

Reviw Article - Year 1998 - Volume 13 -
Facial Rejuvenation with CO2 Laser - A Study of 200 Patients
Rejuvenescimento Facial com Laser de CO2 - Revisão de 200 Pacientes
ABSTRACT
C02 laser Ultrapulse (Coherent Inc.) was used in 200 patients, from March 1996 to December 1997. In 180 patients (90%) full face laser resurfacing was done, and in 87 patients (48,3%) this procedure was associated with face lifting surgery. On the remaining 20 patients, CO2 laser was applied on other body areas, as dorsal hands, and for excision of warts and nevi. All patients submitted to laser resurfacing were previously treated during 1 to 2 months with retinoic acid and hydroquinone. The procedures were done under local anesthesia supervised by an anesthesiologist. A clear film dressing impregnated with silicone gel (Silon TSR, Bio-Med Sciences, Bethlehem, PA, USA) was used for 6 to 7 days and complete healing was observed in 7 to 10 days. Complications were exclusively dermatological, without relation to surgery. Ten consecutive patients have undergone skin biopsies for the study of the histological effects of the laser. Personal satisfaction, evaluated after 6 months to one year was excellent in 58%, good in 30%, regular in 10% and poor in 2%. In the last one, severe acne scars were observed, with indication to repeat the treatment.
Keywords: laser; resurfacing; facial rejuvenation.
RESUMO
Utilizamos o laser de CO2 Ultrapulse (Coherent Inc.,Palo Alto, CA) em 200 pacientes, de março de 96 a dezembro de 1997. O laser na face foi realizado em 180 pacientes (90%) sendo que em 87 pacientes (48,3%) esse procedimento foi associado a ritidoplastia. Nos 20 pacientes restantes, o laser de CO2 foi utilizado em outros segmentos do corpo, como no tratamento do dorso das mãos e na retirada de nervos e verrugas da face e de outras áreas do corpo. Todos os pacientes submetidos a laser de face foram preparados previamente por um período de 1 a 2 meses com ácido retinóico e hidroquinona. Os procedimentos foram realizados sob anestesia local e sedação, supervisionados por anestesiologista. Utilizou-se curativo semipermeável impregnado com silicone gel (Silon TSR) Bio-Med Ccinces, Bethlehem, PA, USA) por um período de 6 a 7 dias, com cicatrização completa após 7 a 10 dias. Todas as intercorrências pós-operatórias foram de origem dermatológica, sem qualquer complicação de ordem cirúrgica. Dez pacientes consecutivos foram submetidos a biópsia de pele para estudo histológico da ação do laser. A satisfação pessoal, avaliada após um período de 6 a 12 meses, foi ótima em 58%, boa em 30%, regular em 10% e insatisfatória em 2% dos casos. Os últimos foram seqüelas de acne grave com indicação de repetir o procedimento.
Palavras-chave: laser; resurfacing; rejuvenescimento facial
In the last years, many authors have been studying the applications of CO2 laser, which led to a worldwide divulgation of this technology(3, 4, 10, 11, 13, 15).
The continuous evolution of the CO2 laser technology - Computer Pattern Generator Scanner (CPG) - facilitated its use for procedures in the whole face(1, 2, 12).
With the successful use of CO2 laser in association with some minimal procedures of face surgery like superior blepharoplasty, inferior transconjunctival blepharoplasty and endoscopic browlift, we have begun to use CO2 laser together with cervicofacial rhytidoplasty, even over the cutaneous flap. The flap is subcutaneously undermined and the residual thermal coagulation effect of the CO2 laser reaches the dermis.
The subdermal vascularization of the flap remains intact(9).
MATERIAL & METHODS
From March 1996 to December 1997, 200 laser resurfacing procedures were performed. We used CO2 laser Ultrapulse (Coherent, Inc., Palo Alto, CA). 190 patients were female and 10 were male. Patient's age ranged from 15 to 70 years old, predominating the patients aging 40-49 years (30%) and 50-59 (29%).
Patients were previously prepared. The treatment began 1 month before the resurfacing in patients with fair skin types (Fitzpatrick classification I and II) to two months in patients with darker skin types (Fitzpatrick classification III to V). The preparation consisted in using retinoic acid 0.025%, hydroquinone (2 to 4%) sunscreen SPF 25.
Every patient received acyclovir and antibiotics (cephalosporin) 48 hours before the procedure, which were maintained for 7 days after the laser procedures, as preconized by many authors(6).
Patients who had full facial resurfacing received 4 mg of intravenous dexamethasone (Decadron) during the surgery and after that, the antibiotic was administered orally for 2 days.
The procedures were done under local anesthesia and sedation was controlled by an anesthesiologist. After antisepsis, all wrinkles and deep sulcus were marked with blue methylene. Anesthetic nerve blocks were performed (supra and infra-orbital, nasociliar, mentonian, maxillary at their origin and cutaneous branches of cervical plexus), and were complemented with local anesthesia where nerve blocks do not work. We used lidocaine 2% for the nerve block and lidocaine 2% associated with Marcaine 0.5% in epinephrine solution 1:400000. Tetracaine eyedrops were also used. During the laser resurfacing and the laser blepharoplasty the globe was protected using an eyeshield.
Full face laser resurfacing was done in 78 patients alone or associated with surgical procedures as: superior blepharoplasty, inferior transconjunctival blepharoplasty, canthopexy and facial lipoinjection. In 87 patients, the laser was associated with rhytidectomy at the same surgical time. In these cases, the rhytidectomy was done undermining the cutaneous flap associated with SMAS-platysma flap. Laser resurfacing was also applied over the neck with less energy and in one pass only. In 15 patients, laser was regional, mainly perioral and periorbital, and 20 patients had other pathologies treated, like nevi, warts, etc.
All surgical procedures were done before resurfacing. The treatment started with laser on the wrinkle margins previously marked ("shoulders") with 500 mJ, 10 W, ultrapulse and CPG off. Then, the treated area was cleaned with saline solution, to remove the vaporized epidermis. After that, we did 2 passes with 300 mJ, 60 W, CPG 396 on nasal and frontal areas, lips and c11eeks; 2 passes with 175 m], 30 VV; CPG 366 on the eyelid . On the neck and undermined skin flap we used 175 mJ, 30 W, CPG 396, one pass. The area was cleaned after each pass.
All laser-treated areas were covered with a clear film dressing impregnated with silicone gel (Silon TSR, Bio-Med Sciences, Bethlehem, PA, USA) and changed whenever necessary, mostly on the third postoperative day and kept until the 7th or 8th postoperative day. On exposed areas, where Silon could not protect, as perioral or lower neck, vaseline was daily used.
After this time, patients used neutral hydrating creams, hydrocortisone creams for itching and erythema and sunscreen for sunlight protection and social exposure. In the first month, the skin was more sensitive and erythematous, followed by a hyperpigmentation that must be prevented and/or treated. For this reason clarifying topical treatment should begin in the first postoperative month. After 1 month, glycolic acid 8% and hydroquinone 2 to 4% was applied until tl,e hyperpigmentation diminished. Association with kojic acid was done when necessary.
Patients were advised to avoid sun exposure for 3 to 4 months.
Biopsies were done in the upper eyelids and in the preauricular region in 10 consecutive patients for histological study.
On the upper eyelids we used 175 mJ, 30 W, CPG 366, 2 passes and on the preauricular region, 300 mJ, 60 W, CPG 396, 2 passes. We used these same parameters of the laser for all biopsies.
RESULTS
Figure 1 shows that among 200 patients, 78 (39%) were submitted to full face laser resurfacing (FFLR) associated to surgical procedures like blepharoplasty, canthopexy and endoscopic brow lift, face lipoinjection, rhinoplasty, etc; 87 patients (43%) had rhytidectomy with FFLR, also including the procedures above; 15 patients (8%) had regional laser resurfacing, mostly perioral and periorbital; and in 20 cases (10%) laser treatment was done over different areas like back of the hands, and also in nevi and warts of the face and in other areas of the body.
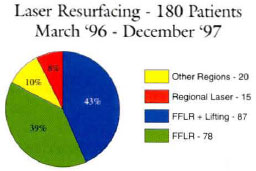
Fig. 1 - Patient's distribution according to the technique employed.
Table I shows each procedure done at the same surgical time as the laser. Out of 180 patients, 165 were submitted to FFLR and 15 were submitted to regional facial laser.
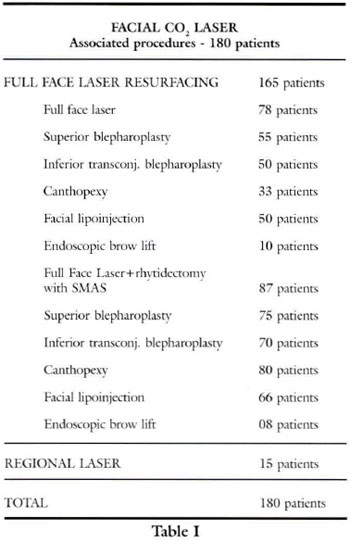
The surgical procedures were done isolated or in association with superior blepharoplasty plus lipoinjection or superior blepharoplasry plus inferior transconjunctival blepharoplasty, etc. Canthopexy with Flower's technique(5) was mostly performed in association with face and neck lift because these patients were older than those submitted to laser only. When a light level of inferior eyelid flaccidity is present (positive SNAP test) it is an indication, from our point of view, of prophylactic or therapeutic canthopexy.
Figure 2 shows the personal satisfaction rate in 180 patients. It shows that in 105 patients (58%) the results were beyond expectation, being these patients extremely glad with surgical outcome 6 months after the surgery. These cases were associated with face and neck lift or endoscopic browlift or other procedures; 54 patients (34%) had good results, with complaints of some wrinkles reappearance (expression wrinkles), treated later with botulinum toxin(7). In 18 patients (10%) the results were considered regular, due to postoperative complications, return of some wrinkles, persistent localized hyperchromy and reappearance of some acne scars; 3 patients (2%) with severe acne scars considered their results poor and another lasertherapy was indicated.
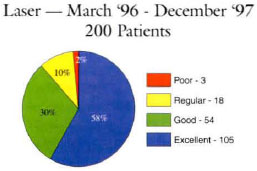
Fig. 2 . Personal satisfaction of patients submitted to laser resurfacing.
Studies have been done to define the CO2 laser histological action over the skin(14)
Biopsies were done in 10 patients, in two specific areas: superior eyelids and preauricular area. We used in all this patients the same laser parameters.
On the eyelids where there was minimal collagen basophilic degeneration in papillary dermis, right after the treatment (175 mJ, 30 W, CPG 366, 2 passes) a complete coagulation occurred until the transition level between papillary and reticular dermis, completely vanishing photoaging of this area (figs. 3 and 4).
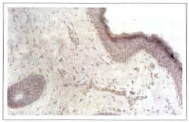
Fig. 3 - Eyelid skin histology with minimal collagen basophilic degeneration, in the papillary dermis. Applied 175 mJ, 2 passes.
Fig. 4 - Eyelid skin histology after CO2 laser with complete coagulation of the degenerated basophilic collagen area. The coagulation area extends until the papillary dermis/reticular dermis transition (double arrow).
Histology of preauricular area where collagen basophilic degeneration was shown down to the transition papillary/supelficial reticular dermis, which means Fitzpatrick I and II or a previously well prepared skin, after 2 passes using 300 mJ, 60 W, CPG 396, there was complete coagulation of collagen basophilic degeneration until superficial reticular dermis (figs. 5 and 6).

Fig. 5 - Preauricular skin histology with minimal collagen basophilic degeneration down to the papillary dermis/reticular dermis transition. Applied 300 mJ, 2 passes.

Fig. 6 - Preauricular skin histology after CO2 laser application, with complete coagulation of the collagen basophilic degeneration area. The coagulation area extends to the superficial reticular dermis (double arrow).
In cases where skin presented a collagen basophilic degeneration down to the deep reticular dermis; that is, severe photoaging, skin inadequately prepared or Fitzpatrick III to V, using the same parameters, basophilic degeneration was not completely treated. Only the superficial reticular dermis was reached, so that collagen basophilic degeneration still lasted (figs. 7 and 8).
Fig. 7 - Preauricular skin histology with intense collagen basophilic degeneration (D), extending until the deep reticular dermis; applied 300 mJ, 2 passes.
Fig. 8 - Preauricular skin histology after CO2 laser application, with coagulation of only a part of the collagen basophilic degeneration. This area goes down to the superficial reticular dermis (double arrow), but the collagen actinic lesion area is deeper (D).
DISCUSSION
We consider laser resurfacing an excellent method for facial rejuvenation. A good result depends on the right indication and adequate managenlent.
The surgeon should always keep a good relationship with the patient, providing every possible explanations on the preoperative period, and all necessary team attention on the first postoperative month, when the patient is very vulnerable psychologically due to the aesthetic aspects. That is why the attentions must be reinforced.
We advise full face laser resurfacing (82%) for most patients rather than regional laser resurfacing (8%), in order to facilitate the postoperative c1arifying treatment.
Undoubtedly, CO2, laser(l4) presents great effect on elastic fiber and collagen at the reticular dermis level, offering good results in deep wrinkles.
In our histological studies we observed that the patients with Fitzpatrick skin type I and II did not present deep collagen basophilic degeneration and that treatment parameters were enough to obtain the total vanishing of the photoaged skin with CO2 laser treatment. Patients with Fitzpatrick skin with III to V, who presented deep collagen basophilic degeneration, dle usual parameters were not enough to completely eliminate the photoaged skin wid, CO2 laser.
The collagen basophilic degeneration suffers complete coagulation down to the transition of papillary/reticular dermis on the eyelids and down to the superficial reticular dermis on the preauricular area, that is the coagulation process doesn't reach the appendage layer in me deep reticular dermis, completely vanishing the photoaged skin from the treated areas as far as the parameters above are observed.
The biopsy parameters observed show us that with 175 mJ the coagulation process reached the transition papillary dermis/superficial reticular dermis. With 300 mJ the coagulation process reached the superficial reticular dermis, without damaging the deep reticular dermis appendages.
We can conclude that in patients with higher degree of photoaged skin, we can go deeper with the laser or we must prepare their patients' skin for longer during the preoperatory period so that best results are obtained.
It was also noticed that FFLR associated with other procedures as blepharoplasty, canthopexy, endoscopic browlift, face and neck lift, lipoinjections, lead to better results and personal satisfaction if compared to isolated or regional use of laser (figs. 9 to 20).
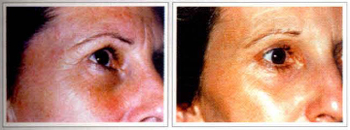
Figs. 9 & 10 - Female patient, 48 years, with glabella and eyelid wrinkles (left). Same patient, 1 year after FFLR associated with endoscopic brow lifting, superior blepharoplasty and canthopexy (right).

Figs. 11 & 12 - Female patient, 72 year, with full face flaccidiry (left). Same patient, 1 year after FFLR associared with face and neck lifting, SMAS-platysma, superior blepharoplasty, inferior transconjunctival blepharoplasty, canthopexy and lipoinjection of the nasal sulcus (right).

Fig. 13 - Same patient of fig. 11, close up of the eye1ids.
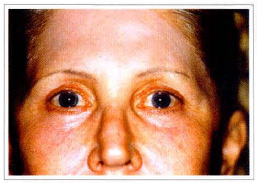
Fig. 14 - Same patient, 1 year after the treatment.
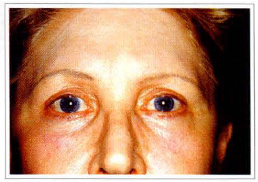
Fig. 15 - Same patient, 1 year and 10 months after the treatment.

Fig. 16 - Patient of fig. 11, close up of perioral region.

Fig. 17 - Same patient, 1 year after treatment, showing improvement of the facial flaccidity and perioral wrinkles.

Fig. 18 - Same patient with maintained result, 1 year and 10 months after the treatment.
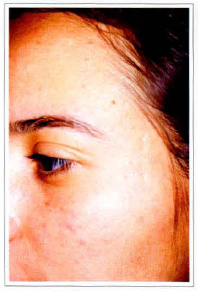
Fig. 19 . Female patient, 17 years, presenting acne scars.
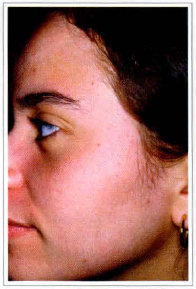
Fig. 20 . Same patient, 1 year later, after FFLR.
We had as complications 2 cases of localized bacterial infections treated with topic therapy (figs. 21 and 22); one case of fungic infection treated with fluconazole (100 mg, for 7 days) associated with topic therapy and 8 cases of contact dermatitis in the first postoperative month related to hypersensitivity to the chemical agent, or hydroquinone allergy, solved by changing active cream agents. The erythema disappeared in all cases in 3 or less months and hyperchromy was treated with clarifying creams for 3 to 5 months. There were no cases of intense hypochromy and clarifying creams were suspended as soon as the skin reached a natural color, because prolonged utilization can lead to unrecoverable hypochromy. Some patients presented strips of hyper and hypopigmentation on the mandibular area of difficult treatment (fig. 23).

Fig. 21 - Complication after CO2 laser. Patient 10 days PO, presenting local bacterial infection in the frontal region.

Fig. 22 - Same patient, 21 days after CO2 laser, with total improvement of the lesions without sequela.

Fig. 23 - Patient with hyper and hypopigmentation on the mandibular area, 4 months after CO2 laser.
All patients were previously treated with acyclovir and antibiotics (Cephalosporin) 48 hours before and 7 days after the procedure, to reduce complications like herpes and bacterial infections.
Before beginning practicing with CO2 laser for facial rejuvenation, a plastic surgeon needs a good training period with laser experient teams. After that, a good patient selection is fundamental, starting with Fitzpatrick I to III, and also with no traces of psychological disturbs. In the first postoperative week all team attentions are necessary until the first and second postoperative month. The surgeon in charge of the patient should keep a close follow up of the dermatological reactions, changing products as needed.
REFERENCES
1. APFELBERG, DB. Ultrapulse Carbon Dioxide Laser with CPG Scanner for Full-Face Resurfacing for Rhytids, Photoaging and Acne Scars. Plast. Reconrtr. Surg. 1997; 99(7):1817-25.
2. ALSTER, TS: Treatment of Facial Rhytides with a High-Energy Pulsed Carbon Dioxide laser; Plast. Reconstr. Surg. 1996; 98(5):791-4.
3. FITZPATRICK, RE et a1. The Depth of Thermal Necrosis Using the CO2 laser. A Comparison of the Superpulsed Mode and Conventional Mode. J. Dermatol. Surg. Oncol. 1991; 17:340-9.
4. _. Depth of Vaporization and Residual Thermal Damage Using Multiple Passes of the Ultrapulse CO2 laser, lasers. Surg. Med. 1997; 21(9):31-8.
5. FLOWERS, RS. Canthopexy wirh Aesrheric Blepharoplasty. In: ANNUAL MEETING OF THE AMERICAN SOCIETY FOR AESTHETIC PLASTIC SURGEONS, 1983.
6. HOEFFLIN, SM. Preoperative and Postoperative Care for laser Resulfacing Patients. Aesthetic Surg. 1996; 16(4):232-4.
7. MATSUDO, PK. Botulinum Toxin for Correction of Fronto-glabella Wrinkles: Preliminary Evaluation. Aesth. Plast. Surg. 1996; 20:439-441.
8. MC DANIEL, DH et al. The Erbium Yag Laser: A Review and Preliminary Report on Resurfacing of the Face, Neck and Hands. Aesth. Surg. 1997; 17(3):157-64.
9. NATHAN, M, FELDER, DS. CO2 laser Resurfacing over Facial Flaps. Aesth. Surg. 1997; 17(5):285-92.
10. ROBERTS III, TL et al. CO2 Laser Resurfacing: Recognizing and Minimizing Complications. Aesth. Surg. 1996; 16(2):142-8.
11. _. Aesthetic CO2 Laser Surgery: Evaluation of 907 Patients. Aesth. Surg. 1997; 17(5):293-303.
12. RONCATI, C and TUNDISI, M. "Resurfacing" com o Ultrapulse-Laser; Nova Arma no Rejuvenescimenro Facial; Rev. Bras. Cir. Plast. 1996; 11(2):69-73.
13. ROSEMBERG, GJ et al. Treatment of Post Laser Resurfacing Complications - Panel Discussion. Aesth Surg. 1997; 17(2):119-23.
14. STUZIN, JM. et al.: Histological Effects of the High-energy Pulsed CO2 Laser on Photoaged Facial Skin. Plast. Reconstr. Surg. 1997; 99(7):2036-50.
15. WEINSTEIN, C and RAMIREZ, O. Complications of Carbon Dioxide Laser Resurfacing and the Prevention. Aesth Surg. 1997; 17(4):216-25.
I - Titular Member of the Brazilian Society of Plastic Surgery, Member of the Scientific Committee of the Brazilian
Society of Plastic Surgery, Section of Paraná, Guest Professor of the Evangelic University of Cuririba.
II - Associate Member of the Brazilian Society of Plastic Surgery.
III - Resident, Plastic Surgery, Evangelic University of Curitiba.
IV - Pathologist, Member of the Brazilian Society of Pathology.
Address for Correspondence:
Ruth Graf, MD
R. Solimões, 1184
80810-070 - Curitiba - Paraná
Brazil
Phone: (55 41) 335-7237 - Fax: (55 41) 335-9394
e-mail: hansgraf@bsi.com.br


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter