

Articles - Year 1999 - Volume 14 -
Radial Forearm Flap Experience in 15 Cases of Microsurgical Face and Neck Reconstruction
Retalho Radial do Antebraço: Experiência em 15 Casos de Reconstrução Microcirúrgica de Face e Pescoço
ABSTRACT
Due to its fair, fine texture and hairless skin, and its thin subcutaneous tissue, the radial forearm flap has been largely utilized in face and neck reconstructions. We analized retrospectively our patients who had been submitted to face and neck reconstructions with this flap. From 1994 to 1998) we operated on fourteen patients, including eight women and six men. Their ages ranged from 13 to 63 years old. One patient was operated on 2 times) totalizing 15flaps. The facial vessels were utilized for 87% of the microvascular anastomosis. In all of the cases we set on a reverse flux. The donor site was covered with a thigh split thickness skin graft. The microvascular anastomosis was successful in 93% of the cases. There were only two complications (13%). In one case the venous anastomosis trombosed and the flap suffired total necrosis. The area was successfully reconstructed with the contralateral flap. Another patient suffired a parcial necrosis of the split thickness skin graft at the donor site, which was closed by secondary intention. These results stress the choice of the radial forearm flap as one of the best in face and neck microsurgical reconstructions. The main shortcoming is the unpleasant scar in the donor site.
Keywords: Forearm; surgical flaps; case report; head and neck reconstruction.
RESUMO
Por apresentar pele clara, de textura fina, com poucos pêlos e tecido subcutâneo pouco espesso, o retalho radial do antebraço tem sido largamente utilizado nas reconstruções da face e do pescoço. Fizemos uma análise retrospectiva dos nossos pacientes submetidos a reconstruções de face e pescoço com esse retalho. Durante o período de 1994 a 1998, operamos quatorze pacientes, sendo oito mulheres e seis homens. A idade deles variou de 13 a 63 anos. Um paciente foi operado duas vezes, totalizando 15 retalhos. A a. facial e sua veia comitante foram utilizadas em 87% das anastomoses microvasculares. Em todos os casos estabelecemos fluxo reverso. A área doadora foi coberta com enxerto de pele parcial da coxa. Obtivemos sucesso em 93% das anastomoses microvasculares. Houve apenas duas complicações (13%). Em um caso ocorreu trombose venosa com necrose do retalho, sendo a área reconstruída com o retalho contralateral, que se manteve viável. Outra paciente sofreu perda parcial do enxerto de pele no antebraço, evoluindo com cicatrização por segunda intenção. Os resultados obtidos reforçam a escolha do retalho radial do antebraço como um dos melhores nas reconstruções microcirúrgicas de face e pescoço. Seu principal inconveniente é a cicatriz evidente na área doadora.
Palavras-chave: Antebraço; retalhos cirúrgicos; relato de caso; reconstrução de cabeça e pescoço
The radial forearm flap was first described as a free flap by Yang et al. in 1978, in China(l, 2). Due to that, it is known as "the chinese flap". In 1982, Song et al. published their good results utilizing this flap in 31 patients with postburn scar contractures of the face and neck(3). Since then, this flap has been largely utilized in the western world due to its several clinical applications. Nowadays, it is utilized in face and neck reconstructions, including the oral cavity, nose and pharinge and esophagus.
It has many advantages. Its vascular pedicle is long and its vessels have large caliber, facilitating the vascular anastomosis. The comitant veins together with the radial artery do not have valves, allowing the flux to be reversed. It can be utilized as a composite flap including nerve, bone or tendon(4). Besides that, the forearm skin is similar to that of the face, since it is fair, with a fine texture, almost hairless, and the subjacent subcutaneous tissue is thin. These features make the radial forearm flap the ideal cover for the face and the neck.
We analized our patients retrospectively to show the results and complications associated to the use of this flap in face and neck reconstructions.
PATIENTS AND METHODS
From 1994 to 1998, fourteen patients were submitted to extensive ressections of lesions in the face or in the neck.
All of these patients underwent radial forearm flap reconstruction through microvascular anastomoses.
The surgical technique was the same described by Song et al.(1) (Fig. 1) despite some modifications. We always harvest the flap from the upper forearm end, in order to reduce the morbidity resulting from tendon exposure. In the lower forearm we have incised the skin longitudinally only to obtain a longer vascular pedicle, and we have sutured primarily the resulting linear incision. That is why all of the related cases were anastomosed with a reverse blood supply.
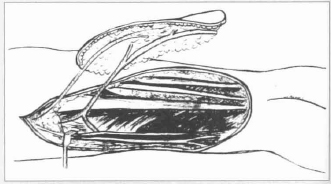
Fig. 1 - Radial forearm flap as described by Yang et al. in 1978, draining through the cephalic vein.
The end to end vascular anastomosis were carried out with the facial artery or the temporal superficialis artery and the venae comitantes. The choice has been made according to the site of the resection and the extension of the flap pedicle. We do prefer the facial artery due to its larger caliber and lesser tortuosity. The cephalic vein has not been utilized in any of our anastomosis.
The donor site in the forearm was covered with a split-thickness skin graft from the thigh. Above the graft we made a tie-over dressing and the extremity was immobilized with a plaster cast.
RESULTS
The cases are described in Table I. Figures 2 to 7 are related to pre and postoperative aspects of some patients. We operated on fourteen patients, performing fifteen flaps. They were 13 to 63 years old, six males and eight females. The microvascular anastomosis was carried on with the facial artery and its venae comitant in 13 of 15 patients (87%). In two patients only we utilized the temporalis superficialis artery and its venae comitante. In all of our patients we established a reverse blood flow.

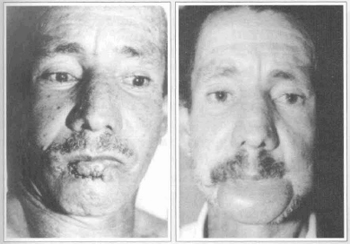
Fig. 2 - Cases 1 and 2: Lower lip escamous cell carcinoma. A. Preoperative view. B. Three months after the second surgery.
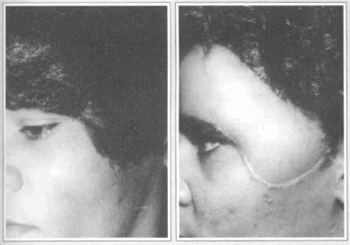
Fig. 3 - Case 3: Frontal pigmented pilous nevus. A. Preoperative view. B. Final result after three months.
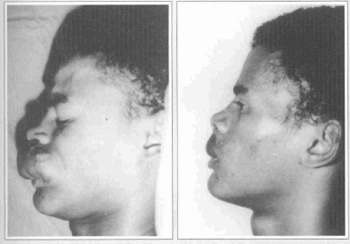
Fig. 4 - Case 4: Upper lip hemangioma, recidive. A. Preoperative view. B. Postoperative view after six months.
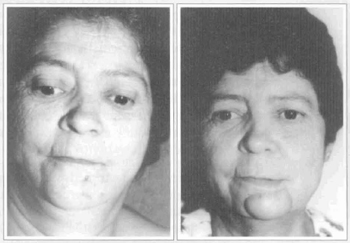
Fig. 5 - Case 5: Mentual basal cell carcinoma, recidive. A. Preoperative view. B. Three months after operation.

Fig. 6 - Case 6: Ulcerated frontal flat hemangioma. A. Preoperative view. B. Postoperative view after three months.
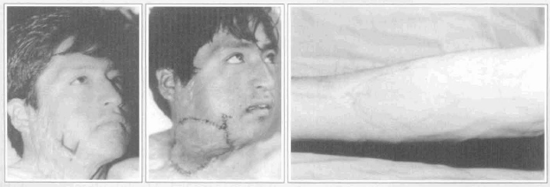
Fig. 7 - Case 12: Postburn cervical contracture. A. Preoperative view. B. Recent postoperative view. C. Postoperative view of the donor area in the forearm after six months.
All of the patients were satisfied with the cosmetic appearance of the reconstruction, except for two women who complained about the thickness of the adjacent skin. One of them was submitted to a parcial resection and stretching of the flap, and she is now satisfied with the final result. The other one will be submitted to the same surgery. One patient considered the resulting scar at the donor site as unpleasant.
One male patient presented a venous trombosis and consequent total necrosis of the flap. He has been submitted to another microsurgical reconstruction with the opposite radial forearm flap, which was successful. In both cases, we have made a composite flap, including the tendon of the palmaris longus muscle. It has been fixed on the orbicularis oris muscle, assuring better oral continence. Cases 1 and 2 of Table I corresponds to this patient.
One female patient suffered a parcial loss of the graft in the forearm, with a consequent exposure of the tendon of the flexor carpi radialis in a 2x2 cm area. The granulating tissue has grown in this area and it was closed by secondary intention.
In the other patients we reached a good result in the donor area of the upper forearm (Fig.7c).
DISCUSSION
Microvascular surgery has progressed, and success rates of 96 to 98 percent have been reported(5). Our experience with the radial forearm flap has shown the confiability of this flap, since we succeeded in 93 percent of the cases. These results increase the popularity of microsurgical flaps, and their indications have become less restricted. Nowadays, in many circumstances, free tissue transfer is the preferred method of treatment, even though conventional local or distant flaps are available.
The donor-site morbidity is the main shortcoming of this flap(6, 7). Tendon exposure, mainly in the lower forearm, prevents the "take" of the graft, since the peri tendinous tissue is fi-equently removed together with the flap. In our patients this happened only once (7%), but the reported rate can reach 79%(8). This problem can be avoided through careful disection, preserving peri tendinous tissue, or protecting the tendons with the adjacent muscle bellies. Other procedures described are full-thickness skin grafts harvested from the abdomen, preexpansion of the forearm skin(6) or prefabrication of fascial splitthickness skin graft, preserving forearm skin(9).
Partial graft loss may be treated conservatively with dressings and debridements of exposed tendons, and they heal by secondary intention. Alternatively, this area can be grafted again. Therefore partial graft loss does not bring longterm morbidity.
The radial forearm flap is one of the best choices for face and neck reconstrutions, due to its functional and aesthetic features, high success rates of microvascular anastomosis and low incidence of donor site morbidity.
REFERENCES
1. YANG G, BAOQUI C, YUZHI G. Free forearm skin transplantation. Natl. Med. J. China 1981; 61:139-41.
2. YANG GF, CHEN PJ, GAO YZ, LIU XY, LI J, JIANG SX, HESP. Forearm free skin flap transplantation. Br. J. Plast. Surg. 1997; 50: 162-5.
3. SONG R, GAO Y, SONG Y, YU Y, SONGY. The forearm flap. Clin. Plast. Surg. 1982;9:21-6.
4. SERLETTI JM, TAVIN E, MORAN SL, CONIGLIO JU. Total lower lip reconstruction with a sensate composite radial forearm-palmaris longus free flap and a tongue flap. Plast. Reconstr. Surg. 1997; 99:559-61.
5. KROLL SS, SCHUSTERMAN MA, REECE GP, MILLER MJ, EVANS GR, ROBB GL, BALDWIN BJ. Choice of flap and incidence of free flap success. Plast. Reconstr. Surg. 1996; 98:459-63.
6. SHOELLER T, OTTO A, WECHSELBERGER G, LILLE S. Radial forearm flap donor-site complications and morbidity. Plast. Reconstr. Surg. 1998; 101:874-5.
7. SUOMINEN S, SHOVUO J, ASKOSELJAVAARA S. Donor site morbidity of radial forearm flap. Scand. J. Plast. Reconstr. Hand Surg. 1996; 30:57-61.
8. RICHARDSON D, FISHER SE, VAUGHAN ED, BROWN JS. Radial forearm flap donor-site complications and morbidity. Plast. Reconstr. Surg. 1997; 99:109-15.
9. WOLFF KD, ERVENS J, HOFFMEISTER B. Improvement of the radial forearm donor site by prefabrication of fascial-split-thickness skin grafts. Plast. Reconstr. Surg. 1996; 98:358-61.
I - Professor of the Faculty of Medicine of the UFMG.
II - Chief of the Plastic Surgery Division of the Hospital da Baleia, Fundação Benjamin Guimarães.
III - Professor of Plastic Surgery of the Faculty of Medical Sciences - Belo Horizonte - MG.
IV - Resident in Plastic Surgery of the Hospital das Clínicas, UFMG.
V - Resident in Plastic Surgery of the Hospital das Clínicas, UFMG.
Address for correspondence:
Edgard Rocha Silva, MD
R. Paulo Freire de Araujo, 30
30450-600 - Belo Horizonte - MG Brazil
Phone: (55 31) 344-9925 Fax: (55 31) 296-9076


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter