

Original Article - Year 2018 - Volume 33 -
Secondary mastopexy with exchange of prosthesis: mirror "D" technique
Mastopexia secundária com troca de prótese: técnica em "D" espelhado
ABSTRACT
Introduction: Breast implantation combined with mastopexy is
challenging, not only because a standard procedure is lacking,
but also because of the high potential for complications,
including a high rate of post-surgical revision. Originally
intended for primary mastopexy and inclusion of silicone
implants in hypoplastic breasts with moderate to severe
ptosis, the use of the mirror "D" technique is now extended to
treatment of ptosis recurrence with displacement of prostheses,
with or without capsular contracture and/or unsightly scars.
Method: The procedure described was performed in 90
patients, using specific marking to determine block resection
of skin and underlying parenchyma for symmetrization. The
procedure included use of a medial pedicle flap and exchange
of original implants for textured, high-profile, round silicone
prostheses with equal volumes bilaterally and positioned
in the submuscular plane, resulting in a final vertical scar.
Results: No surgical revision was required in any of the
cases. There was no occurrence of postoperative infection or
necrosis of the nipple-areola complex or scar. The average
parenchyma resection was 80 g. Eighty-nine patients (98.8%)
were submitted to resection of different volumes. The average
prosthesis volume was 300 mL. The length of the vertical scar
was stable with an average of 6.5 cm after 2 years. The results
were considered satisfactory according to patient assessment.
Conclusion: Secondary mastopexy is a more complex surgery
due to severe atrophy of the tissue as a result of previous
surgery. Its benefits include improved symmetrization, thinner
scars and reduction in tension on the nipple-areola complex,
long-lasting results, and a high degree of patient satisfaction.
Keywords: Breast implants; Mammoplasty; Atrophy; Secondary prevention; Reconstructive surgical procedures
RESUMO
Introdução: A inclusão de implante mamário combinada com pexia é uma cirurgia
desafiadora, não somente pela ausência de procedimento padrão, mas por se
mostrar uma cirurgia com elevado potencial de complicações, entre elas, alto
índice de revisões pós-cirúrgicas. Neste trabalho é descrita a utilização da
técnica em "D" espelhado originalmente usada para mastopexia primária e
inclusão de implantes de silicone em mamas hipoplásicas associadas à ptose
moderada a grave, agora se estendendo o uso para o tratamento de recidiva de
ptoses com deslocamento das próteses com ou sem contratura capsular e/ou
cicatrizes inestéticas.
Método: O procedimento descrito, realizado em 90 pacientes, faz uso de marcação
própria que determina ressecção em bloco de pele e parênquima subjacente
para simetrização, retalho de pedículo medial, troca dos implantes originais
para próteses de silicone texturizada, perfil alto, redonda, volumes iguais
bilateralmente, posicionadas em plano submuscular, resultando em uma
cicatriz final vertical.
Resultados: Pelos dados obtidos não foi necessária revisão cirúrgica em nenhum dos casos.
Não houve ocorrência de infecção pós-cirúrgica ou necrose da placa
areolopapilar, bem como da cicatriz. A ressecção média do parênquima foi de
80g. Oitenta e nove pacientes (98,8%) foram submetidas à ressecção de
diferentes tamanhos. O volume médio das próteses incluídas foi de 300ml. O
comprimento da cicatriz vertical se mostrou estável em média de 6,5cm após 2
anos. Os resultados foram considerados satisfatórios pela avaliação feita
pelos pacientes.
Conclusão: A mastopexia secundária mostrou-se uma cirurgia de maior complexidade devido
à atrofia severa dos tecidos, resultado da cirurgia prévia. Seus benefícios
incluem maior simetrização, cicatrizes mais finas com diminuição da tensão
da placa areolopapilar, resultados duradouros e alto grau de satisfação das
pacientes.
Palavras-chave: Implantes de mama; Mamoplastia; Atrofia; Prevenção secundária; Procedimentos cirúrgicos reconstrutivos
INTRODUCTION
Combined mastopexy with implant placement would appear to be simple, but is in fact an architecturally challenging intervention, with technical difficulties, risks, and non-durable results1.
There has been no consensus regarding ideal technique1-3, with reported postsurgical revision rates reaching 54%4-6.
The surgery has been performed in patients with inverted T mastopexy with prostheses who develop ptosis relapse (grade III and IV) with prosthesis displacement. We present a variation of the mirror “D” technique7 with long-lasting results and a high degree of patient satisfaction.
The changes described include the form of marking, positioning of the patient during surgery, and surgical techniques. The mirror “D” technique consists of combined resection of skin and breast parenchyma, use of a medial pedicle8, a new submuscular prosthesis9,10, and a vertical scar11.
OBJECTIVE
To provide lasting results and reduce the rate of recurrence of ptosis with prosthesis displacement.
METHODS
Results obtained with the mirror “D” technique for secondary mastopexy with replacement of prostheses were evaluated in 90 female patients aged 30-60 years old, with no exclusion by race, between July 2013 and July 2015 and living in the city of São Paulo, Vale do Paraíba and the north coast. Surgery was performed by the author at the Hospital Antoninho da Rocha Marmo in São José dos Campos, SP, with the approval of the Ethics Committee of the hospital and with signed informed consent, according to the principles of the Declaration of Helsinki (001/ADM/HARM/2018).
Patients had undergone inverted T mastopexy with subglandular prostheses and complained of grade III and IV ptosis relapse with prosthesis displacement, with or without capsular contracture and/or unsightly scarring. The patients were evaluated weekly during the first month, then monthly for 6 months, then every 3 months for 2 years following surgery.
RESULTS
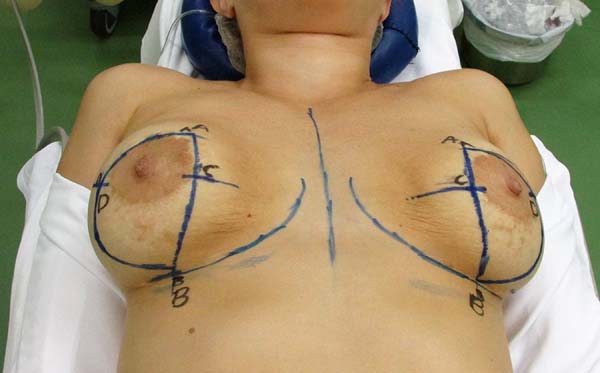
Marking
Marking is performed in supine position with arms next to the trunk (Figure 1); this position accentuates the mammary groove up to 1 cm more compared with marking in upright position.
When properly positioned, a midline incision is marked from the sternal notch to the umbilicus.
The groove formed naturally by the positioning of the breasts in decubitus position is marked.
According to the position naturally adopted by the breasts, point A is marked 9 cm from the midline and 10 cm from the inframammary groove.
According to the groove naturally formed in decubitus position, point B is marked at the level of the groove, 10 cm from the midline. Point C is marked 6 cm from the inframammary groove by following the junction line from point A to point B. Using a bidigital block maneuver, point D is marked according to the maximum extent of skin resection.
>Closure in mirror “D” technique is performed by the linear apposition of points A and B and an arc extended laterally from point A to point B through D, including the areola superiorly, according to the limits of point D for inferior continuation of the arc. The junction of points C and D at the end of surgery will coincide with the location of the lower edge of the new position of the areola and beginning of the vertical scar. This is found approximately 6 cm from the groove marked at the beginning, while point B guides the end of the vertical scar.
Technique
Schwartzman Maneuver: Surgery begins with marking of the areola with a 4 cm areolotome, followed by decortication of skin over the tissue that gives rise to the medial pedicle flap;
Preparation of the medial flap: The medial flap is marked with a 5-cm base, measuring at least 1 cm around the areola. The tissue is removed by maintaining a thickness of at least 2 cm from the lateral edge to the base of the flap8.
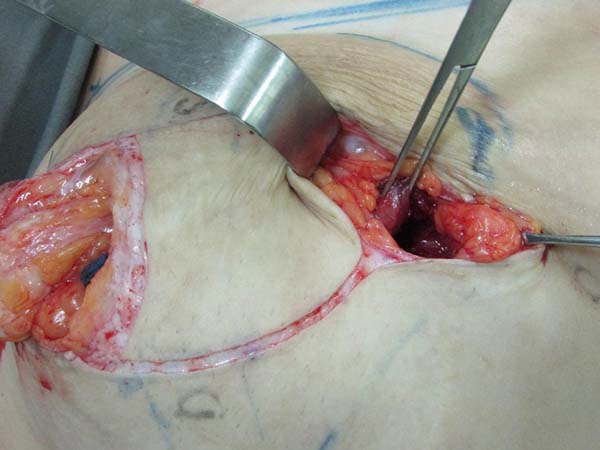
Preparation of the submuscular pocket: Marking is performed to the level of subcutaneous tissue. Inferior periareolar mammotomy is performed to remove the prosthesis. A new submuscular inframammary pocket is created at the level of point B (Figure 2). The anatomical limits of the submuscular pocket are: clavicle superiorly at 2 cm from the medial line, not exceeding the anterior axillary line laterally, and inferiorly up to the mammary groove, partially releasing the tendon insertion in the inferior medial direction.
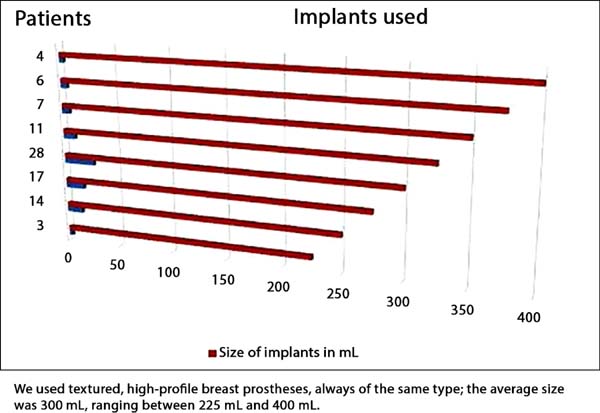
Placement of the prosthesis: The mammary parenchyma underlying the marking protects the muscle to avoid disruption during placement of prostheses. We use textured, high-profile, round silicone implants, with volumes varying from 225 to 400 mL (Figure 3).
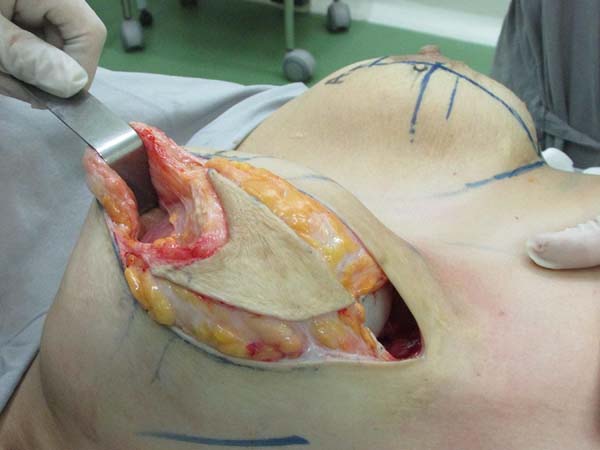
Resection for symmetrization: Pulling the flap superiorly, a line is drawn parallel to the midline, coinciding with the A-B line; an incision is made perpendicular to the muscle (Figure 4). The lateral portion of the breast is freed in the lateral direction, on the projection of a D arc. Once the lateral portion is released, the flap is pulled along a vector directed toward the notch (superomedially), followed by resection of tissue that exceeds the projection of the incision in AB (Figure 5 and 6). After resection of the parenchyma, the lateral muscular support of the prosthesis becomes apparent, preventing communication with the previous subglandular pocket; severe atrophy of the tissues in these cases is also evident (Figure 7).
Capsulotomy or capsulectomy: In grade I and II capsular contracture, capsulotomy is performed (Figure 8) with radiating incisions until the mammary parenchyma is reached. Capsulectomy is used in grades III and IV contracture.
Sutures: Closure of muscle is performed with nylon 2.0, and mammary parenchyma is sutured with inferomedial traction on the lateral parenchyma for medialization, thus approaching the medial and lateral pillars with inverted nylon 2.0 sutures. Sutures are placed to join pillars and muscle at each point (Figure 9). Suturing is performed in planes and the final closure of the skin is performed with inverted colorless nylon 4.0.
Marking of Areola: The junction of points C and D (Figure 10) coincides with the location of the bottom edge of the new position of the areola and beginning of the vertical scar, and is found approximately 6 cm from the groove marked in the beginning, while point B guides the end of the vertical scar.
Portovac drain is placed: For drainage of the subglandular pocket.
Dressing: Is performed with Micropore tape crisscrossing directly on the scar, and is maintained for 10 days (Figure 11).
RESULTS
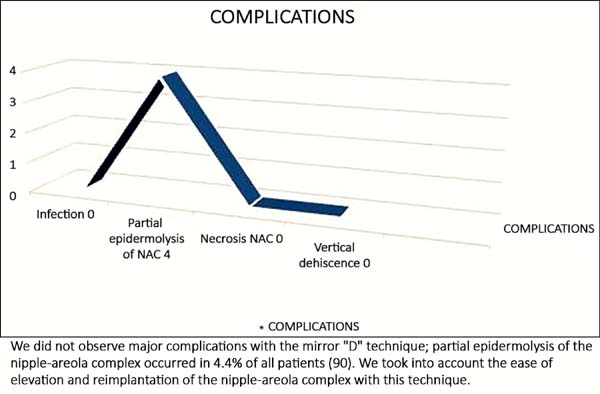
No surgical revision was required in any of the cases. There was no postsurgical infection or necrosis of the nipple-areolar complex or scar (Figures 12 to 20).
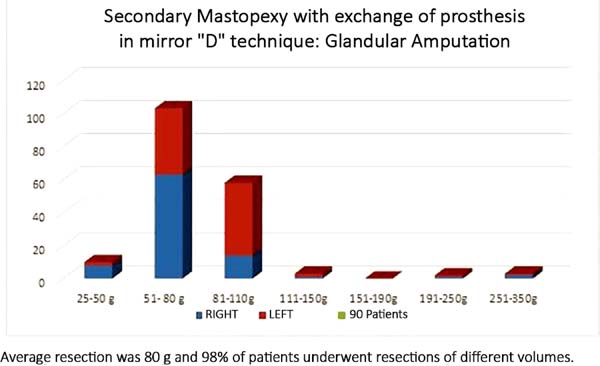
The average resection of the parenchyma measured 80 g, ranging from 25 g to 350 g (Figure 21). Resection of different volumes was performed in 98% of cases, with an average difference between breasts of 50 g, ranging from 20 to 200 g.
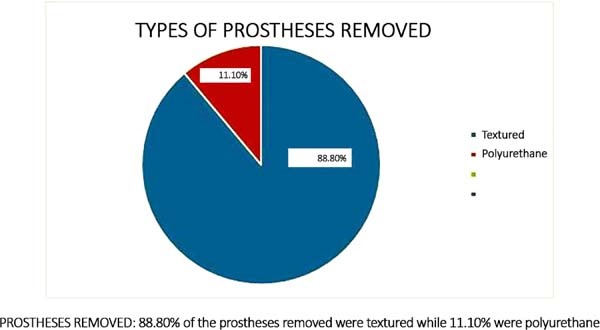
The prostheses removed in 80 patients (88.8%) were textured, and were polyurethane covered in 10 patients (11.1%); volumes ranged between 200 and 460 mL (Figure 22).
The average new standard commercial prosthesis volume was 300 mL, ranging between 225 and 400 mL; prostheses were textured and round, with high profile (Figure 23).
The average final breast volume increase (mean of breast implant volume subtracted from mean dry volume) was 250 g (textured silicone, high profile, round, 200 mL = 200 g). The length of the vertical scar was stable with time, measuring 6.0 cm in the immediate postoperative period and averaging 6.5 cm after 2 years.
Four (4.4%) cases of partial epidermolysis of the nipple-areolar complex were successfully treated with conservative measures (dressing with alginate hydrogel) (Figure 24).
Patients who underwent the mirror “D” technique rated their results at two different time points using predetermined criteria (Tables 1 and 2).
| After 6 months | Poor | Fair | Good | Excellent | Total | ||||
|---|---|---|---|---|---|---|---|---|---|
| Quality of scar | __ | __ | 6 | 6.6% | 18 | 20% | 66 | 73.3% | 90-100% |
| Aesthetic format | __ | __ | 3 | 3.3% | 22 | 24.4% | 65 | 72.2% | 90-100% |
| Symmetry | __ | __ | 4 | 4.4% | 24 | 26.6% | 62 | 68.8% | 90-100% |
| Total | |||||||||
| After 24 months | Poor | Fair | Good | Excellent | Total | ||||
|---|---|---|---|---|---|---|---|---|---|
| Quality of scar | __ | __ | 2 | 2.2% | 25 | 27.7% | 63 | 70% | 90-100% |
| Aesthetic format | __ | __ | 1 | 1.1% | 33 | 36.6% | 56 | 62.2% | 90-100% |
| Symmetry | __ | __ | 4 | 4.4% | 34 | 37.7% | 52 | 57.7% | 90-100% |
| Total | |||||||||
DISCUSSION
This variation of the mirror “D” technique was used in 90 patients, with a high degree of satisfaction.
The mirror “D” technique uses specific markings with the patient in dorsal decubitus and arms next to the trunk. This position accentuates the mammary groove up to 1 cm more compared with marking in upright position, resulting in a more suitable format and natural final result, while facilitating placement of the prosthesis in the submuscular plane.
In this position, the breasts naturally assume symmetric spatial adjustment that is easily visualized in the positioning of the nipple-areola complex (NAC). This cancels the asymmetry induced by gravity that is seen in upright position, resulting in naturally symmetrical breasts in the postoperative period9,12,13.
These patients present with severe tissue atrophy14-16 (skin, parenchyma, muscle), requiring small changes in the preparation of the submuscular pocket that now includes an inframammary opening (previously at the level of the second costal arch in the midclavicular line), in addition to preservation of the parenchyma (resection prior to placement of the prosthesis); we avoid any communication with the old pocket, providing improved lateral support of the prosthesis, and thus, avoiding lateralization.
After resection and closure of the parenchyma, the mirror “D” marking technique along with the submuscular breast prosthesis provide symmetrical, medialized breasts without tension on the NAC, and with parallel vertical scars (with a difference of 1 cm between point A and B); the results have a high rate of patient satisfaction.
CONCLUSION
The mirror “D” technique is a good option in secondary mastopexy, resulting in correction despite the increased complexity of the desired results caused by severe atrophy of tissues in these patients4,7,15 as a result of previous surgery. The benefits include symmetrical breasts, parallel vertical scars, decreased tension on the NAC, lasting results, and a high degree of patient satisfaction.
REFERENCES
1. Spear SL. Augmentation/mastopexy: "surgeon, beware". Plast Reconstr Surg. 2006;118(7 Suppl):133S-4S.
2. Spear SL, Low M, Ducic I. Revision augmentation mastopexy: indications, operations, and outcomes. Ann Plast Surg. 2003;51(6):540-6. PMID: 14646644 DOI: http://dx.doi.org/10.1097/01.sap.0000096450.04443.be
3. Stevens WG, Freeman ME, Stoker DA, Quardt SM, Cohen R, Hirsch EM One-stage mastopexy with breast augmentation: a review of 321 patients. Plast Reconstr Surg. 2007;120(6):1674-9. DOI: http://dx.doi.org/10.1097/01.prs.0000282726.29350.ba
4. Spear SL, Pelletiere CV, Menon N. One-stage augmentation combined with mastopexy: aesthetic results and patient satisfaction. Aesthetic Plast Surg. 2004;28(5):259-67. DOI: http://dx.doi.org/10.1007/s00266-004-0032-6
5. Cárdenas-Camarena L, Ramírez-Macías R; International Confederation for Plastic Reconstructive and Aesthetic Surgery; International Society of Aesthetic Plastic Surgery; Iberolatinoamerican Plastic Surgery Federation; Mexican Association of Plastic Esthetic and Reconstructive Surgery; Western Mexican Association of Plastic, Esthetic and Reconstructive Surgery; Jalisco College of Plastic Surgeons. Augmentation/mastopexy: how to select and perform the proper technique. Aesthetic Plast Surg. 2006;30(1):21-33. DOI: http://dx.doi.org/10.1007/s00266-005-0133-x
6. Spear SL, Boehmler JH 4th, Clemens MW. Augmentation/mastopexy: a 3-year review of a single surgeon's practice. Plast Reconstr Surg. 2006;118(7 Suppl):136S-47S.
7. Sanchéz J, Carvalho AC, Erazo P. Mastopexia com prótese: técnica em "D" espelhado. Rev Bras Cir Plást. 2008;23(3):200-6.
8. Wada A, Millan LS, Gallafrio ST, Gemperli R, Ferreira MC. Tratamento da ptose mamária e hipomastia utilizando técnica de mamoplastia com pedículo súpero-medial e implante mamário. Rev Bras Cir Plást. 2012;27(4):576-83. DOI: http://dx.doi.org/10.1590/S1983-51752012000400018
9. Biggs TM, Yarish RS. Augmentation mammaplasty: retropectoral versus retromammary implantation. Clin Plast Surg.1988;15(4):549-55. PMID: 3224480
10. Daher JC, Amaral JDLG, Pedroso DB, Cintra Júnior R, Borgatto MS. Mastopexia associada a implante de silicone submuscular ou subglandular: sistematização das escolhas e dificuldades. Rev Bras Cir Plást. 2012;27(2):294-300. DOI: http://dx.doi.org/10.1590/S1983-51752012000200021
11. Persoff MM. Vertical mastopexy with expansion augmentation. Aesthetic Plast Surg. 2003;27(1):13-9. DOI: http://dx.doi.org/10.1007/s00266-002-0072-8
12. Pitanguy I. A new technic of plastic surgery of the breast. Study of 245 consecutive cases and presentation of a personal technic. Ann Chir Plast. 1962:199-208. PMID: 13943809 DOI: http://dx.doi.org/10.1097/00006534-196211000-00023
13. Almeida ARH, Araújo GKM, Mafra AVC, Pimenta PS, Fabrini HS. Mastoplastia de aumento com inclusão de implante de silicone associado a mastopexia com abordagem inicial periareolar (safety pocket). Rev Bras Cir Plást. 2012;27(4):569-75. DOI: http://dx.doi.org/10.1590/S1983-51752012000400017
14. Soares AB, Franco FF, Rosim ET, Renó BA, Hachmann JOPA, Guidi MC, et al. Mastopexia com uso de implantes associados a retalho de músculo peitoral maior: técnica utilizada na Disciplina de Cirurgia Plástica da Unicamp. Rev Bras Cir Plást. 2011;26(4):659-63. DOI: http://dx.doi.org/10.1590/S1983-51752011000400021
15. Valente DS, Carvalho LA, Zanella RK. Mastopexia crescente com implantes de silicone: um estudo longitudinal prospectivo. Rev Bras Cir Plást. 2012;27(4):584-7. DOI: http://dx.doi.org/10.1590/S1983-51752012000400019
16. Pessoa MCM, Accorsi Jr. J, Ribeiro L, Moreira LF. Mastopexia com implantes: uso sistemático dos retalhos de base inferior de Ribeiro. Rev Bras Cir Plást. 2013;28(3):333-42.
1. Sociedade Brasileira de Cirurgia Plástica, São
Paulo, SP, Brazil.
2. Clínica Juan Sánchez, São José dos Campos, SP,
Brazil.
3. Universidade Federal de São Paulo, Escola
Paulista de Medicina, São José dos Campos, SP, Brazil.
4. Clínica Dra. Patrícia Erazo, São Paulo, SP,
Brazil.
5. Universidade Santa Cecília, São Paulo, SP,
Brazil.
Corresponding author: Juan Carlos Sánchez López, Rua Santa Clara, 1035 - Vila Icaraí - São José dos Campos, SP, Brazil. Zip Code 12243-630. E-mail: comercial@drjuan.com.br
Article received: August 25, 2017.
Article accepted: September 5, 2018.
Conflicts of interest: none.











































 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter