

Original Article - Year 2018 - Volume 33 -
Total lower eyelid reconstruction with the combined use of the Hughes and Destro flaps
Reconstrução total de pálpebra inferior com associação dos retalhos de Hughes e Destro
ABSTRACT
Introduction: Lower eyelid cancers are common. Basal
cell carcinoma, squamous cell carcinoma, and melanoma
are responsible for 5 to 10% of all skin cancers. Complete
reconstruction after excision of a tumor that creates a defect
involving more than 50% of the eyelid is a challenge. Reports
vary regarding the best method of reconstruction, and most
available literature is in the form of case reports, leading
to inconsistency in the evidence presented.
Methods: This
retrospective study examined the medical records to evaluate
the functional results achieved by the author in patients who
underwent total lower eyelid reconstruction after cancer
resection between May 2012 and May 2016. The Hughes
myotarsoconjunctival flap was used for reconstruction of the
internal lamella, and the Destro VY skin advancement flap was
used for the external lamella.
Results: Of 13 patients with a
mean age of 72.61 years, basal cell carcinoma accounted for 11
cases. No comorbidity was observed in the flap donor areas.
Contralateral symmetry and palpebral closure were achieved
in 12 cases; 1 case of ectropion was successfully treated, but
no other functional problems were identified.
Conclusion:
The combined use of the Hughes flap and Destro flap is a
valuable alternative for total reconstruction of the lower
eyelid and can achieve favorable functional and aesthetic
outcomes with donor tissue, similar to that of resected tissue.
Keywords: Reconstructive surgical procedures; Eyelids; Surgical flaps; Eyelid neoplasms
RESUMO
Introdução: A neoplasia de pálpebra inferior é uma doença frequente. O carcinoma
basocelular, o espinocelular e o melanoma são responsáveis por 5 a 10% de
todos os cânceres de pele. A reconstrução total da pálpebra inferior após
exérese de neoplasia cujo defeito envolva mais que 50% da pálpebra é um
desafio. A literatura mostra alternativas discordantes quanto ao melhor
método de reconstrução nessas situações, sendo a maioria dos trabalhos
composta por relatos de casos, levando à inconsistência nas evidências
apresentadas.
Método: Avaliar retrospectivamente, por meio da coleta de dados em prontuários, os
resultados funcionais alcançados pelo autor nos pacientes submetidos à
reconstrução total de pálpebra inferior após ressecção de neoplasia entre
maio de 2012 e maio de 2016, na Santa Casa de Passos, com a associação do
retalho miotarsoconjuntival de Hughes para reconstrução da lamela interna e
do retalho de avanço de pele VY de Destro para reconstituir a lamela
externa.
Resultados: Foram operados 13 pacientes, com média de idade de 72,61 anos. O carcinoma
basocelular foi responsável pela maioria das lesões com 11 casos. Nenhum
paciente apresentou comorbidade nas áreas doadoras dos retalhos. A simetria
contralateral e o fechamento palpebral foram observados em 12 casos, sendo
um caso de ectrópio tratado com sucesso, não sendo identificados outros
problemas funcionais.
Conclusão: A associação do retalho miotarsoconjuntival de Hughes e retalho de Destro é
uma alternativa valiosa para a reconstrução total da pálpebra inferior,
visto conseguirmos um resultado funcional e estético favorável com tecidos
doadores semelhantes aos ressecados.
Palavras-chave: Procedimentos cirúrgicos reconstrutivos; Pálpebras; Retalhos cirúrgicos; Neoplasias palpebrais
INTRODUCTION
The eyelid is a common site of cancer. Skin cancer of the eyelids, including basal cell carcinoma, squamous cell carcinoma, and melanoma, accounts for 5 to 10% of all skin cancers, with 95% comprising basal cell carcinomas or squamous cell carcinoma1,2. Reconstruction of the lower eyelid after excision for cancer or trauma is a challenge. Numerous options are possible depending on the extent of the defect3.
Plastic surgery seeks to repair and restore the protective function of the eyelid, preferably using techniques that also provide good aesthetic results4. The surgical anatomy that guides reconstruction planning divides the eyelid into 3 lamellae: anterior, middle, and posterior. The anterior lamella is composed of the skin and orbicularis oculi. The middle lamella is defined as the combined orbital septum, adipose orbital tissue, and submuscular fibroadipose tissue. The posterior lamella includes the fascia of the lower eyelid, the tarsus, and the connective tunica of the eyelid5.
Eyelid defects are classified as 2 types, according to the affected structures: partial, when the posterior lamella is preserved, and total, when all lamellae are compromised6. In full-thickness defects, it is necessary to restore the 2 lamellae and the eyelid support, a function naturally performed by the tarsus, which is composed of dense connective tissue, devoid of cartilage7. In these cases, at least 1 of the reconstructed lamellae needs vascular support.
Common and reliable surgical techniques involve patch and graft options. Thus, an algorithm for reconstruction of full-thickness defects of the lower eyelid assists in the choice of the type of reconstruction to be performed. Defects smaller than 25% of the eyelid margin can be treated with primary suturing. Cantholysis and canthotomy allow primary closure of defects comprising 25 to 50% of the palpebral margin.
Tenzel’s semicircular flap combined with a periosteal flap or palatal mucosal graft, with atrial or septal cartilage for the posterior lamella, is used to repair defects of 50 to 75%. Lesions that require extensive resection of 50 to 100% of the palpebral margin are more satisfactorily treated with a tarsoconjunctival flap of the upper eyelid for the internal lamella and a forward flap or total skin graft for the anterior lamella8.
The literature reports discordant alternatives as to the best method of reconstruction for the lower eyelid internal lamella when primary suturing is impossible. The vast majority of studies comprise case reports or small patient samples, leading to inconsistency in the evidence presented9.
This study evaluated cases of lower eyelid cancer that left a defect of more than 50% of the eyelid and were reconstructed with the combined use of 2 flaps for the reconstitution of the anterior and posterior lamellae.
OBJECTIVE
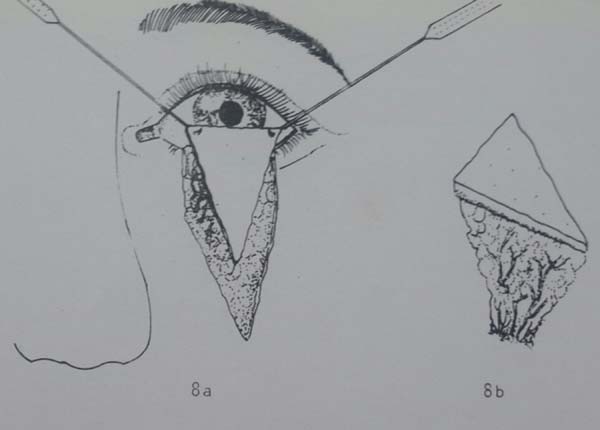
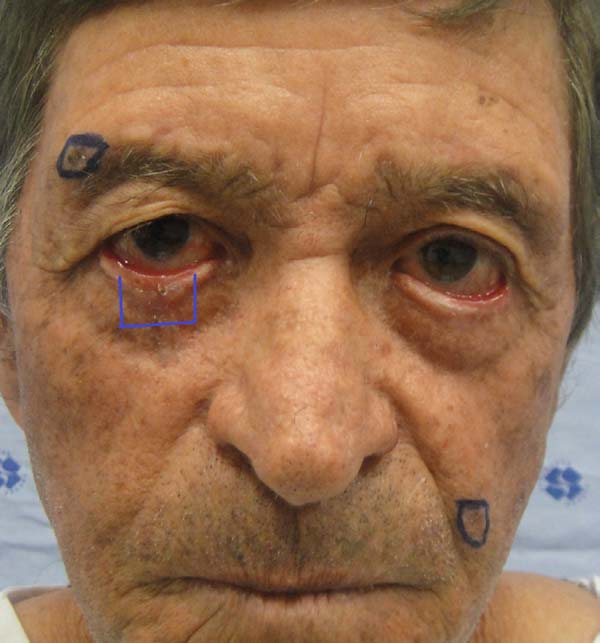
To evaluate the results of the Hughes myotarsoconjunctival flap (Figure 1) for reconstruction of the internal lamella combined with the VY Destro skin flap (Figure 2) for reconstruction of the external lamella in defects caused by resection of lower eyelid cancer.
METHODS
This retrospective study of medical records included 13 patients who underwent total reconstruction of the lower eyelid by the author after resection of cancer between May 2012 and May 2016 at Santa Casa de Misericórdia de Passos, MG. When the defect involved the total plane of the lower eyelid and horizontal extension greater than 50%, the eyelid was reconstructed using the Hughes myotarsoconjunctival flap10 to recreate the posterior lamella; a triangular flap of skin with a subcutaneous Destro pedicle was used to reconstruct the anterior lamella11.
Data collected included age, sex, histological tumor type, comorbidities, surgical time, flap transection time, complications, and follow-up duration.
The results were evaluated using the following parameters: 1) palpebral occlusion capacity; 2) signs of ectropion; 3) symmetry; and 4) morbidity of the flap donor area.
All cases were performed by the author with the same assistant, and all were performed under local anesthesia (lidocaine 2% with epinephrine 1:200,000) and topical corneal anesthesia combined with intravenous sedation. One case was performed with general intravenous anesthesia. Brush marking of tumor margins of 3 to 5 mm was performed. After antisepsis of the entire face and anesthesia, the lesion was resected and sent immediately for frozen analysis and determination of safety margins. After confirming margins free of cancer, surgery proceeded.
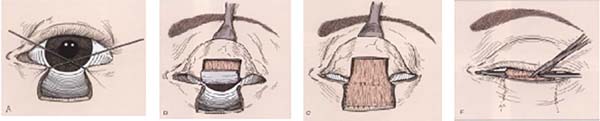
For the Hughes flap, eyelid eversion was performed with a repair point at the eyelid edge or with use of a retractor and forceps cable as a support. The myotarsoconjunctival flap was designed so that the distal incision was 4 mm from the palpebral margin (being parallel to the margin to ensure the stability and contour of the upper eyelid) and the medial and lateral extension was sufficient to reach and reconstruct the posterior lamella. On average, the height of the dissected tarsus was 4 to 6 mm and was slightly smaller than the size of the defect.
Infiltration of the everted subconjunctival upper eyelid was performed with 1 ml of local anesthetic. An incision was made on the flap using a number 15 blade, and the flap was dissected with blunt scissors in the subtarsal plane to the plane of the levator muscle of the upper eyelid; this dissection was continued superiorly until the flap could be advanced to the inferior defect without tension. The flap was sutured with Vicryl® 6.0 in a continuous line to the lower palpebral conjunctiva, just above the fundus of the palpebral sac and extending to the palpebral ridge, thus, repairing the posterior lamella.
To repair the anterior lamella with the Destro flap, methylene blue was used to demarcate a “V” flap that began at the lower ends of the defect with a vertical line slightly longer than the height of the defect, descending and converging toward the malar region. The central subcutaneous pedicle of the inverted cone-shaped flap was delicately dissected by separating loose subcutaneous tissue and preserving the vessels, in a dissection designed to taper the pedicle that progressed to the muscular plane.
The larger the desired displacement, we ensured that the more tapered and longer was the pedicle. We advanced the triangular flap on the myotarsoconjunctival flap by sliding to cover the raw area. The first 2 points were attached with Mononylon® 5.0, reaching the bilateral conjunctival ridge 2 mm below the 2 upper angles of the flap, with some points attached with Vicryl 6.0. The fasciocutaneous triangular flap was attached to the superior tarsus, which was reflected 1 mm above the residual lower palpebral margin to avoid inferior retraction (Figures 3 to 9).
Transection of the flap was performed after 3 to 4 weeks under local anesthesia using a tentacan support for corneal protection (Figure 10). Hemostasis was performed at the upper border of the flap, with thinning of excess tissue and healing by second intention. In some cases, Vicryl 6.0 simple stitches were used to regularize the collar.
This study adhered to the principles of the Declaration of Helsinki revised in 2000 and Resolution 196/96 of the National Health Council. The patients signed a Free and Informed Consent Form, allowing the use of their data and the publication of their photos (CAAE:69519617.7.0000.8043).
RESULTS
Thirteen patients (6 women and 7 men) were operated on over 4 years. All were Caucasian. Ages ranged from 55 to 89 years with a mean of 72.61 years. Basal cell carcinoma accounted for 11 cases (84.61%), with 1 case of squamous cell carcinoma and 1 case of Merkel cell carcinoma. The surgical time averaged 75.76 minutes (for the first stage of reconstruction). Myotarsoconjunctival flap transection was performed from 19 to 39 days after the first surgery, with a mean of 28 days. The follow-up duration was at least 12 months. During this period there were no cases of local recurrence (Table 1).
| Age (years) | Sex | Etiology | Surgical time (min) | Transection (days) | Complications | Resolution |
|---|---|---|---|---|---|---|
| 56 | F | BCC | 60 | 26 | ||
| 55 | M | BCC | 110 | 30 | ||
| 86 | F | BCC | 75 | 21 | ||
| 83 | F | BCC | 40 | 21 | ||
| 58 | M | BCC | 95 | 19 | Ectopic mucosa on the palpebral border | Upper eyelid skin graft |
| 80 | F | BCC | 75 | 39 | ||
| 59 | M | Merkel | 135 | 36 | Edema with conjunctival irritation | Massage |
| 77 | M | BCC | 130 | 39 | ||
| 89 | F | BCC | 45 | 28 | ||
| 83 | M | BCC | 40 | 22 | ||
| 61 | F | BCC | 60 | 23 | ||
| 85 | M | SCC | 75 | 32 | ||
| 72 | M | BCC | 120 | 28 | Ectropion | Fricke flap |
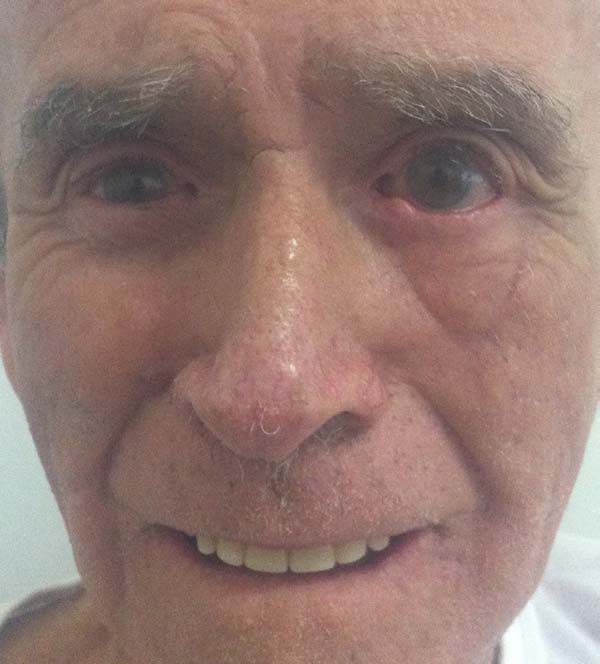
According to the criteria established by the study, no patient had comorbidity at the flap donor area. One patient with an extensive tumor developed early conjunctival irritation due to edema that caused the skin of the flap to contact and irritate the conjunctiva. With massage, she had spontaneous resolution at 4 months and regression of edema (Figures 11 to 13).
Another patient developed ciliary border hyperemia caused by ectopic conjunctival mucosa beyond the eyelid border, despite having a regular eyelid border without ectropion at the level of the limbus. This was corrected after 24 months with a thin skin graft of the ipsilateral upper eyelid (Figures 14 to 17). The last operated case had a severe ectropion, which was successfully corrected 3 months later with a Fricke flap of the upper eyelid (Figures 18 to 21). Contralateral symmetry and palpebral closure were observed in all cases at the end of treatment, and no other functional problems were identified in any of the patients.
DISCUSSION
Reconstruction of large defects of the lower eyelid is a challenge for restorative surgery. Different techniques have been described, including those by Mustardé12, the use of Hughes flap with modifications and advances13, the use of hard palate graft covered by orbicularis muscle advancement14, the use of the Tripier flap15, and other more complex approaches, such as the use of pre-expanded lingual mucosal flap16, the use of acellular dermal matrix17, the use of cheek flap supported by the fascia lata18, and the use of the superior orbicularis muscle flap combined with the island tarsoconjunctival19 and Fricke flap20,21. All these techniques are useful when lower eyelid reconstruction is necessary; however, some are complex and expensive3.
To achieve excellent functional and aesthetic results, the 2 layers of the lower eyelid must be adequately reconstructed, bearing in mind that the use of a graft on a lamella requires the use of a flap in the other. When a flap is used on a lamella, an option is rebuilding of the other flap with a flap or graft. Once this is done, the vascular supply is guaranteed, as is the integration of the reconstruction13.
In the present study, we used the triangular flap of the subcutaneous pedicle to reconstruct the anterior lamella. We believe that a flap of the same aesthetic unit is the best option because it has color and thickness similar to that of the resected area11,22. A skin graft, either from the upper eyelid or retroauricular region, is also an option; however, the graft must be removed from another surgical region and requires a flap to the internal lamella to vascularize the graft.
The internal lamella can be reconstructed with the use of a nasal septal chondromucosal graft12,22,23, ear cartilage (Destro’s preference)24,25, or hard palate mucosa14. However, these grafts are unstable in large resections due to the lack of remaining eyelid support, which makes them difficult to attach, and necessitates the use of extensive skin flaps to rework the external lamella26; however, these may impair adherence to the graft due to excessive thickness.
To reconstruct the internal lamella, we used a myotarsoconjunctival flap. This alternative provides more stability and support for lateral, medial, and inferior attachment to the remaining lower eyelid, in addition to being well vascularized.
Mustardé opposed the use of the upper eyelid for reconstruction of the lower eyelid due to the possibility of upper palpebral retraction leading to corneal exposure. This would be of concern if we consider the original work of Hughes in 1937, in which an incision was made in the gray line with total division of the upper eyelid, leaving it with reduced support and susceptible to postoperative retraction.
The main problem with the original technique was, therefore, frequent morbidity in the donor area, with retraction and entropion after division of the pedicle. To avoid this complication, some authors27-29 modified the original Hughes technique to preserve the tarsus and reduce its inclusion in the flap. In this modification, which we used in our patients, the lower horizontal border of the Hughes flap should be at least 4 mm from the eyelid margin, so that a tarsal plaque remains in the donor site of the upper eyelid, avoiding postoperative deformity. There is no justification for not using this excellent flap in lesions larger than 50% because is safe to use in terms of vascularity and provides support for external lamellar apposition, which is a factor in stability and reconstruction of the eyelid9.
One difficulty presented by this Hughes flap option occurs when the eye with the affected eyelid is the single source of vision, making it difficult to use flaps within the same aesthetic unit. Another negative point is the need for a second operation 3 weeks later for transection of the Hughes flap and opening of the eyelid cleft13.
Hughes performed transection of the myotarsoconjunctival flap pedicle after 3 months10. Cies and Bartlett30 reported dividing the patch at 3 and 4 weeks without complications, and McCord and Nunery28 waited 6 to 8 weeks before the split. Leibovitch et al.31 divided the flap in 7 days and found that this did not compromise the blood supply, with good aesthetic and functional results even after early flap splitting. In our patients, the objective was to perform transection after 3 weeks on average, but this period varied due to external and individual factors, which in our analysis did not alter the results; the mean transection was performed at 28 days.
One of our first patients (Figures 15 to 17) developed hyperemia of the palpebral margin after division of the pedicle in the second surgical stage. We attributed this hyperemia to use of simple Vicryl 6.0 suturing at the palpebral border after transection; this led to advancement of the mucosa on the new palpebral border and an excellent functional result; however, posterior aesthetic correction was required, and was performed with a thin skin graft of the upper eyelid 2 years later, achieving an excellent result.
Bartley and Putterman32 regularized the border after transfection of the flap and allowed spontaneous granulation to occur. This allowed the mucocutaneous junction to be formed by second intention and to avoid postoperative hyperemia. Thus, this technique was performed in the rest of the patients and hyperemia was not observed again.
More extensive lesions present more pronounced postoperative edema, which can lead to eye discomfort and irritation. In these patients, postoperative massage or lymphatic drainage can help with resolution (Figures 11 to 13)
We attributed a postoperative ectropion in the last patient (Figures 18 to 21) to the sagging and poor elasticity of malar skin that we underestimated by using a flap to reconstruct the anterior lamella. We believe that, in this case, Destro fasciocutaneous flap was not a good choice for reconstruction of the anterior lamella after rotating the Hugues flap.
Other alternatives, such as a Mustardé flap, or even skin grafting of the contralateral or retroauricular upper eyelid on the myotarsoconjunctival flap, should be considered if lateral facial flaccidity is present. In these cases, full-thickness skin grafts are considered for reconstruction of the anterior lamella33, and are preferred by many authors34. In this well-known complication with use of a Fricke flap, care should be taken to evaluate the elasticity of facial skin before choosing a VY flap, since inadequate elasticity of the skin of the malar region may lead to inferior retraction of the reconstituted palpebral ridge.
The average surgical time was 74.61 minutes and was considered rapid for this procedure. In 3 cases, the surgery was prolonged because the frozen margin required extension; this did not affect the results, given the importance of performing total excision of the tumor.
All patients were followed for at least 12 months by plastic surgery, with satisfactory outcomes; 2 cases developed complications, but were treated. During this period, there were no lesion recurrences and patients were followed up by clinical oncology.
CONCLUSION
Lower palpebral reconstruction is a challenge for the plastic surgery specialist who has several available techniques. The combined use of the Hughes myotarsoconjunctival flap and a Destro flap is a valuable alternative to complete reconstruction of the lower eyelid, as it achieves a favorable functional and aesthetic result, enabling major reconstruction options after cancer resection of the entire lower eyelid plane.
REFERENCES
1. Cook BE Jr, Bartley GB. Treatment options and future prospects for the management of eyelid malignancies: an evidence-based update. Ophthalmology. 2001;108(11):2088-98. DOI: http://dx.doi.org/10.1016/S0161-6420(01)00796-5
2. Abraham JC, Jabaley ME, Hoopes JE. Basal cell carcinoma of the medial canthal region. Am J Surg. 1973;126(4):492-5. PMID: 4582802 DOI: http://dx.doi.org/10.1016/S0002-9610(73)80036-4
3. Panse N, Sambhus M, Sahasrabudhe P, Deodhar A. The Tarsoconjunctival Flap for Lower Lid Reconstruction-Review of Literature and Case Series. J Clin Exp Ophthalmol. 2013;4(2):271. DOI: http://dx.doi.org/10.4172/2155-9570.1000271
4. Mélega JM, Viterbo F, Mendes FH. Cirurgia plástica: os princípios e a atualidade. Rio de Janeiro: Guanabara Koogan; 2011. p. 573-4.
5. Kakizaki H, Malhotra R, Madge SN, Selva D. Lower eyelid anatomy: an update. Ann Plast Surg. 2009;63(3):344-51.
6. Newman MI, Spinelli HM. Reconstruction of the eyelids, correction of ptosis, and canthoplasty. In: Thorne CH, ed. Grabb and Smith's Plastic Surgery. 7th ed. Philadelphia: Lippincott Williams & Wilkins; 2007. p. 397-416.
7. Alves JCRR, Liu RP, Silva Filho AF, Pereira NA, Carvalho EES. Reconstrução palpebral com enxerto de cartilagem autóloga de concha de orelha. Rev Bras Cir Plást. 2012;27(2):243- 8.
8. Fante RG. Reconstruction of the eyelids. In: Baker SR. Local Flaps in Facial Reconstruction. Philadelphia: Elsevier; 2007. p. 387-412.
9. Maniglia RF. Uso do retalho tarso conjuntival para reconstrução da lamela interna da pálpebra inferior [Dissertação de mestrado]. São Paulo: Faculdade de Ciências Médicas da Santa Casa de São Paulo; 2008.
10. Hughes WL. A new method for rebuilding a lower lid: report of a case. Arch Ophthalmol. 1937;17(6):1008-17.
11. Destro MW. Retalhos triangulares de pele com pedículo subcutâneo central na reconstrução da pálpebra inferior [Tese de doutorado]. Belo Horizonte: Universidade Federal de Minas Gerais, Faculdade de Medicina; 1990.
12. Mustarde JC. Repair and reconstruction of the orbital region. 2nd ed. Edinburgh: Churchill Livingstone; 1980.
13. Rohrich RJ, Zbar RI. The evolution of the Hughes Tarsoconjunctival flap for the lower eyelid reconstruction. Plast Reconstr Surg. 1999;104(2):518-22.
14. Lalonde DH, Osei-Tutu KB. Functional reconstruction of unilateral, subtotal, full-thickness upper and lower eyelid defects with a single hard palate graft covered with advancement orbicularis myocutaneous flaps. Plast Reconstr Surg. 2005;115(6):1696-700. PMID: 15861077
15. Tripier L. Lambeau músculocutané en forme de pont. Appliqué a la restauration de paupieres. Gaz Hop (Paris). 1889;62:1124-5.
16. Miyawaki T, Hisako A, Suzuki H, Kurihara K, Jackson IT. Pre-expansion of mucosa-lined flap for lower eyelid reconstruction. Plast Reconstr Surg. 2005;116(5):76e-82e.
17. Li TG, Shorr N, Goldberg RA. Comparison of the efficacy of hard palate grafts with acellular human dermis grafts in lower eyelid surgery. Plast Reconstr Surg. 2005;116(3):873-8.
18. Matsumoto K, Nakanishi H, Urano Y, Kubo Y, Nagae H. Lower eyelid reconstruction with a cheek flap supported by fascia lata. Plast Reconstr Surg. 1999;103(6):1650-4. PMID: 10323697
19. Porfiris E, Christopoulos A, Sandris P, Georgiou P, Ioannidis A, Popa CV, et al. Upper eyelid orbicularis oculi flap with tarsoconjunctival island for reconstruction of full-thickness lower lid defects. Plast Reconstr Surg. 1999;103(1):186-91. PMID: 9915182
20. Fricke JCG. Bildung neuer Augenlieder (Blepharoplastik) nach Zerstörungen und dadurch hervorgebrachten Auswärtswendungen derselben. Hamburg: Pethes und Bessler; 1829.
21. Wilcsek G, Leatherbarrow B, Halliwell M, Francis I. The 'RITE' use of the Fricke flap in periorbital reconstruction. Eye (Lond). 2005;19(8):854-60.
22. Destro MW, da Silva AL, Speranzini MB. Lower eyelid repair utilising triangular skin flaps with subcutaneous pedicles. Br J Plast Surg. 1991;44(5):363-7. PMID: 1873616
23. Güzel MZ, Yildirim I, Aygit AC, Aydin Y, Bayramiçli M. Reconstruction of the total lower eyelid defect - useful modifications. Eur J Plast Surg. 1995;18(4):171-4.
24. Friedhofer H, Salles AG, Jucá MCCR, Ferreira MC. Eyelid reconstruction using cartilage grafts from auricular scapha. Eur J Plast Surg. 1999;22(2-3):96-101.
25. Matsuo K, Sakaguchi Y, Kiyono M, Hataya Y, Hirose T. Lid margin reconstruction with an orbicularis oculi musculocutaneous advancement flap and a conchal cartilage graft. Plast Reconstr Surg. 1991;87(1):142-5.
26. Leone CR Jr. Tarsal pedicle flap for lower eyelid reconstruction. Arch Ophthalmol. 1977;95(8):1423-4.
27. Pollock WJ, Colon GA, Ryan RF. Reconstruction of the lower eyelid by a different lid- splitting operation: case report. Plast Reconstr Surg. 1972;50(2):184-7. PMID: 4558116
28. McCord CD Jr, Nunery WR. Reconstructive Procedures of the Lower Eyelid and Outer Canthus. In: McCord CD Jr, ed. Oculoplastic Surgery. New York: Raven Press; 1981. p.194-8.
29. Hughes WL. Total lower lid reconstruction: technical details. Trans Am Ophthalmol Soc. 1976;74:321-9. PMID: 867633
30. Cies WA, Bartlett RE. Modification of the Mustardé and Hughes methods of reconstructing the lower lid. Ann Ophthalmol. 1975;7(11):1497-502.
31. Leibovitch I, Selva D. Modified Hughes flap: division at 7 days. Ophthalmology. 2004;111(12):2164-7. PMID: 15582069
32. Bartley GB, Putterman AM. A minor modification of the Hughes' operation for lower eyelid reconstruction. Am J Ophthalmol. 1995;119(1):96-7.
33. Borges KS, Chedid R, Dibe M, Sbalchiero JC, Leal PRA. Reconstrução de pálpebra inferior com retalho modificado de Hughes: análise de resultados e complicações no Instituto Nacional do Câncer Rio de Janeiro. Rev Bras Cir Plást. 2010;25(3 Suppl.1):23.
34. Chedid R, Borges KS, Santos P, Sbalchiero JC, Dibe MA, Leal PR, et al. Perfil das reconstruções de pálpebra inferior no Instituto Nacional do Câncer: estudo retrospectivo de 137 casos. Rev Bras. Cirurgia Plást. 2010;25(3 Suppl.1):1-102.
1. Departamento de Cirurgia Plástica, Santa Casa
de Passos, Hospital Regional de Câncer de Passos, Passos, MG,
Brazil.
Corresponding author: Diogo Almeida Lima, Avenida Arouca, 260, Centro - Passos, MG, Brazil. Zip Code 37900-152. E-mail: drdiogolima@gmail.com
Article received: August 8, 2017.
Article accepted: October 11, 2017.
Conflicts of interest: none.







































 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter