

Original Article - Year 2019 - Volume 34 -
Epidemiological analysis and evolution of patients undergoing reconstructive plastic surgery in a trauma referral hospital
Análise epidemiológico-evolutiva de pacientes submetidos a cirurgia plástica reparadora em um hospital de referência em trauma
ABSTRACT
Introduction: Trauma injuries are sudden aggravations to health that may lead to temporary disabilities and interfere with the victim's quality of life. The reconstructive plastic surgery (RPS) unit of the Urgency and Emergency Metropolitan Hospital (Hospital Metropolitano de Urgência e Emergência - HMUE) is a referral unit for the treatment of trauma patients in the state of Pará, Brazil.
Methods: This was an observational, analytical, and cross-sectional prospective study. The study population was composed of 78 patients treated from December 2015 to December 2016.
Results: The study population was predominantly male, autonomous, and aged between 21 and 30 years. Traffic accidents were the most frequent cause of trauma. The most affected area was the lower limbs, and the most common type of surgery performed was grafting. Viability was in the range of 90-100% in both patients undergoing graft and flap surgery. No significant association was found between the age range of patients and the degree of viability. However, there was a relationship between the number of days from the accident until the medical intervention and the degree of graft viability.
Conclusion: Patients admitted to the hospital on the same day of the accident were six times more likely to present graft viability above 80%, and therefore, to have a favorable outcome.
Keywords: Reconstructive surgical procedures; Epidemiology; Wounds and injuries; Clinical Evolution
RESUMO
Introdução: Lesões decorrentes de trauma são agravos súbitos à saúde que podem levar a deficiências temporárias e interferir na qualidade de vida das vítimas. O serviço de Cirurgia Plástica Reparadora (CPR) do Hospital Metropolitano de Urgência e Emergência (HMUE) atua como a unidade de referência no tratamento de feridas dos pacientes vítimas de trauma no Estado do Pará.
Métodos: Estudo observacional analítico, do tipo transversal prospectivo. A população foi composta por 78 pacientes atendidos no período de dezembro de 2015 até dezembro de 2016.
Resultados: A população predominante foi de pacientes do sexo masculino, autônomos, entre 21 a 30 anos. Os acidentes automobilísticos foram os mais prevalentes. A área corporal mais afetada foi a dos membros inferiores e o tipo de cirurgia mais realizada foi enxerto. Tanto entre os pacientes submetidos à cirurgia de enxerto quanto os de retalho, predominou a viabilidade no intervalo de 90-100%. Não foi verificada associação significativa da faixa etária dos pacientes sob o grau de viabilidade. Houve relação entre o número de dias do acidente até a intervenção com o grau de viabilidade do enxerto.
Conclusão: Os pacientes internados no hospital no mesmo dia do acidente têm seis vezes mais chance de apresentar viabilidade do enxerto acima de 80% e, portanto, desfecho favorável.
Palavras-chave: Procedimentos cirúrgicos reconstrutivos; Epidemiologia; Ferimentos e lesões; Evolução clínica
INTRODUCTION
The reconstructive plastic surgery (RPS) unit of the Urgency and Emergency Metropolitan Hospital (HMUE) in Ananindeua acts as a referral unit for the treatment of trauma patients in the state of Pará, Brazil. It also provides referral support for other specialties of the hospital, and therefore, receives a large volume of patients1.
Trauma injuries are sudden health problems that can lead to death. Trauma injuries may be a result of urban violence or traffic accidents, termed as external causes in the International Classification of Diseases2.
Trauma injuries are one of the leading causes of preventable death. Therefore, knowing the epidemiological and evolutionary profile of patients involved in these type of accidents allows the use of more effective strategies for the prevention and reduction of temporary or permanent disabilities that interfere negatively with the victims’ quality of life3,4.
METHODS
This was an analytical, observational, and cross-sectional prospective study conducted at the RPS unit of the HMUE. The population was comprised of 78 patients treated by the HMUE reconstructive plastic surgery team from December 2015 to December 2016.
Patients of both genders and all age groups who were victims of trauma and treated in the RPS unit of the HMUE from December 2015 to December 2016 and who agreed to participate in the study and signed an informed consent form (ICF) were included in the study. Patients who were treated outside of this interval, patients younger than 18 years who did not have authorization from a legal guardian, unconscious patients, or patients who refused to sign the ICF or who failed to meet the analyzed criteria were excluded from the study.
Data was collected on two separate occasions. First, an interview was conducted with patients before reconstructive surgery. Patients answered an epidemiological questionnaire and information related to the trauma was collected. Then, information was collected after the invention regarding the treatment performed and its evolution, in accordance with medical supervision and medical records.
Pearson’s non-parametric chi-square test for trend/adhesion and for association between nominal variables, symbolized by χ2, was adopted. A p-value of <0.05 was considered statistically significant. In order to verify the significant or non-viable prevalence of the surgery according to factors such as age, hospital distance (km), days between the accident and hospitalization, and hospitalization days prior to surgery, the odds ratio (OR) was calculated with a significance level of 0.05.
The collected data were tabulated, processed, and analyzed by means of descriptive and inferential statistics. The programs Microsoft Excel and Statistical Package for Social Sciences(SPSS) (version 22.0), both for Windows 7, were used for the statistical analysis of data.
The project was approved by the ethics committee of the State University of Pará (Universidade do Estado do Pará), Biological and Health Sciences Center, Campus II (Opinion No. 1.004.945).
RESULTS
Most study patients were in the age range of 21 to 30 years (32.05%), followed by the age range of 11 to 20 years (21.79%) and 31 to 40 years (20.51%). The male sex was predominant among patients, as was origin from the municipality of Belém (32.05%) and autonomy (34.62%), with a significant trend (p < 0.005).
With regard to the mechanism of trauma, 78% of accidents were blunt traumas, 18% were penetrating traumas, and 4% were unreported. Among the patients who were classified as having penetrating traumas, 64% were the result of firearms and 36% were the result of bladed weapons. Car accident (collision between vehicles) was the main type of accident among patients, with the lower limbs being most affected (in 67.95% of cases), followed by the upper limbs (16.67% of cases).
With respect to hospital distance, the majority of patients (47.44%) travelled between 1-30 km from the site of the accident to the HMUE. Approximately 66.67% patients were hospitalized on the same day of the accident. Most patients (38%) waited between 30-59 hospital days before the operation.
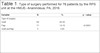
Table 1 shows that 82.05% of patients underwent some type of skin graft surgery. Table 2 shows that both patients who underwent graft surgery (82.05%) and those who underwent flap surgery (14.10%) had viability in the range of 90-100%.
| Variable | N | % | p - value |
|---|---|---|---|
| Type of surgery | |||
| Graft | 64 | 82.05 | <0.0001** |
| Flap | 11 | 14.10 | |
| Graft and flap | 3 | 3.85 |
Source: Data from this study (2016)(1); Pearson's Chi-square test (p-value <0.05);
** Highly significant difference;
| Viability (%) | Type of surgery | Total | |||||
|---|---|---|---|---|---|---|---|
| Graft | Flap | Graft/flap | |||||
| Qty | % | Qty | % | Qty | % | ||
| 0-19 | 0 | 0 | 1 | 1.28 | 1 | 1.28 | 2 |
| 20-29 | 0 | 0 | 1 | 1.28 | 0 | 0 | 1 |
| 70-79 | 1 | 1.28 | 0 | 0 | 0 | 0 | 1 |
| 80-89 | 9 | 11.54 | 3 | 3.85 | 0 | 0 | 12 |
| 90-100 | 54 | 69.23 | 6 | 7.69 | 2 | 2.56 | 62 |
| Total | 64 | 82.05 | 11 | 14.1 | 3 | 3.85 | 78 |
Source: Data from this study (2016); RPS: reconstructive plastic surgery; HMUE: Hospital Metropolitano de Urgência e Emergência.
Table 3 shows that with graft surgery, 84.38% of patients had a good outcome, followed by 15.63% of patients who had a fair outcome. With flap surgery, 54.55% of patients had a good outcome, followed by 27.27% with a fair outcome, and 18.18% with a poor outcome. Among patients who had graft and flap surgery, 66.67% had a good outcome and 33.33% had a poor outcome. It should be noted that among both patients who underwent graft and flap surgeries, a good outcome was predominant.
| Result (%) | Type ofsurgery | Total | |||||
|---|---|---|---|---|---|---|---|
| Graft | Flap | Graft/flap | |||||
| Qty | % | Qty | % | Qty | % | ||
| Poor (loss > 80% or dehiscence) | 0 | 0 | 2 | 18.18 | 1 | 33.33 | 3 (84%) |
| Fair (loss between 30-79%) | 10 | 15.63 | 3 | 27.27 | 0 | 0 | 13(16.66%) |
| Good (<20% of loss) | 54 | 84.38 | 6 | 54.55 | 2 | 66.67 | 62(79.5%) |
| Total | 64 | 11 | 3 | 78 | |||
Source: Data from this study (2016). RPS: reconstructive plastic surgery; HMUE: Hospital Metropolitano de Urgência e Emergência.
There was a correlation between the date of hospitalization after the accident and graft viability. Among patients who were hospitalized on the same day of the accident, 63.16% presented graft viability above 80%, whereas only 5.26% presented graft viability less than 80%. In patients who were admitted a day or more after the accident, the percentage of patients with less than 80% viability was two-fold higher (10.53%). That is, among patients who waited more than one day to be admitted, the percentage of graft variability was lower. In Table 4, the OR indicates that patients hospitalized on the same day as the accident were six-fold more likely to present graft viability above 80% (p < 0.05).
| Days between accident and hospitalization (n=76) | Viability | Odds Ratio | p - value | |||
|---|---|---|---|---|---|---|
| 0% to 80% | Above 80% | |||||
| n | % | n | % | |||
| On the same day | 4 | 5.26 | 48 | 63.16 | 6.00 | 0.0120* |
| 1 or more days | 8 | 10.53 | 16 | 21.05 | ||
Fonte: Data from this study (2016) (1); Odds Ratio (p-value < 0.05)
No significant correlation was found (p > 0.05) between the number of days which passed between hospitalization and surgery and the degree of graft viability. In order words, the viability rate was independent of the number of days patients waited after admission before undergoing reconstructive surgery.
DISCUSSION
Our study had a predominance of male patients (87.18%). Similar studies5,6 also found a predominance of males. Males are more involved in traumatic events. Social and cultural factors related to gender expose the male sex to higher trauma risks, such as excessive speed when driving cars, hazardous maneuvers in traffic, violent behavior, and a greater consumption of alcohol, making them more vulnerable to external causes7.
With regard to age, other studies also demonstrated that the age range between 21 and 30 years was the most frequent8.
With respect to the origin of patients, the municipality of Belém was the most common origin (32.05%) with a significant trend (p < 0.05), followed by the municipality of Ananindeua (5.13%), where the HMUE is located. Belém has more traumatic events than Ananindeua because it is a capital city and has a larger population. Another reason is the geographic relationship between these two cities: they are close, almost a conurbation, thus facilitating the regulation and transport of patients to the HMUE.
Approximately 47.44% of enrolled patients were smokers. Patients with diabetes and alcoholic intake had a low frequency (1.28%). However, this value was probably underestimated since data was collected by an interview and many may have felt afraid to speak truthfully about alcoholic beverage intake.
In this study the mechanism of trauma was classified as blunt or penetrating, with 78% being classified as blunt traumas (events such as car accidents, falls, accidents at work, etc.) and 18% being classified as penetrating traumas (events involving perforation by bladed weapons or firearms). Approximately 4% of traumas were unreported. A similar result was found in a 2016 study9, in which 78.24% of injuries were blunt traumas, 21.39% were penetrating, and 0.37% were not included in these classifications. In 2014, another study reported that 86.4% of traumas were blunt, whereas 13.6% were penetrating10.
In this study, car accident (38.46%) was the main type of accident and showed a significant trend (p < 0.05), which is consistent with a study conducted in 2014 in which car accidents ranked as the main cause of attendance (44.85%)11.
Traffic accidents are complex events because they may be related to human failure, vehicle failure, and even the environment. Some of these factors are the result of driver carelessness, such as hazardous maneuvers, alcohol intake and drug abuse, excessive speeding, and fatigue, as well as climatic conditions, inadequate roads and signage, and lack of vehicle maintenance12.
In this study 71.70% of patients were in accidents involving motorcycles, and the majority (96.77%) were victims of collision accidents with other vehicles. Of the fall accidents, 45.45% involved motorcycles, whereas 27.27% of run-over accidents involved motorcycles.
Majority of the patients (47.44%) travelled between 1-30 km from the site of the accident to the hospital, a statistically significant result. This result is possibly justified by the predominant origin of patients from Belém, which is a town near Ananindeua where the HMUE is located.
Regarding the number of days between the accident and hospitalization, 66.67% patients were hospitalized on the same day as the accident. This trend is significant (p < 0.05), probably because most of the injured were from Belém, a city close to the HMUE.
With respect to the number of days between the date of admission and the date of reconstructive surgery at the HMUE, 38.46% of patients underwent surgery 30-59 days after hospital admittance. The second highest proportion of patients (33.33%) underwent surgery less than 30 days after admission. These trends were significant (p < 0.05).
The patients referred to the RPS unit were first admitted to the emergency room, where they usually underwent general and/or orthopedic surgery, before being referred to the plastic surgery unit, which explains this timeframe for the reconstructive intervention. Another reason for this interval may be due to the delay in requesting other specialties so that the plastic surgery team could evaluate the patient or the wait to improve wound conditions before performing surgery.
The most common surgical procedure performed in this study was skin grafting (82.05%), with a significant trend (p < 0.05). Flap surgery was performed in 14.10% patients, and 3.85% patients underwent graft and flap surgery. A similar 2017 study8 also identified skin grafting as the most common reconstructive procedure (62.1% of cases). Fasciocutaneous flap was the second most frequent procedure, performed in 21.9% of cases, followed by muscle flap in 12.6%, and microsurgical flap in 3.4%. However, only patients with lower limb trauma were analyzed. In this study, we did not differentiate the type of flap, which may be interesting to do in future studies.
The results showed that the most affected body area was the lower limbs in 67.95% cases, with a significant tendency (p <0.05), followed by the upper limbs (16.67%), head (5.13%), and trunk (2.56%), whereas 7.69% cases were unreported. In the epidemiological analysis of trauma victims in a similar study13, the most affected body regions were the lower limbs (27.4% cases), followed by the upper limbs (22.1% cases).
Complex limb wounds are increasingly common, mainly due to the growing number of motorcycle accidents14. The leg region has a thin subcutaneous layer and few muscle bellies, permitting the exposure of the tibia and tendons in trauma with the loss of soft tissue, which is often associated with fractures15.
In patients who underwent skin graft surgery (82.05%) and in patients who underwent flap surgery (14.10%), the predominant viability was between 90-100%. This result demonstrates that the HMUE reconstructive surgery team followed preoperative, intraoperative, and postoperative recommendations, as a viability of 90-100% in surgical skin grafts and flaps reflects a successful management of patient extrinsic factors.
There was no significant prevalence (p >0.05) of the age group with viability, meaning the viability of the surgery was independent of the patient’s age. Pearson’s correlation test was also performed, which confirmed that there was no significant correlation between age and degree of viability. The degree of correlation between the two variables was negative and weak (r = - 0.155), which was in contrast to existing literature. Elderly patients are more susceptible to surgical wound rupture and healing delay than younger patients. With aging, collagen undergoes qualitative and quantitative changes. The collagen content in the dermis diminishes with age, and the aged collagen fibers present distorted architecture and organization16.
There was a significant correlation (p < 0.05) between the number of days before hospitalization after the accident and the degree of viability. The ORindicates that patients hospitalized on the same day as the accident were six-fold more likely to present viability above 80% (p < 0.05). Early admission influences the early care of trauma and helps prevent wound infection, an important factor in the delay of surgical treatment. Therefore, the earlier the patient is hospitalized, the faster care is received, preventing the injury from developing into infection and necrosis.
In this study, 47.43% of patients were smokers, whereas 52.56% were non-smokers. When the influence of smoking on the viability of surgery was analyzed, viability was above 80% in both smokers (44.87%) and non-smokers (50%). These results are in contrast to a study conducted in 201217, which found that the risk of developing wound healing complications was twice as high in smokers than in non-smokers.
There was no significant correlation (p > 0.05) between the number of days that the patient had to wait to perform reconstructive surgery after admission and the degree of viability. In other words, the viability of the surgery did not depend on the number of days that the patient waited to perform plastic surgery after admission, thus proving that preoperative, intraoperative, and postoperative care was more important than the speed in performing the procedure.
Closure reconstruction should be performed only when the wound bed is suitable to receive coverage18. Local and systemic wound factors and patient condition should be assessed, since they are crucial for treatment success19.
CONCLUSION
In conclusion, the profile of the average patient admitted to the reconstructive plastic surgery unit for trauma was young, male, of an economically active age, autonomous, a smoker, and from the city of Belém. Blunt trauma was the predominant cause of injury. The main traumatic events were traffic accidents and aggressions, with lower limbs being the most affected area of the body. The most commonly performed type of surgery was graft surgery. The percentage of surgical viability was independent of the age and distance travelled by the patient from the accident site to the hospital. Patients hospitalized on the same day as the accident were six times more likely to have surgical viability above 80%.
COLLABORATIONS
|
FSV |
Final manuscript approval; supervision. |
|
FAS |
Analysis and/or data interpretation; conception and design study; data curation; investigation; project administration; writing - original draft preparation. |
|
ANNF |
Analysis and/or data interpretation; resources; writing - original draft preparation; writing - review & editing. |
|
JPSN |
Analysis and/or data interpretation; conception and design study; data curation; investigation; project administration; resources; writing - review & editing. |
|
LSM |
Conception and design study; formal analysis; investigation; methodology; project administration; resources; validation. |
REFERENCES
1. Motoki THC, Carvalho KC, Vendramin FS. Perfil de pacientes vítimas de trauma em membro inferior atendidos pela equipe de cirurgia reparadora do Hospital Metropolitano de Urgência e Emergência. Rev Bras Cir Plást. 2013;28(2):276-81. DOI: http://dx.doi.org/10.1590/S1983-51752013000200018
2. Sociedade Brasileira de Atendimento Integral ao Traumatizado. Trauma. 2015. [acesso 2018 Jan 8]. Disponível em: http://www.sbait.org.br/trauma.php
3. Seerig LM, Bacchieri G, Nascimento GG, Barros ALD, Demarco FF. Use of motorcycle in Brazil: users profile, prevalence of use and traffic accidents occurrence - a population-based study. Ciênc Saúde Coletiva. 2016;21(12):3703-10. DOI: http://dx.doi.org/10.1590/1413-812320152112.28212015
4. Chang AJBA, Milcheski DA, Nakamoto H, Tuma Junior P, Lobato R, Ferreira MC. Condutas em traumas complexos de partes moles de membros inferiores no HCFMUSP. Rev Bras Cir Plást. 2013;28(3):87.
5. Praça WR, Matos MCB, Fioravanti RK, Magro MCS, Hermann PRS. Perfil epidemiológico e clínico de vítimas de trauma em um hospital do Distrito Federal, Brasil. Rev Pre Infec Saúde. 2017;3(1):1- 7.
6. Gomes ATL, Silva MF, Dantas BAS, Miranda JMA, Melo GMS, Dantas RAN. Perfil epidemiológico das emergências traumáticas assistidas por um serviço pré-hospitalar móvel de urgência. Enferm Global. 2017;16(45):384-415.
7. Arnauts I, Oliveira MLF. Padrão de consumo do álcool por jovens vítimas de trauma e usuários de álcool. REME Rev Min Enferm. 2012;16(3):410-8.
8. Rezende RBM, Macedo JLS, Rosa SC, Galli FS. Perfil epidemiológico e tratamento de perdas de substância por trauma em membros inferiores. Rev Col Bras Cir. 2017;44(5):444-51. DOI: http://dx.doi.org/10.1590/0100-69912017005004
9. Souza Filho PHF. Análise do Atendimento de Pacientes Politraumatizados no Hospital do Subúrbio
10. [Monografia]. Salvador: Universidade Federal da Bahia; 2016.
11. Monteiro KS. Perfil do Paciente Traumatizado: caracterização das variáveis pré e intra-hospitalar
12. [Monografia]. Ceilândia: Universidade de Brasília, Faculdade de Ceilândia; 2014.
13. Souza CB, Leão CEG, Mafra MVM, Viel DO, Dupin AE, Ramos PVS, et al. Perfil epidemiológico dos pacientes atendidos pelo serviço de cirurgia plástica do hospital João XXIII em Belo Horizonte/MG no período de março à agosto de 2013. Rev Bras Cir Plást. 2014;29(2):269-74.
14. Ulbrich ME, Mantovani MF, Balduino AF, Reis BK. Protocolo de enfermagem em atendimento emergencial: subsídio para o acolhimento às vítimas. Cogitare Enferm. 2010;15(2):286-92. DOI: http://dx.doi.org/10.5380/ce.v15i2.17863
15. Nogueira JM, Oliveira SMC. Análise epidemiológica das vítimas de trauma. Rev Mov (Goiânia). 2014;7(3):738-49.
16. Brasil. Ministério da Saúde. Sistemas de Informações Hospitalares do SUS (SIH-SUS). Morbidade Hospitalar do SUS por Acidentes de Transporte por Local de Internação 2016. [acesso 2018 Abr 7]. Disponível: http://tabnet.datasus.gov.br/cgi/tabcgi.exe?sih/cnv/niuf.def
17. Vendramin FS. Retalho sural de fluxo reverso: 10 anos de experiência clínica e modificações. Rev Bras Cir Plást. 2012;27(2):309-15. DOI: http://dx.doi.org/10.1590/S1983-51752012000200023
18. Leong M, Phillips LG. Cicatrização de Feridas. In: Townsend KL, Beauchamp CM, Evers RD, Mattox BM. Sabiston. Tratado de Cirurgia: A Base Biológica da Prática Cirúrgica Moderna. 19a ed. Rio de Janeiro: Elsevier; 2014.
19. Wong J, Lam DP, Abrishami A, Chan MT, Chung F. Short-term preoperative smoking cessation and postoperative complications: a systematic review and meta-analysis. Can J Anaesth. 2012;59(3):268-79. DOI: http://dx.doi.org/10.1007/s12630-011-9652-x
20. Teixeira Neto N, Chi A, Paggiaro AO, Ferreira MC. Tratamento cirúrgico das feridas complexas. Rev Med (São Paulo). 2010;89(3/4):147-52.
21. Park H, Copeland C, Henry S, Barbul A, Complex wounds and their management. Surg Clin North Am. 2010;90(6):1181-94.
1. Sociedade Brasileira de Cirurgia Plástica, São
Paulo, SP, Brazil
2. Universidade Federal do Pará, Belém, PA,
Brazil
3. Hospital Metropolitano de Urgência e
Emergência, Ananindeua, PA, Brazil
4. Universidade do Estado do Pará, Belém, PA,
Brazil
5. Centro Universitário do Estado do Pará, Belém,
PA, Brazil.
Corresponding author: Fabiel Spani Vendramin Rua Municipalidade, nº 985, sala 2112 - Umarizal, Belém, PA, Brazil Zip Code 66050-350 E-mail: drfabiel@gmail.com
Article received: June 19, 2018.
Article accepted: November 11, 2018.
Conflicts of interest: none.





 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter