ptosis were evaluated using a score from 1 to 10 as follows: 1-4, unsatisfactory; 5-6, satisfactory; and 7-10, good.
RESULTS
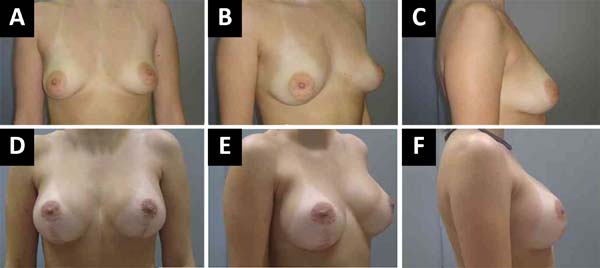
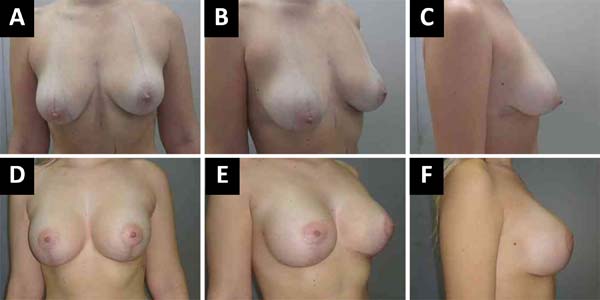
The surgical technique was reproducible. Only one aesthetic result was considered satisfactory (Figure 6) whereas the other results for the symmetry of the nipple-areola complex (Figure 7) and presence of ptosis (Figure 8) were considered good by the evaluators.
There was one case of massive unilateral hematoma, with the need for surgical drainage, and no cases of seroma. Furthermore, three patients presented small skin lesions at the junction of the T scars on the inframammary fold, which healed spontaneously. There were complaints of mild pain and no cases of extrusion or implant infection. Two patients had a transient decrease in areolar sensitivity, and three patients had unilateral superior dislocation of the implant with slight asymmetry.
DISCUSSION
Some limitations of implant placement using the dual-plane technique in cases of ptosis and flaccidity led us to search for surgical alternatives. We sought to provide greater implant coverage using the pectoralis major muscle, approaching the muscle anatomically to allow full use of this muscle for implant coverage and reduce postoperative pain.
Stable fixation of the breast to the muscle tissue was included in this surgical strategy to minimize the risk of breast ptosis (double bubble deformity). Although several studies did not emphasize the intensity of postoperative pain, this factor is relevant and often increases patient resistance to use implants in the submuscular pocket.
Daher et al.8 reported that the degree of satisfaction in mastopexy procedures with submuscular and subglandular implants was 90-96%, and the rate of reoperation was 6.58%. These authors also reported that the use of submuscular implants caused postoperative pain but did not describe breast attachment to the muscle. Implant volumes ranged from 150 mL to 400 mL. This result was different from ours; our patients did not have significant complaints of pain, despite the use of stitches to attach the breast to the muscle and significant muscular detachment.
Daniel1 describes a dual-plane method using a 3 cm-wide muscle sheath of the lower portion of the pectoralis major muscle to prevent ptosis. The implant volume varied from 135 mL to 550 mL and ranged from 215 mL to 285 mL in most cases. In this surgical strategy incisions are made in the inferior region of the pectoralis major muscle and the implant is not covered extensively; consequently, rippling in the upper portion may occur. In our study, we tried to cover the implant extensively, and consequently, minimize the chances of rippling.
Sanches et al.6 described the use of large submuscular pockets to accommodate implants by using a small disinsertion of the inferomedial portion of the pectoralis major muscle without the use of stitches to attach the breast to the muscle tissue, and implant volumes ranged from 200 mL to 240 mL. Despite the extensive muscle detachment, the authors did not attach the mammary tissue to the muscle, and the attachment proposed herein may be an important contribution of our study. We believe that this attachment helps maintain the long-term result.
Khan5 described the use of internal fixation for mild degrees of ptosis via the inframammary access without removing skin, the use of a muscle-splitting pocket, upper pole detachment above the upper border of the muscle and sutures, and attachment of the lower pole of the breast with fixation points in the fascia of the upper portion of the pectoralis major muscle. Implant volumes ranged from 260 mL to 440 mL. We believe it is essential to remove excess skin to help fixation in cases of more obvious ptosis.
Bruschi et al.2 described a pectoralis muscle-splitting technique in periareolar mastopexy using a mixed pocket and attachment of the lower pole of the breast to the upper portion of the pectoralis major muscle. However, the number of stitches was not mentioned. Implant volumes ranged from 250 mL to 355 mL.
One of the advantages was that attaching the breast to the pectoralis major muscle caused more stable and permanent positioning of the breasts, significantly reducing the tendency of the tissue to slide over the muscle. In addition to better positioning, the muscular approach was more anatomical, reduced postoperative pain, and provided better implant coverage by the muscle, with more natural results.
This procedure reduced postoperative ptosis, complaints, and retouching. We emphasize that the presence of severe ptosis and flaccidity are contraindications to this approach, and the patients need to collaborate in the late postoperative period by routinely using a bra and avoid weight variations.
The disadvantage of using these technical modifications is a longer surgical time. However, the increase in the number of operations decreases the difference in surgical time compared to the use of a subfascial implant. Another limitation of using submuscular implants is the increased risk of implant dislocation, compromising the aesthetic result. In addition to the strategies already mentioned to reduce this possibility, more compressive dressings in the upper pole of the breast and implant stabilizers were used.
There were three cases of asymmetry due to unilateral superior dislocation of the implants, and in two of these cases, there were no significant complaints by the patients. In only one case, asymmetry was significant because of excessive implant dislocation and excess residual skin, and retouching was scheduled to reposition the implant and remove excess skin.
The detachment of the lower portion of the pectoralis muscle without extensive muscle sectioning usually helps keep the implant in the correct position using compressive dressings and breast implant stabilizers; this procedure also reduces pain. The cases in which it was difficult to reposition the implants can be attributed to asymmetries of the chest with irregularities in the costal arch and/or prolonged muscle contraction due to pain or fear of immobilization of the upper limbs and relaxation of the shoulders.
CONCLUSION
The treatment of breast ptosis associated with flaccidity and/or hypomastia involving the placement of a submuscular implant and anchoring of the breast to the pectoralis muscle using fixation points is a reproducible technique with good aesthetic results (Figures 9 and 10).
The obtained results should be long-lasting, considering the changes proposed to reduce postoperative pain and the risk of glandular ptosis and are advantageous compared to other available options because the period of implementation of these technical modifications is less than two years.
ACKNOWLEDGMENTS
To Renato Silva Freitas, Luciano Sampaio Busato, Marco Aurelio L. Gamborgi, and André Auesvald, directors of the regional branch of the Brazilian Society of Plastic Surgery (Sociedade Brasileira de Cirurgia Plástica-SBCP) of Paraná, Brazil, for encouraging the improvement of the technical modifications presented in this study.
To Milton Keita Maeda and José Garcia Junqueira Neto for the significant contribution to the development of the surgical strategies.
REFERENCES
1. Daniel MJB. Inclusão de Prótese de Mama em Duplo Espaço - Prêmio Georges Arié 2004. Rev Soc Bras Cir Plást. 2005;20(2):82-7.
2. Bruschi S, Bochiotti MA, Ruka E, Fraccalvieri M. "Slip Sliding" technique. A new method to perform mastopexy-augmentation. Eur J Plast Surg. 2015;38(2):117-22. DOI: http://dx.doi.org/10.1007/s00238-014-1027-4
3. Khan UD. Muscle-spliting, subglandular, and partial submuscular augmentation mamoplasties: a 12-year retrospective analysis of 2026 primary cases. Aesthetic Plast Surg. 2013;37(2):290-302. DOI: http://dx.doi.org/10.1007/s00266-012-0026-8
4. Khan UD. Augmentation mastopexy in muscle-spliting biplane: outcome of first 44 consecutive cases of mastopexy in a new pocket. Aesthetic Plast Surg. 2010;34(3):313-21. DOI: http://dx.doi.org/10.1007/s00266-009-9434-9
5. Khan UD. Multiplane technique for simultaneous submuscular breast augmentation and internal glandulopexy using inframammary crease incision in selected patients with early ptosis. Eur J Plast Surg. 2011;34(5):337-43. DOI: http://dx.doi.org/10.1007/s00238-010-0521-6
6. Sanchéz J, Carvalho AC, Erazo P. Mastopexia com prótese: técnica em "D" espelhado. Rev Bras Cir Plást. 2008;23(3):200-6.
7. Soares AB, Franco FF, Rosim ET, Renó BA, Hachmann JOPA, Guidi MC, et al. Mastopexia com uso de implantes associados a retalho de músculo peitoral maior: técnica utilizada na Disciplina de Cirurgia Plástica da Unicamp. Rev Bras Cir Plást. 2011;26(4):659-63. DOI: http://dx.doi.org/10.1590/S1983-51752011000400021
8. Daher JC, Amaral JDLG, Pedroso DB, Cintra Júnior R, Borgatto MS. Mastopexia associada a implante de silicone submuscular ou subglandular: sistematização das escolhas e dificuldades. Rev Bras Cir Plást. 2012;27(2):294-300. DOI: http://dx.doi.org/10.1590/S1983-51752012000200021
9. Carramaschi FR, Tanaka MP. Mastopexia Associada à Inclusão de Prótese Mamária. Rev Bras Cir Plást. 2003;18(1):26-36.
10. Alfaro HMO, Cunha GSR, Vasconcelos FRP, Cosac O, Rosset EGG, Lima DM. Avaliação da ptose pós-operatória em pacientes ex-obesas e não-obesas submetidas a mastopexia com implantes. Rev Bras Cir Plást. 2012;27(3 Suppl. 1):80.
11. Wada A, Millan LS, Gallafrio ST, Gemperli R, Ferreira MC. Tratamento da ptose mamária e hipomastia utilizando técnica de mamoplastia com pedículo súpero-medial e implante mamário. Rev Bras Cir Plást. 2012;27(4):576-83. DOI: http://dx.doi.org/10.1590/S1983-51752012000400018
12. Spear S. Augmentation/Mastopexy: "Surgeon, Beware". Plast Reconstr Surg. 2003;112(3):905-6. PMID: 12960875 DOI: http://dx.doi.org/10.1097/01.PRS.0000072257.66189.3E
1. Universidade Estadual de Londrina, Londrina,
PR, Brazil.
2. Universidade Federal do Paraná, Curitiba, PR,
Brazil.
Corresponding author: Antonio Chiquetti Junior, Rua Paes Leme, 1264, sala 601 - Jardim das Américas, Londrina, PR, Brazil. Zip Code 86010-610. E-mail: chiqueti@sercomtel.com.br
Article received: December 15, 2017.
Article accepted: June 22, 2018.
Conflicts of interest: none.












 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter