

Articles - Year 1999 - Volume 14 -
A Simple Canthopexy
Uma Cantopexia Simples
ABSTRACT
Canthopexies are now integrated to blepharoplasties of the luwer lid. They are of two types: with and without canthotomy. The canthopexy technique we employ is not associated with canthotomy and avoids having to release the lateral canthal tendon. We attach the lateral canthal ligaments to the periosteum of the orbital rim with nonabsorbable suturing material through the superior blepharoplasty wound. 118 patients have been submitted to this procedure. The procedure is quick, greatly reduces morbidity and may be employed in blepharoplasties when there is moderate lid flacidity.
Keywords: Canthopexy; blepharoplasty.
RESUMO
As cantopexias são, hoje, intimamente integradas às blefaroplastias inferiores. Podem ser de dois tipos: com cantotomia e sem cantotomia. A técnica do tipo sem cantotomia que empregamos evita a desinserçâo do ligamento cantal lateral, fixando o ligamento cantal lateral no reborbo orbitário, com fio inabsorvível, tendo como via de acesso a firida da blefaroplastia superior. 118 pacientes foram submetidos à cantopexia associada à blefaroplastia. É um procedimento rápido que diminui sensivelmente a morbidade. Pode ser empregado com sucesso em blefaroplastias onde há moderada flacidez palpebral inferior.
Palavras-chave: Cantopexia; blefaroplastia
Recent studies have indicated that lid retraction after blepharoplasty occurs in 15 to 20%(1, 2) of operated cases. These studies also indicate certain alteration in palpebral fissure dimension with functional consequences(3). Although lid retraction is a complex phenomenon, scar retraction is the most frequent determinant.
Transcutaneous blepharoplasties have become more conservative.
The CO2 laser has contributed to an increase in transconjunctival blepharoplasties. Surgical access through the conjunctiva leaves the skin, the orbicular muscle and the orbital septum untouched. Transconjunctival blepharoplasty also minimizes lid retraction and postoperative ectropion.
Despite all surgical efforts to avoid alteration of the inferior lid position, aging compromises the lateral canthal tendon, an important structural support mechanism(4, 5, 6).
Hypoplasia of the malar bone, shallow orbits, projected globe, and high myopia may also contribute to alterations of the lower lid after blepharoplasty(7).
Several surgeons support blepharoplasty procedure associated with canthoplasty(8, 9, 10, 11, 12, 13, 14, 15) as a way of avoiding post blepharoplasty complications. Flowers(14) performs routine canthoplasty in all inferior blepharoplasties to avoid alterations of the lower lid after surgery.
Believing that this association should be frequent, we carried out several blepharoplasties with canthoplasty association using the CO2 laser for lid resurfacing and canthopexy procedure.
MATERIALS AND METHODS
118 patients were submitted to a tanthoplasty-blepharoplasty association between 1996 and 1998. 96 patient were women (81.3%), the remaining were men (18.7%). Patient's ages varied between 42 and 76 (average age: 59 years). None of the patients had been previously submitted to any sort of aesthetic surgical procedure. All cases showed moderate flacidity of the inferior lid, and in 22 cases, there was antimongoloid obliquity. All patients were operated by the same surgeon (S. L.).
SURGICAL TECHNIQUE
Classical blepharoplasties were performed, followed immediately by transconjunctival canthopexy. The elipse-shaped piece of skin is removed from the superior lid along with a strip of pre-septal orbicular muscle. To remove fatty tissue from the inferior lid, we enter through the conjunctiva. We begin canthoplexy by making a cutaneous incision of about 2 mm, immediatly below the lateral canthus (Fig. 1).
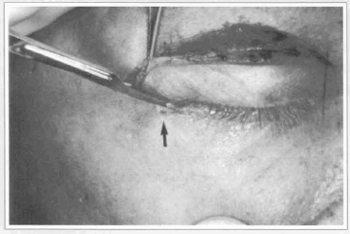
Fig. 1 - Beginning of the canthopexy; 2 mn incision near the lateral canthus (arrow).
Using polipropilene for suturing, we pass a 20 mm needle through the periosteum of the superior orbital rim, in the same direction as the small incision, through the inferior branch of the canthal tendon, reaching the superior lid wound near the initial periosteal fixation point where the canthal tie is made (Figs. 4 & 5). At this phase we can clearly observe the tension at the lower lid and the elevation of the lateral canthus. The hypercorrection lifts the inferior lid between 1 and 2 mm above the inferior limbus, correcting the false impression of excess tissue or of orbicular hypertrophy. After canthopexy, the wound on the superior lid is sutured, and the procedure is completed (Fig. 6).

Fig. 2 - Through the superior lid wound we catch the periosteum of the superior orbital rim.
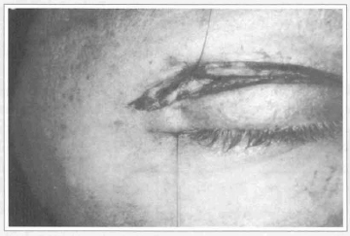
Fig. 3 - The needle comes out of the incision at the lateral canthus.

Fig. 4 - The needle is introduced in the same cutaneous incision, catching the inferior branch of the lateral canthal tendon.

Fig. 5 - The needle comes our near the thread in the superior lid wound, where the final tie is made.
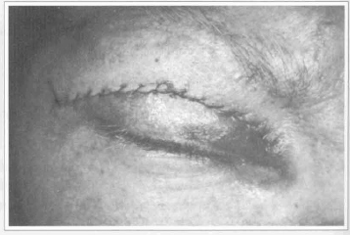
Fig. 6 - Completed superior lid Suture.
It is very important to observe during the canthopexy procedure if the suture has reached the lateral portion of the superior lid levator. Palpebral ptosis would be the immediate consequence.
RESULTS
Flacidity of the lower lid was corrected in all cases. During the first two weeks we observed a greater tension of the lower lid and a slight upward slanting of the the lateral canthus. During this period palpebral movement was slightly limited. In the third week following surgery, lid shape and canthal positioning had become completely normal (Figs. 7a - 7d; 8a - 8d and 9a - 9d).

Fig. 7a - Female patient with bilateral ptosis and inferior scleral show.
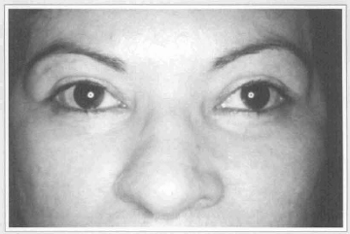
Fig. 7b - Postoperative view. Superior lid blepharoplasty with CO2 laser Ultrapulse and correction of ptosis. Lower lid transconjunctival blepharoplasty, facial resurfacing and canthopexy.
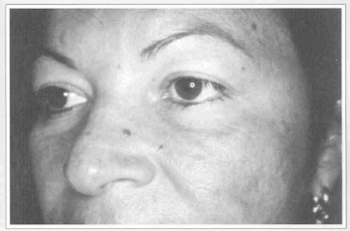
Fig. 7c - Preoperative oblique view.

Fig. 7d - Postoperative oblique view.
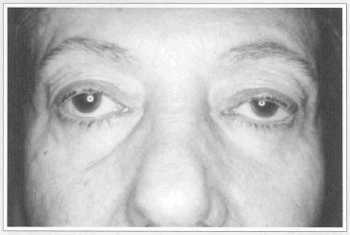
Fig. 8a - Female patient with senile ptosis and inferior scleral show.

Fig. 8b - Postoperative view. Superior lid blepharoplasty with CO2 laser Ultrapulse and correction of ptosis. Lower lid transconjunctival blepharoplasty, aesthetic resurfacing of the peri-orbital area and canthopexy.
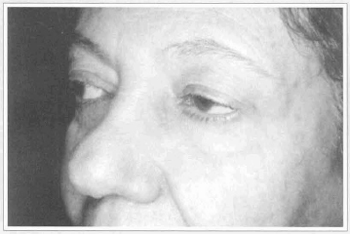
Fig. 8c - Preoperative oblique view.
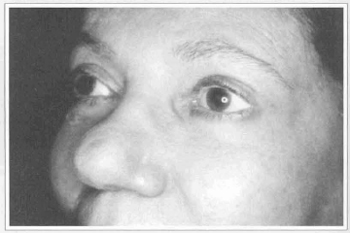
Fig. 8d - Postoperative oblique view.

Fig. 9a - Female patient with dermochalasis, xantelasmas, fatty bags of superior lid. Advanced photo aging of the skin.
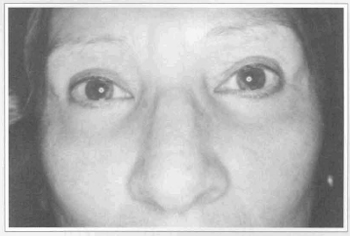
Fig. 9b - Postoperative view. Superior lid blepharoplasty with CO2 laser Ultrapulse. Lower lid transconjunctival blepharoplasty, facial resurfacing and canthopexy.
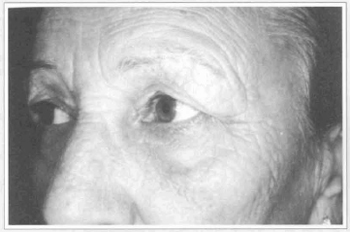
Fig. 9c - Preoperative oblique view.

Fig. 9d - Postoperative oblique view.
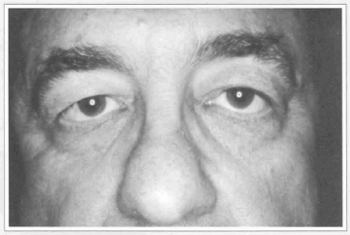
Fig. lOa - Male patient with dermochalasis, antimongoloid obliquity, scleral show.
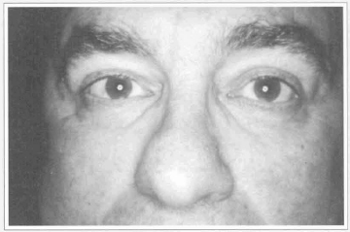
Fig. lOb - Postoperative view. Superior transconjunctival blepharoplasty with CO2 laser Ultrapulse. Inferior transconjunctival blepharoplasty, periorbital resurfacing and canthopexy. Total corretion of flacidity and lid position.
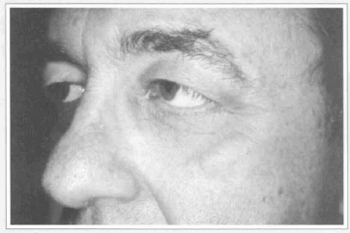
Fig. lOc - Preoperative oblique view.
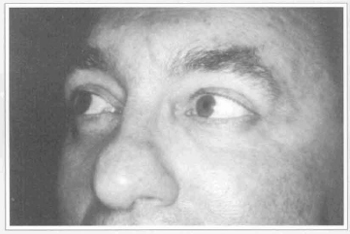
Fig. lOd - Postoperative oblique view.
In two cases small granulomas at the area near the canthopexy tie in the superior orbital rim were observed.
These were ressected after six months without causing any aesthetic harm nor alterations of the inferior lid.
DISCUSSION
Lateral canthoplasties are performed in reconstructive and aesthetic surgical procedures to correct flacidity of the lower lid and to correct the positioning of the lower lid and the lateral canthus. Several canthopexy procedures have been successfully described and employed. Careful evaluation of patients, including analysis of the orbital anatomy, the position of the globe, fissure symmetry and integrity of the canthal ligaments will indicate the type of surgical procedure that should be employed(l5).
There are two classifications of canthoplasties: with or without canthotomy.
In 1966, Bick(16), and Tenzel(l7), in 1969, employed canthotomies in reconstructive procedures. Anderson and Gordy(ll) described a variation of the technique in which a flap of the conjunctival epithelium was employed. Since then the tarsal strip has been widely used in lid surgeries. In 1983, McCord(l8) became the first surgeon to use a variation of this technique to avoid complications in aesthetic blepharoplaslties. In 1987, Lisman and his collaborators(7) began using tarsal suspension in blepharoplasties.
Canthotomies that are associated to lateral fixation offer some advantages, such as: horizontal shortening of the lid shape alterations, elimination of inferior lid retraction and the possibility of association with surgical lifting of the third portion of the face(l5, 19-22). Often these procedures are used to treat blepharoplasty complications, such as lid retraction, ectropion, and complex deformities known as double convexities.
Canthopexies without canthotomies allow for the correction of lid flacidity while preserving the anatomic integrity of the canthus, avoiding lid shortening.
Postoperative quemosis is less frequent; morbidity is reduced. These procedures were developed for use in the correction of lower lid flacidity (4, 8, 13 - 15, 21, 23 - 28). Most of these techniques employ transposition of a muscular or dermal-muscular flap, or, the release of the lateral canthal tendon with a transposition through a suborbicular tunnel towards the periosteum of the lateral orbital rim.
Our technique follows the principles of the canthopexy without canthotomy; however, we do not dissect a submuscular tunnel and avoid the release of the lateral canthal tendon. We perform the canthopexy with nonabsorbant suturing material. This procedure greatly reduced surgical time and drastically lowered morbidity. It may be used in inferior lid flacidity correction and in correction of moderate alterations of antimongoloid obliquity.
We have used this technique in blepharoplasties using CO2 laser equipment. We do not reconunend that it be used in cases of lower lid retraction with anterior and medial lamela alterations. We feel that in such cases, techniques associated with canthotomies and lateral fixation, and resection of the retracting components or elevation of the third portion of the face techniques are more indicated.
We agree with Flowers(14) who considers that canthopexies and fat removal should be the two primary aspects of lower lid blepharoplasties and that the greatest enemy of lasting canthopexies is the resection of skin from the lower lid.
There is a large variety of surgical techniques for the correction of lower lid flacidity and of the alteration of positioning of the lower lid and the lateral canthus. Each of these techniques has a different indication.
The success of all surgical procedures depends on the knowledge of lid anatomy and the preservation of delicate lid structures.
REFERENCES
1. BAYLIS HI, LONG JA, GROT MJ. Transconjuntival lower eyedid blepharoplasty: Thecnique and Complications. Ophthalmology. 1989; 96:1027-1031.
2. MC GRAW BL, ADAMSON PA. Post blepharoplasty ectropion: Prevention and Management. Arch. Otolaryngol. Head and Neck Surg. 1991; 117:852-857.
3. LESSA S, ELENA EH, ARAUJO MRC, e PITANGUY I. Modificações anatomicas da fenda palpebral após blefaroplastia. Rev. Bras. Cir. 1997; 87:179-188.
4. WHITAKER LA. Selective alteration of palpebral fissure form by lateral canthopexy. Plast. Reconstr. Surg. 1984; 74:611-615.
5. HILL JC. An analysis of senile changes in the palpebral fissure. Can. J. Ophthalmol. 1975; 10:32-35.
6. OUSTERHOUT DK, and WEIL RB. The role of lateral canthal tendon in lower eyelid laxity. Plast. Reconstr. Surg. 1982; 69:620-622.
7. LISMAN RD, REES T, BAKER D, and SMITH B. Experience with tarsal suspension as a factor in lower lid blepharoplasty. Plast & Reconstr. Surg. 1987; 79:897-905.
8. HINDERERUT. Blepharocanthoplasty with eyebrow lift. Plast Recontr. Surg. 1975; 56:402-409.
9. ADAMSON JE, MC CRAW JB, CARRAWAY JH. Use of muscle flap in lower blepharoplasty. Plast. Reconstr. Surg. 1979; 63:359-363.
10. MLADICK RA. The muscle-suspension lower blepharoplasty. Plast. Reconstr. Surg.1979; 64:171-175.
11. ANDERSON RL, and GORDY DD. The tarsal strip procedure. Arch. Ophthalmol. 1979; 97:2192-2196.
12. FLOWERS RS. Canthopexy with aesthetic blepharoplasty. Presented to annual meeting of the American Society for Aesthetic Plastic Surgeons. April, 1983.
13. ORTIZ-MONASTERIO F, RODRIGUES A. Lateral canthoplasty to change the eye slant. Plast. Reconstr. Surg. 1985; 75:1.
14. FLOWERS RS. Canthopexy as a routine blepharoplasty component. In Blepharoplasty and Periorbital Aesthetic Surgery. Clin. Plast. Surg. 1993; 20:351-365.
15. JELKS GW, GLAT PM, JELKS EB and LONGAKER MT The inferior retinacular lateral canthoplasty: A new technique. Plast. Reconstr. Surg. 1997; 100:1262-1270.
16. BICK MW. Surgical management of orbital tarsal disparity. Arch. Ophthalmol. 1966; 75:386.
17. TENZEL RR. Treatment of lagophthalmos of the lower lid. Arch. Ophthalmol. 1969; 81:366-371.
18. MC CORD CD JR, and SHORE JW Avoidance of complications in lower lid blepharoplasty. Ophthalmol. 1983; 90:1039-1046.
19. HESTER TR, CODNERMA, and MC CORD CD. Subperiosteal Malar Cheek Lift with Lower lid Blepharoplasty. In C.D. Mc Cord (Ed), Eyelid Surgery: Principles and Thechniques. Philadelphia: Lippincott-Raven. 1995; p. 149.
20.HESTER TR, CODNER MA, and MC CORD, CD. The "centro facial" approach for correction of facial ageing using the transblepharoplasty subperiosteal cheeklift.Aesthetic Surg. Q. 1996; 16:51-57.
21. LASSUS C. An easy canthoplasty. Aesth. Plast. Surg. 1996; 20:137-140.
22. GLAT PM, JELKS GW, JELKS EB, WOOD M, GADANGI P and LONGAKER MT. Evolution of the lateral canthoplasty: techniques and indications. Plast. Reconstr. Surg. 1997; 100: 1396-1405.
23. FLOWERS RS. Advanced blepharoplasty: Principles of precision. In. Gonzalez-Ulhoa M et al (eds): Aesthetic Plastic Surgery, Vol. 2. Padua, Piccin, Nuova Libraria, 1987; p. 115.
24. HINDERER UT. Correction of weakness of the lower eyelid and latheral canthus. Clin. Plast. Surg. 1993; 20:331-349.
25. EDGERTON MT and WOLFORT FG. The dermal flap canthal lift for lower eyelid support: A technique of value in the surgical treatment offacial palsy. Plast. Reconstr. Surg. 1969; 43:42-52.
26. MONTADON D. A modification of the dermalflap canthal lift for connection of the paralyzed eyelid. Plast. Reconstr. Surg. 1978; 61:555-557.
27. MARSH JL and EDGERTON MT. Periosteal pennant lateral canthoplasty. Plast. Reconstr. Surg. 1979; 64:24-29.
28. HAMRA ST. The zygorbicular dissection in composite rhytidectomy: An ideal midface plane. Plast. Reconstr. Surg. 1998; 102:1646-1657.
I - Assistant Professor at the Post Graduate Medical School of the Pontificia Universidade Catolica do Rio de Janeiro, at the Carlos Chagas Medical Institute, at the 38th Infirmary of the Santa Casa de Misericordia do Rio de Janeiro (Prof. Ivo Pitanguy's Service). Head of the Oculo-Plastic Department of the 1st Infirmary of the Santa Casa de Misericordia do Rio de Janeiro (Prof. Paiva Goçalves' Service); Member of the Brazilian College of Surgeons (TCBC), Specialist of the Brazilian College of Surgeons (TSBCP).
II - Assistant Professor at the Post Graduate Medical School of the Pontificia Universidade Catolica do Rio de Janeiro, at the Carlos Chagas Medical Institute, at the 38th Infirmary of the Santa Casa de Misericordia do Rio de Janeiro (Prof. Ivo Pitanguy's Service). Plastic Surgeon of the Oculo-Plastic Department of the 1st Infirmary of the Santa Casa de Misericordia do Rio de Janeiro (Prof. Paiva Gonçalves' Service); Assistant Professor of the Oculo-Plastic Department of the Ophthalmology Service (Prof. Renato Curi's service) of the Federal Flurninense University (HUAP), Member of the Brazilian College of Surgeons (TCBC), Specialist of the Brazilian College of Surgeons (TSBCP).
III - Plastic Surgeon at the 1st Infirmary of the Santa Casa de Misericordia do Rio de Janeiro (Prof. Paiva Gonçalves' service), at the 38th Infirmary of the Santa Casa de Misericordia (Prof. Ivo Pitanguy's service), Specialist of the Brazilian College of Surgeons (TSBCP).
Address for correspondence:
Av. Ataulfo de Paiva, 135 - cj. 1101
22449-900 - Rio de Janeiro - RJ Brazil
Phone: (5521) 259 1245 - Fax: (55 21) 259 0099
e-mail: slessa@iptec.com.br


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter