

Articles - Year 1998 - Volume 13 -
Health Risks of Ultraviolet Radiation
Riscos à Saúde da Radiação Ultravioleta
ABSTRACT
Ultraviolet radiation in sunlight is critical for vitamin D synthesis in the skin and other physiological aspects of our lives. However, it produces a variety of pathologic effects, including sunburn, pigmentary change, immunologic alterations, and neoplasia. A constellation of structural alterations of the epidermis, the dermal-epidermal junction, and the dermis is uniquely characteristic of photo-damage. It has its influences in plastic surgery, such as photoaging, facial peeling, hyperpigmentation of scars. As we know, the only protection from atmosphere we have is being destroyed everyday by man and his evolution, and that is why the exposure to ultraviolet radiation without appropriate protective measures can be very damaging to our skin and health. UVR induced changes can be minimized or prevented by the use of proper clothing, appropriate application of physical and/or chemical sunscreens, behavior modification, and awareness of photosensitizing medications. The goal of this review article is to understand the deleterious effects of sun exposure and how to prevent them, as well as the cultural, economical, and educational changes we'll need to go through in view of the new atmosphere.
Keywords: ultraviolet radiation; skin cancer; photoaging; photoimmunology; plastic surgery; prevention.
RESUMO
A radiação ultravioleta da luz solar é crucial para a síntese de vitamina D na pele e em outros aspectos fisiológicos da vida humana. Entretanto, ocasiona uma variedade de efeitos patológicos, como queimaduras, mudanças de pigmentação da pele, alterações imunológicas e neoplasias. Uma série de alterações estruturais na epiderme, na junção dermo-epidérmica e na derme são características singulares e exclusivas do dano solar. Isso corresponde a influências na Cirurgia Plástica, como o envelhecimento causado pelo sol, "peeling" facial e hiperpigmentação de cicatrizes. Como se sabe, nossa única proteção na atmosftra contra os raios ultravioleta está sendo destruída dia a dia pelo homem e sua evolução. Por isso, a exposição à radiação ultravioleta sem meios adequados de proteção pode ser danosa à pele e à saúde. As alterações induzidas pela radiação ultravioleta podem ser atenuadas ou evitadas com o uso de roupas apropriadas, uso adequado de barreiras químicas e/ou físicas, mudanças de hábitos e cautela no uso de medicamentos fotossensibilizantes. O objetivo deste artigo é compreender os efeitos deletérios da exposição à luz solar e como preveni-los, e avaliar as mudanças culturais, econômicas e educacionais a serem implementadas tendo em vista a nova atmosfera.
Palavras-chave: radiação ultravioleta; câncer de pele; fotoenvelhecimento; fotoimunologia; cirurgia plástica; prevenção
Sunlight and ultraviolet radiation (UVR) from artificial light sources can be tonic or toxic to human skin. It is unthinkable that radiant energy from the sun is not intricately woven into our life processes as other omnipresent environmental factors are, such as air and water. The sun is necessary for life. We are warmed by its rays and we are able to see it with the eyes that respond to the visible light portion of the solar spectrum (400 to 760 nm).
The health promoting qualities of sunlight have been acknowledged since ancient times. In the twentieth century natural light and UVR from artificial sources have always been recognized for their tonic value and endowed with health-giving powers, a feeling that light is good for our psyche, for the synthesis of vitamin D, and for generating a "healthy" tan to enhance the photoprotective properties of melanin in our skin. Yet, excessive exposure to this life-supporting radiation without appropriate protective measures can be very damaging to skin in those individuals whose natural photoprotective defenses are poor(21).
The exposure of skin to solar ultraviolet light is a growing problem in the world because of the increasing population of the sunbelt, the increasing number of vacations being taken in warmer areas, and the popularity of sunbathing, tanning salons, and outdoor sports. The greater life expectancies in most industrialized countries will also raise the lifelong exposure of many people to the sun(5).
The deleterious effects of UVR depend upon the length (duration) and the frequency of exposure, the intensity of solar radiation based on the latitude of the location from the equator, and the reactivity of the skin based on genetically determined constitutive skin color and skin photo tvpe. For a normal fair-skinned healthy person, there are five concerns about the harmful effects of sun exposure:
1. The acute effects (sunburns, drug induced phototoxicity).
2. The potential long-term risk of repeated uncontrolled sun exposures resulting in the development of actinic changes or dermatoheliosis (wrinkling, premature aging of the skin, irregular thinning of the epidermis, telangiectasia, hyperpigmented maculas.
3. The development of pre-malignancies (solar keratoses) and malignancies, both non-melanomas (basal cell and squamous cell carcinoma) and melanomas.
4. The consequence of cumulative photochemical damage to unprotected eyes resulting in yellow-brown coloration of the lens (aging of lens) and nuclear cataract formation.
5. The alteration of the immune responses and of the function and distribution of components of the immune system causing a selective immune incompetence.
There are over 40 human skin diseases that are either caused or aggravated by sun exposure, such as genetic diseases (xeroderma pigmentosum, albinism), metabolic diseases (porphvries), drug-induced phototoxic and photoallergic or photoinmmunologic diseases, degenerative or neoplastic diseases, as well as several other processes, such as solar urticaria, lupus erythematosus and more.
The ability to modify sunlight and therefore to decrease the chances of carcinoma in patients prone to sunburn should be understood by all physicians.
The goal of this article is to understand the deleterious effects of the sun exposure and how to prevent them, as well as to discuss the cultural, economical and educational changes that are necessary to be done in view of the new atmosphere.
HISTORICAL ASPECTS
Man's relative hairlessness and thin skin indicates his tropical origins. No one knows what was the skin color of the first humans. Most scientists believe, however, they were dark-skinned and that skin emerged later as man migrated to less tropical regions, where colder climates forced them to wear more clothing. The wide variety of human skin color is a direct measure of me diverse climates man has come to know. The distribution of light skin in regions that receive little UVR and darker skin in regions that receive more generally holds true around the world.
The skin cancer has been on the rise since the 1940's when tanned skin came into fashion. For centuries, aristocratic women prided themselves on a lily-white complexion. Tanned skin was the mark of the worker who labored outdoors. Women carefully guarded their faces from the sun with large hats parasols. But nothing changes if not fashion. With the popularity of seaside resorts, sports and other leisure pursuits after World War II, tanned skin became desirable, an enviable vacation souvenir. For those with dark skin, tanning was a relatively harmless pastime. But for light-skinned people, sunbathing became a risk, for they were exposing their skin to amounts of sun nature had not properly equipped them to handle.
SOLAR RADIATION AND ITS PHYSIOLOGICAL ACTION
The ultraviolet radiation occupies the region of the electromagnetic spectrum between visible light and X-rays. It can initiate photochemical reactions in the skin This process occurs when vitamin D3 is produced. The full impact of UVR on human health is difficult to quantify (fig. 1).
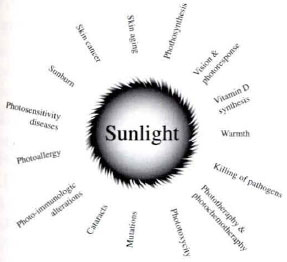
Fig. 1. Sun and its health effects.
The UV spectrum is classified as the region between 200 and 400 nm. The region between 400 and 320 nm, the so-called "black light" region, is called UV-A and is responsible for pigmentation of the skin, or suntanning.
The region between 320 and 280 nm is called UV-B, the erythema region. Most of the biologically active and potentially harmful UV from natural sources fall within this range.
The region between 280 and 220 nm is called UV-C region and is noted for its bactericidal and germicidal effect. The UV-C region occurs in the light of germicidal lamp and some welding arcs, but not in the sunlight at me surface of the earth.
The region between 220 and 170 nm is me most efficient wavelength range for me production of ozone. The UVR in this wavelength range is strongly absorbed by air.
By far the most common exposure to me UVR is from direct sunlight. Solar irradiation exhibits a broad spectrum of UVR, both in intensity and wavelength. Fortunately, the surface of the earth is shielded by the atmosphere, otherwise, solar UVR would probably be lethal to most living organisms on earth. Many factors affect the actual dose of UV received by humans, including:
- altitude above sea level;
- geographical latitude;
- time of me year;
- presence or absence of dust and pollution.
Practically no UVR from the sun with wavelength below 290 nm reaches the earth surface, primarily due to atmospheric filtering.
THE OZONE LAYER
Filtering of wavelengths less man 290 nm by ozone is a very important process because the shorter UV wavelengths are highly damaging to animals and plants. In the upper atmosphere ozone is fonned by photochemical processes. Ozone is present in the stratosphere mainly between 15 and 35 km above the earth's surface and it is constantly being generated and degraded(12).
Unfortunately, with the evolution we're having losses in the ozone layer and these can be produced by several forms of air pollution, through complicated chemical and photochemical processes in the stratosphere, nitric oxides from stratospheric aviation, nuclear bombs, and chlorine from photodissociation of chlorofluoromethanes (Freons in aerosol, propellants and refrigeration devices) produce catalytic losses in the ozone layer.
Because the transmission of solar UVB through the atmosphere varies exponentially with ozone concentration, small changes in me ozone layer may result in hazardous increases in UV irradiuance at the earth's surface. As an example, recent calculations indicate that a 1% decrease in atmospheric ozone is expected to increase the incidence of non-melanoma skin cancer by 2.7%.
The 1992 global average total ozone, measured by the Total Ozone Mapping Spectrometer (TOMS) on the Nimbus-7 satellite, was 2 to 3 percent lower than any earlier year observed by TOMS (1979 to 1991). Ozone amounts were low in a wide range of latitudes in both the Northern and Southern Hemispheres, and the largest decreases were in the regions from 10ºS to 20ºS and lOºN to 60ºN(8).
PHOTOIMMUNOLOGY
Photoin1munology is the study of the effects of ultraviolet radiation (UVR) on immunologic processes. It is now known that the skin functions not only as a protective barrier but is an important part of the immune system. The immune responses originating in the skin corresponds to the SALT (skin-associated lymphoid tissues) concept. According to this concept, the skin contains antigen presenting cells called Langherhan cells (LC) that are capable of communicating with T lymphocytes. In addition, depending on their state of activation, keratinocytes produce a number of cytokines that may also participate in immune recognition in the skin(10). Epidermal cytokines produced by keratinocytes include interleukins, colony stimulating factors, and tumor necrosis factor-alpha.
UVR leads to a functional impairment of SALT through ways that are not yet completely understood. It is clear that UVR alters the ability of LC to present antigens effectively to T cells. UVR also causes keratinocytes to increase production ofc)'tokines (ILl, IL-6, TNF) and induces d1e release of immunosuppressive factors which can lead to a progressive spread of infectious and/or neoplastic processes affecting the skin.
THE SUN AND ITS SHORT TERM HEALTH EFFECTS
Functionally two groups of health effects can be described, those related to acute, direct exposure and those that appear over protracted periods in which there is increased risk to health. Acute effect due to direct UV exposure vary with dose and due to the limited penetration of UV into the tissue, the principle short-term effects are restricted to the skin and eyes(l5).
Dermatological
Immediate changes in the skin occur in a sequence of events including quick darkening of cellular pigment, the occurrence of erythema (sunburn), production and migration of melanin granules (suntanning), and changes in the cell growth in the epidermis. The skin pigment, melanin, is directly and immediately affected by UVR.
Erythema, also occurring soon after initiation of UV exposure, is a vascular reaction that consists of vasodilation and augmented blood flow. The extent and severity of this reaction is highly variable, depending on the skin properties (transmission of UV through the epidermal layers) and the wavelengths of UV received.
"Suntanning" occurs over a slightly longer period than erythema, however the process has a similar action spectrum. This increase in pigmentation occurs both because of increased production of pigment granules and the spread of granules more uniformly throughout epidermal cells.
Another short-term effect of sun exposure is the recurrent facial-oral herpes simplex. It is estimated that one-third of the population of the United States experience recurrent episodes of facial-oral HSV, known as recurrent herpes labialis or cold sores. The most common triggering events to bring on recurrent cold sores are sun exposure, trauma to lips, emotional stress, and fatigue.
The final short-term effect on the skin is a change in the growth patterns of epidermal cells. After short-term slowing of growth there is an increase that gives rise to hyperplasia in the epidermis with a concomitant shedding of cells form the skin surface.
Ocular
Although a small amount of UV may no produce permanent injury to the eyes, the only safe procedure to follow is to exclude completely all harmful levels of exposure. The elimination of harmful UVR must be given attention, because it can do great injury to the eyes without causing discomfort during exposure. The potential for strong UV sources (for example, lasers) to cause irreversible damage to ocular structures is of particular concern.
It is only after damage has been done (some 4-6 hours later) that the effects can begins to appear in the form of conjunctival irritation. Effects on the eye consists of photokeratitis and conjuctivitis. These clinical effects are caused primarily by UVB and UVC irradiation.
Late effects may also occur after prolonged exposure to UV sources, natural or synthetic. These can consist of decreased elasticity in the skin giving the appearance of premature aging, or certain types of cataracts may increase. The dose-response relationships of these phenomena are unknown. Of greater concern is the increased risk of cancer particularly of the skin, in people exposed to UVR.
THE SUN AND ITS LONG TERM HEALTH EFFECTS
Lentigo solar
"Liver spots", "les medallion de cimetiere", sometimes called "coffin spots", are actinically induced and therefore should not be called senile lentigo. The appropriate term is solar lentigo. The lesion may be present on UVR exposed skin in more than 90% of Caucasians over 70 years of age. Lesions are flat, have uniform brown color, and are especially prominent on the dorsum of the hand of photodamaged older persons. The maculas are usually larger than 1 cm, are multiple, and have circumscribed well-defined round borders. Histologically, epidermal rate ridges are elongated with increased numbers of benign melanocytes(16).
Cutis Rhomboidalis Nuchae
This is an example of the profound textural and pigmentary changes thar can occur on the neck of chronically sun exposed person. Coarse furrows lie in crisscross fashion dividing thickened, leathery, ruddy-colored skin.
Favre-Racouchot Disease
Also known as nodular elastosis with cysts and comedones, occurs on facial sun exposed skin and is characterized by huge open comedones (blackheads), predominantly on the temples of some older persons. The follicular orifices are greatly dilated and contain dense impacted horn. Sebaceous glands are atrophic. Dermathoeliosis is the necessary background for the development of solar comedones. The comedones respond to topical retinoic acid.
Solar Purpura (Batema's Senile Purpura)
Purpura frequently occurs following trauma to severely sun-damaged skin of the forearm of elderly persons. Torsional stresses rapidly lead to hemorrhages thar may require months for the blood pigments to be resorbed.
Venous Lake
It is a venous ectasia that appear as a blue-black soft papule, typically on the lower lip and other sun exposed areas such as the helix of the eat, the face and the neck. Dereriorations in the three-dimensional network of connective tissue in both the vascular adventitia as well as the dermis contribute to their development. Venous lakes may be mistaken for melanomas or pigmented basal cell carcinomas. Diascopy is useful in making the diagnosis in which direct pressure created by a glass microscope slide cause a vascular lesion to blanch, thereby differentiating it from a neoplasia(16).
Stellate Scars of the Hands and Forearms
These have been mistakenly attributed to a preexisting purpura. The latter heal without scarring. Stellate scars have been inaptly called pseudo scars (of Coulomb), bur they are true scars resulting form tearing of fragile photodamaged skin.
Chronic Actinic Dermatitis
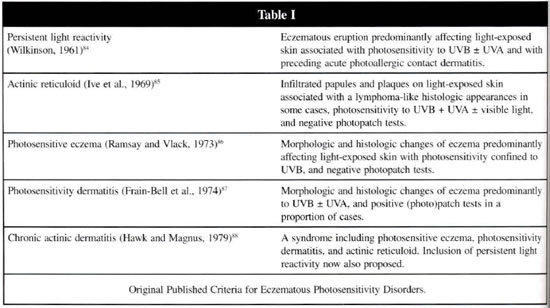
The syndromes of persistent light reactivity, actinic reticuloid, photosensitive eczema and photosensitivity dermatitis, which were defined 15 or more years ago, are now considered as variants of the single condition called chronic actinic dermatitis and is characterized by a persistent eruption of generally eczematous character, possibly associated with infiltrated papules and plaques, predominantly affecting exposed skin, although sometimes extending to covered areas, on occasion, as erythroderma(9) (table I).
Drug reactions
Numerous systemic medications may augment UVR susceptibility. This may occur with the use of oral antibiotics, antihypertensives, psoralens, immunosuppressive agents, nonsteroidal antiinflammatory drugs, and other agents. In addition, a number of topical medications and industrial chemicals may increase the susceptibility to damage by sunlight. These include topical psoralens, tretinoin, and other photosensitizing and depigmentation agents. Some essential oils (bergamot, lime, vanilla, etc.) may cause photoallergy, too. Photosensitivity reaction appears to be more prevalent in older age groups. A pseudoporphyria-like presentation can occur on light exposed areas of patients taking naproxen or furosemide. Thiazide diuretics and sulfonamide-base hypoglycemic agents can cause photosensitivity. The elderly must always be closely questioned regarding drug-intake, in view of age-associated forgetfulness. Resolution of the eruption upon withdrawal of the drug is often prolonged.
Xeroderma Pigmentosum
It is a rare autosomal recessive disease of humans characterized by an accelerated chronic degeneration of sun exposed areas of the body, including an elevated risk of developing cancers of the skin(2).
Solar Urticaria
It is an uncommon condition in which UV or visible irradiation leads to whealing of some or all exposed skin. It is more common in females, between 20 and 40 years of age, and persist indefinitely, occasionally slowly worsening, or gradually improves. Within 5 to 10 minutes of sun exposure, patients experience itching, erythema, and patchy or confluent whealing, which with sun avoidance resolves within 1 to 2 hours(9).
Chronic Discoid Lupus Erythematosus
It is a localized discoid inflamnation of the skin occurring most frequently in areas exposed to UVR. The lesions consist of dusky red, well-localized, single or multiple plaques, 5-20 mm in diameter, usually on the face (butterfly distribution). The external ears, scalp and oral mucous membrances can be involved. There is atrophy, telangiectasia, and follicular plugging. The lesion is usually covered by dry, horny adherent scales.
Photoaging
Given that in many ways our culture promotes deeply tanned skin as a symbol of beauty, health, and even happiness, physicians face an uphill battle in promoting ti,e healthy aspects of a pale complexion. Not only excessive solar exposure can intensify aging in skin, it can also lead to serious health risks. Photoaging denotes the gross and microscopic cutaneous changes that are a consequence of chronic solar radiation.
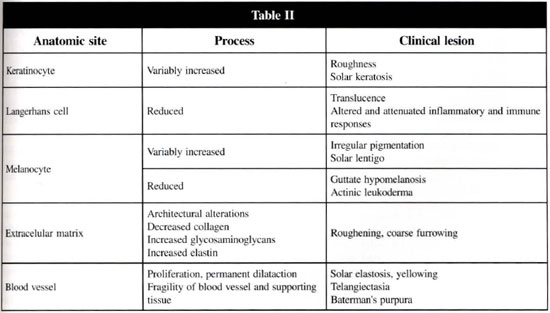
A serious sun worshiper, at age 50, special if skin photo type I (blue-eyed, fair skinned, Celtic ancestry who burn easily and tan poorly) have a plethora ofwrinkles, with yellowed, lax, dly, leathety, knobby, blotchy skin and a variety of benign, premalignant and malignant neoplasms. In contrast, those who scrupulously avoid the sun can reach the ninth decade with smooth, unblemished skin(4) (table II).
At one time photoaging, like aging itself, was considered irreversible. Nowadays, the daily application of retinoic acid typically results within 2-5 days in an erythematous scaling reaction, which lessens with continued usage. Clinical improvements in global appearance, surface roughness, fine and coarse wrinkles, mottled pigmentation, and swallowness were shown after a 10 to 12 months therapy, at least. The beneficial effects were dose-dependent and increased with the duration of the therapy(6). There is no information regarding longterm positive, negative, or toxic effects of this agent. Conflicting data exist demonstrating both prevention and potentiation effects of topical retinoid in the development of UVR induced skin tumors in animals.
Cataracts
The most effective wavelengths for UV-induced cataracts are 290 nm to 310 nm. Cataracts have been induced experimentally with exposures of high intensity/short duration and low intensity/long duration. UVA may be effective in cataract formation, but high values of radiant exposure are necessary and long duration exposures.
Pellagra
It is caused by a lack of niacin. The disease is characterized by four D's: dermatitis, diarrhea, dementia, and death. The dermatitis is precipitated by sunlight and frequently resembles sunburn, but the erythema is prolonged, and pigmentation and desquamation usually follows.
SUN EXPOSURE AND SKIN CANCER
Cancer of the skin is the most common type of neoplasm in countries with predominately Caucasian populations and high levels of ambient solar radiation. The incidence of new cases of skin cancer exceeds 500,000 per year in the United States alone(21). Most skin cancers are thought from chronic exposure of the skin to solar ultraviolet radiation (UVR). The three types of skin cancer related to sun exposure are basal cell, squamous cell, and melanoma. The increasing incidence of skin cancers, including melanoma, has been attributed to increasing exposure of the population to sunlight. During the past century, changes in clothing styles, recreational activities, longevity and other aspects of life-style have resulted in increases in exposure to sunlight.
The wavelengths of solar radiation involved in tumor induction appear to be within the ultraviolet (UV) region of the spectrum (wavelengths between 200 and 400 nm), especially in the UB (290-320 nm) range. Only a small amount a UVB radiations is present in sunlight because wavelengths in this region are strongly absorbed in the atmosphere. UV wavelengths below 290 nm (UVC radiation) are completely absorbed by ozone and thus are not present in natural sunlight. UVA (320-400 nm) makes up 90-95% of ultraviolet energy in the solar spectrum(l2).
Decreases in the stratospheric ozone would cause a corresponding increase in the amount of UVR in sunlight, particularly in the UVB region(4). This may help to explain the rising incidence of skin cancers.
The primary carcinogenic wave band of sunlight falls within the wavelength range between 290 and 320 nm (UVB). This is the primary wavelength blocked by chemical sunscreens. Although UVA appears to be much less carcinogenic, there is very little protection, if any, in most sunscreens against UVA radiation(12). It may be that UVA combined with UVB may accelerate carcinogenesis.
People who are at greatest risk for developing skin cancer are those who spend most of their time outdoors, such as farmers, construction workers, etc. Light-skinned populations who burn easily instead of tanning are at a greater risk than those who have darker pigmentation. There is also an increased incidence of skin cancers geographically as one approaches the equator, suggesting there is a greater intensity of the sun at different latitudes(20).
BASAL CELL
Basal cell cancer (BCC) is a malignant epithelial tumor of the skin that arises from basal cells of the epidermis and its appendages. Its cellular components resemble the relatively undifferentiated, immature cells of the basal layer, and it requires a characteristic stroma.
BCC is the most common tumor affecting light skinned people but it rarely metastasizes(15). Although many BCC arise on areas of the skin that are relatively sun protected such as the scalp and behind the ears, it is widely accepted that UVR is a major etiologic factor in BCC(2). Once a patient has developed a skin cancer, the patient is at increased risk for subsequent skin cancers. Recent studies showed the estimated risk of developing one or more new skin cancers was 35% at 3 years and 50% at 5 years. The new skin cancers tended to be the same cell type as the previous skin cancers(23).
SQUAMOUS CELL CARCINOMA
The cutaneous squamous cell carcinoma (SCC) is a malignant proliferation of the keratinocyte of the epidermis, the most abundant epidermal cell type(9). The SCC usually derives from a precursor, one with partial or in situ changes called actinic keratosis. The majority of SCC occur in light-complexion individuals in skin exposed areas with the lower lip being the principle mucocutaneous site of solar exposure(l6). Although SCC is less common than BCC, the relationship between sun exposure and neoplasia is more direct with SCC than BCC(15). Unlike BCC, invasive SCC can be a rapidly growing tumor with great risk of metastasis. There also appears to be an increased risk of SCC in people who smoke(9).
MELANOMA
Malignant melanoma results in the malignant transformation of melanocytes, usually located in the epidermis, dermis, or mucosal epithelium. Melanoma is the leading fatal illness arising in the skin. Estimates of melanoma caused by sun exposure was 65% in 1985, and the incidence appears to be rising. Out of the several subtypes of melanoma, the lentigo malign melanoma (LMM) has the strongest direct association with sun exposure. This is a variety of intraepidermal melanocytic dysplasia that has the capability of evolving to an intraepidermal (in situ) and invasive melanoma, and because of this it is treated like a melanoma(22).
The manner of skin reaction to sun exposure is an important indicator of melanoma risk. Increased melanoma risk is associated with tendency to sunburn on acute exposure and little or no tendency to tan with chronic exposure(18). The sunburn reaction has been used as an indicator of acute intense insult from UVR, perhaps with a substantial damage to DNA, as well as an overall lack of UV protection. History of sunburn in childhood or adolescence, lifetime numbers of sunburns, and recent severe sunburns have been associated with increased melanoma risks.
Melanoma may suddenly appear without warning, but it may also begin in or near a mole or other dark spot in the skin. When evaluating these areas it is important to remember the ABCD's of melanoma.
- Asymmetry - One half doesn't match the other border
- Border irregularity - The edges are ragged, notched, or blurred.
- Color - Pigmentation is not uniform.
- Diameter - Greater than 6 mm, should concern.
SUN EXPOSURE AND PLASTIC SURGERY
Skin peeling: It must be accepted that with more aggressive peel procedures there will be some change in the skin color. Hyperpigmentation can manifest extremely early, even within the first 2 weeks of the procedure being performed. There are some drugs, such as phenothiazines, psoralen's (particularly in conjunction with UVR), hormones that are capable of producing generalized hyperpigmentation through stimulation of melanogenesis. The sun exposure may precipitate development of hyperpigmentation, and therefore a nonsensitizing sunscreen or sun block should be an essential ingredient in postpeel skin care. It is extremely important that patients be aware of the hazards of sun exposure in the early post treatment state, particularly during the summer months when sun intensity is strongest(l3).
At the first signs of increased pigment formation in the skin, the areas may be treated with a bleach cream compounded as follows:
- Retinoic acid 0,1% cream
- Hydroquinone 4%
- Triamcinolone 0.1 % cream
- Hydrocortisone 2.5% cream
Scars in exposed areas
During the period of scar maturation, approximately the first six months, direct sun exposure of the scar areas has to be avoided. Permanent hyperpigmentation of the scars may occur because of the increased sensitivity of melanocytes and this phase of wound healing.
THE SUN EXPOSURE PRECAUTIONS
It is very important to protect ourselves of the sun induced abnormal reactions. The protection against the adverse effects of UVR on the skin may include the prevention of:
1. Acute sunburn (in fair-skinned individuals),
2. Hyperpigmentation (in dark-skinned) individuals,
3. Acute phototoxic and photoallergic (eczematous) reactions, and
4. Specific disease-oriented responses such as the amelioration of chronic skin damage, as in skin aging and skin cancer(21) .
Skin color and Sun-reaetive Skin photo types
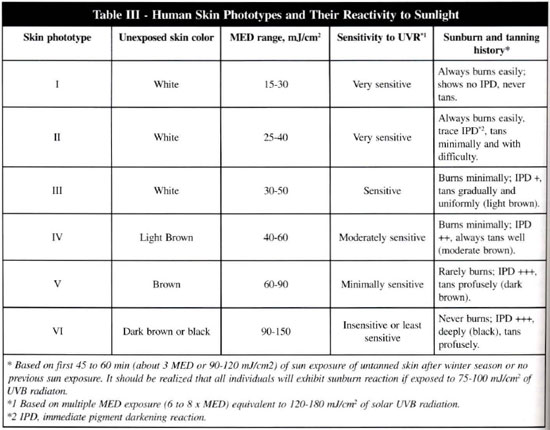
Not all people in the world share an equal risk for the development of skin cancer and changes associated with actinic damage (photoaging) or dermathoeliosis. To identify the white population at high-risk for the development of sun-induced skin changes, a simple working classification has been proposed that is based, not on the phenotype, but on what patients tell us about their responses to an initial sun exposure (table III).
Clothing
Appropriate clothing can provide an optical filter against the penetration of harmful radiation. Hats and umbrellas (parasols) are helpful in minimizing damage to the face and sparsely haired scalps. Broad-brimmed hats protect the ears, nose, and cheeks. The use of appropriated sun glasses are very important. Fair-skinned individuals of SPT I, II and III and patients with xeroderma pigmentosum, erythropoietic porphyria and protoporphyria, and solar urticaria should be strongly recommended to use dlese measures.
Tighter weaves of clothing, preferably colored, tend to allow less radiation to penetrate to the skin. Dark, specially black, clothes are excellent but they absorb the light and infrared radiation and, thus, may be quite uncomfortable. Synthetic materials (polyester fabrics such as nylon, Dacron, etc.) are less transparent to UVB, as well as UVA radiation than cotton fabrics and so are more protective; when examined under UVR, they reveal absorption as well as fluorescence.
Time of the day
The intensity of erythemogenic UVB and UVA rays reaching the earth's surface from the sun is highest between 11 AM and 2 PM. Our skin has no sensors for Jeeling the impact of UV rays as it has for the warnlth of infrared radiation: hence, avoidance of sun exposure between lO AM and 3 PM is the only sensible way to reduce the danger of extensive exposure to such rays.
Topical Sunscreening Agents
The regular use of sunscreens is important for the prevention of dermatoheliosis and skin cancer. When appropriately applied, the chemical and physical sunscreens modify the optical properties of the skin and prevent the deleterious effects of UVB and UVA radiation. By varying the concentration of the active sunscreen agent, topical sunscreens can be formulated in a water-resistant base to achieve the following goals:
1. Screen out either partially or totally UVR impinging on the skin.
2. Inhibit or minimize photochemical and biochemical reactions in the skin responsible for the induction of sunburn reaction.
3. Minimize hyperpigmentation of skin and tanning reaction.
4. Protect the DNA of the viable cells of the epidermis and dermis against the formation of cyclobutyl pyrimidine dimers and chromosomal damage that eventually contribute to mutation and the carcinogenic effects of UVR.
5. Prevent drug-induced photosensitivity reaction and various other types of photodermatoses.
6. Protect epidermal and dermal proteins (keratin, collagen, elastin, enzymes, etc.) against denaturation and the formation of cross-links responsible for photoaging of skin.
7. Modulate alterations of immune function.
Classification
They can be divided into three categories:
1. Chemical sunscreens that function by reducing the amount of UVR that reaches the stratum corneum by absorbing the harmful radiation.
2. Physical sunscreens that function by scattering and reflecting the UV and visible radiation.
3. Combination sunscreens containing two or more UV-absorbing chemicals and UV-scattering agents such as zinc oxide, titanium dioxide, etc. The chemical sunscreens contain para-aminobenzoic acid (PABA) or its derivatives, called PABA esters (either amyldimethyl PABA, also known as Padimate-A and Escalol 506, or octyldimethyl PABA, also known as Padimate-O or Escalol 507), benzophenones (oxybenzene and sulisobenzene), cinnamates (octylmethoxycinnamate and cinoxate), salicylates (homomenthyl salicylate), and anthranilates. The most important quality of a chemical sunscreen is its ability to absorb UVR, defined as extinction coefficient value. The physical sunscreens contain ingredients, particulate in nature, that do not selectively absorb UVR but, when applied as a thin film, primarily reflect and scatter UV and visible radiation because of the size of the particles and the thickness of the film. These include zinc oxide, titanium dioxide, talc (magnesium silicate), magnesium oxide, kaolin, ferrous or ferric oxide, barium sulfate, and red petrolatun. Physical sunscreens are essential for those patients who are particularly sensitive to UVR as well as to visible radiation, and are usually applied to limit areas such as the nose, lips, or the ears.
Patients with vitiligo of the exposed areas should use physical sunscreens with color shades matching the constitutive color of their normal skin. Such sunscreens not only camouflage the vitiliginous areas and provide cosmetic cover-up but protect the amelanotic areas against actinic damage. These physical blockers are becoming more popular, in combination with UVB and UVA-absorbing agents, to provide high SPF values ofthe sunscreen formulation (SPF more than 15). In fact, the sunscreens that exhibit broad-spectrum protection (290 to 400 nm) with high SPF value (=30) contains at least two chemical sunscreen ingredients exhibiting high UV absorption coefficient and one physical sunscreen that scatter and absorbs the UV and near-visible spectrum(1, 10).
Sun Protection Factor (SPF)
The effectiveness of a sunscreen is based on its SPF value. The concept of SPF is based on UV-absorbing properties of a sunscreen and is a quantitative measure of the effectiveness of a sunscreen formulation. The SPF is defined as the ratio of the exposure value of the erythemogenic UV dose needed to produce the minimal erythema reaction through the applied sunscreen product to the UV dose required to produce the same minimal erythema reaction without the topical application of the sunscreen. The higher the protection factor of a sunscreen, the better the product is for protection(22) (table IV).
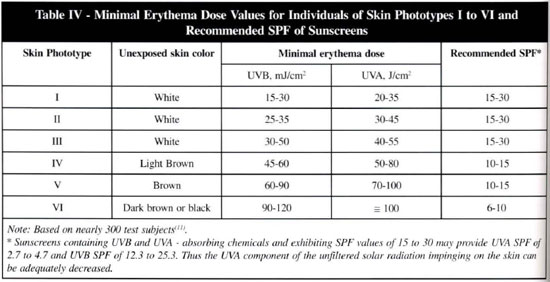
- SPF 2: minimal protection, for people who rarely burn and already have a good tan. Shouldn't be used by fair-skirmed people and children.
- SPF 4: moderate protection, for people who usually tan well and rarely burn.
- SPF 6: extra protection, for people with somewhat sensitive skin, who tan most of the time and seldom burn. Allows some taning.
- SPF 8: maximal protection, for people who burn moderately. Allows limited gradual tanning.
- SPF 15: ultra protection, for blondes, red heads and fair-skinned people. Protects during long periods in the sun. Very slow tanning.
- SPF 23 +: sun blocker, recommended for people who have had a precancerous skin condition. Blocks almost all harmful rays.
Another important property of a sunscreen is its ability to remain on the skin and withstand removal by water and perspiration. "Water-resistant" and "waterproof" are terms used to distinguish these qualities. Water-resistant refers to sun protection maintained following 60 minutes of water immersion, whereas the claim of "waterproof" extends this protection following 80 minutes in the water. Sunscreens can provide this protection by their ability to adhere firmly to the skin or diffuse into the stratum corneum where it can remain absorbed or come conjugated to protein in a manner that can extends its photoprotective abilities during prolonged sunbathing, perspiration, and swimming.
How to recommend topical sunscreens? In table IV, we find some indications for the use of topical sunscreens. In counseling people in the prevention of sunburn, skin cancer, actinic elastosis, and various forms of sun-sensitive reactions, the choice and recommendations of a sunscreen depend upon several factors. The most important considerations should be:
1. Normal individual's skin reactivity to solar radiation after 45 to 60 min. of midday exposure in the early summer: persons of SPT I and II should never indulge in prolonged sunbathing and, for nonsunbathing, they should adopt a program of daily sunscreen application as a regular habit and from an early age.
2. Patient's skin reactivity to UVB and UVA radiation and to chemicals present in the sunscreen: patients with polymorphic light eruption, solar urticaria, lupus erythematosus, chronic actinic dermatitis, etc. react abnormally to UVR; they need to usc broadspectrum sunscreens and physical sunscreens (SPF 15 to 30), preferably without PABA and its esters. Phototesting and contact patch with the prescribed sunscreen may be very helpful to the patient for avoiding any contact or photo dermatitis.
3. The type of environment, intensity of sunlight based on season, proximity to the equator (latitude) and altintde, high and low humidity, snow, wind, and anticipated duration of exposure: it is best to recommend high SPF sunscreens enriched with moisturizers in locations of high-intensity solar radiation, especially while skiing (snow or water).
4. The type of outdoor activity and occupation based on nature of outdoor vs. indoor work, prolonged vs. limited sunbathing, and other activities involving sports-swimming, mountain climbing, etc.
5. Normal individuals skin reactivity ro sunscreens: dermatologists should ascertain or look for evidence of contact sensitivity and delayed hypersensitivity reaction, or any potential for cross-reactivity. Patients with a history of atopic dermatitis are usually sensitive to PABA-related sunscreens and other chemicals.
6. Water-resistant and sweat-resistant properties of sunscreens and their SPF values: sunscreens should be applied uniformly to all the areas of the body that are likely to be exposed (fig. 2).
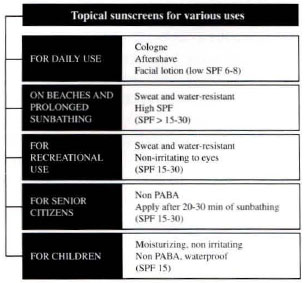
Fig. 2 - Topical Sunscreens for various uses.
Photochemoprotection
A new concept is evolving to achieve better protection of human skin in those individuals who do not like to use sunscreens on a regular base or cannot afford ro buy them. This concept involves the use of topical psoralen (30 parts per million of 5-methoxvpsolaren or bergapten) containing a UVB-absorbing sunscreen (SPF 6 to 8) that in combination with exposure to natural sunlight in low doses can stimulate the production of two natural defense mechanisms: an increase in the thickness of the stratum corneum and the production and transfer of new melanin throughout the epidermis. This method is especially applicable for persons with limited or no competence for tanning (SPT I and II) and who have the lowest concentrations of melanin in the epidermis. Another therapy that can be used for SPT I, II and III people is the topical or oral PUVA (8-MO or 5-MOP and well controlled exposure to UVA radiation). A short course of oral PUVA therapy (twice a week for 3 or 4 weeks) will promote pigmentation and thickening of the stratum corneum and help prevent or ameliorate the development of polymorphous light eruption (PMLE) lesions upon subsequent exposure to sunlight in most patients(21).
Systemic Photoprotection
The development of systemic photoprotectants that could reduce the reaction of skin to sunburn has not been successful. Agents such as PABA, para-amino salicylic acid, antihistamine compounds such as triprolidine exhibiting UV absorption in the 238 to 290 nm range, acetylsalicylic acid, vitamins A, C and E, certain unsaturated fatty acids that easily become photo oxidized, and certain steroids have been suggested as systemic photoprotectants. The effectiveness of many of these agents in preventing UVB-induced sunburn reaction, either totally or partially, has not been evaluated carefully in a controlled, double-blind, study.
Among the few photoprotective agents of limited effectiveness, we will discuss about the beta carotene, a very well-known agent and widely used. Beta carotene is recommended for the amelioration of photosensitivity reactions caused by radiation in the presence of abnormal levels of porphyrins in patients with erythropoietic proroporphyria (EPP), erythropoietic porphyria (EP), and variegate porphyria. EPP is a dominant genetic trait that appears early in chidhood. Unless afflicted patients, especially children, avoid exposure to the sun, a severe photosensitivity reaction will occur with painful swelling, itching erythema, and burning sensation. Vesicles may develop, often leading to scarring and mutilation. Beta carotene is a natural ofmany plants, including common foods such as carrots, tomatoes, green peppers, and oranges; it is non toxic. Only beta carotene, which absorbs radiation in the visible spectrum of light (360 to 500 nm) with a maximum absorption at 450 to 475 nm, has been shown to be partially, if not totally, effective as a systemic photoprotective agent, particularly in patients with EPP who are extremely sensitive to visible radiation.
It is recommended that oral ingestion of synthetic beta carotene to be regulated, to maintain blood carotene levels between 600 and 800 micrograms/100ml (usually a dose of 120 to 180 mg/day for adults). Children under the age of sixteen should receive 30 to 120 mg/day. Beta carotene should be prescribed as follow:
Children: 30 to 60 mg/day for 1 to 8 years old. 90 to 120 mg/day for 9 to 16 years old.
Adults: 120 to 180 mg/day; can be increased to 250 mg/day.
The protective effect of beta carotene for increased tolerance to sun exposure is evidenced after 6 to 8 weeks of therapy Many patients with EPP receiving oral beta carotene are able to develop sun tolerance (up to 30 to 60 min. during summer months) and can, for the first time, engage in outdoor activities for a longer time.
Oral beta carotene is not an effective sunscreen for filtering UVB radiation in sunlight, although it has been shown to slightly increase the MED (minimal erythema dose) in healthy individuals. Patients with very noticeable light sensitivity, as with EPP, congenital porphyria, and xeroderma pigmentosum, should employ photoprotective measures (broadbrimmed hat, long-sleeved clothing, oral beta carotene, and avoidance of sunlight exposure between 10 AM and 4 PM) very early in life. Beta carotene is essentially non toxic and may offer some relief from photosensitivity(2l).
Solar Index
During the past several years, programs to promote public awareness of the possible harmful effects of sun exposure (UVR exposure), the National Meteorological Center of the United States was asked to produce a forecast product. This was to be an index that indicated the general ultraviolet radiation at the earth's surface and allowed the public to gauge their personal exposure. Nowadays, various countries, such as Canada, England, some places in the United States, uses this solar index in their routine weather products and their experience has been very positive with many people actually making changes in their general habits(18).
Four main factors are used to calculate the solar index (UV index): the time of the day, day of year, latinlde for a certain area, and the forecast of tomorrow's ozone layer. The UV index is calculated for clear sky conditions, if the sky is cloudy then an attenuating factor is added. The altimde can also affect the UV index, for each km above sea level there is a 6% increase. There is greater UVR exposure with decreasing latimde and with higher altitude. The greatest UV exposure occurs in June and July in the U.S.A. when the sun is farthest north and the ozone layer is at its lowest level. In South America this occurs in January and February.
The solar index is characterized as follows:
- 0, 1, 2: minimal exposure level
- 3, 4: low exposure level
- 5, 6: moderate exposure level
- 7, 8, 9: high exposure level
- > 10: very high exposure level
Tanning devices
The long-term effects of UV tanning devices are not known, however, these devices have no known health benefits. Therefore persons who choose to use these UV tanning devices should be aware of the potential risks and should follow the manufacture's directions to minimize these risks. Protective goggles should be properly worn. Persons on medications should consult their physicians before using any tanning devices. Most tanning devices producing UVA radiation also emit some UVB radiation. Although UVA radiation is less likely than UVB to cause erythema, it can cause other adverse health effects to the skin, eyes, blood vessels, and immune system as seen above. Some UVA lamps generate greater than 5 times more UVA per unit time than solar UVA radiation reaching the Earth's surface at the Equator.
CONCLUSIONS
After this review about the sun exposure and its harmful effects, we have five approaches that should be recommended to patients and the public in general:
1. Avoid unnecessary sun exposure to harmful ultraviolet radiation between 10 AM and 3 PM
2. Block sunlight; wear protective clothing, broad-brimmed hats, and UV-opaque sun glasses, particularly during peak hours, to prevent cataractogenesis.
3. Cover-up with chemical or physical sunscreens when sun exposure is desired or unavoidable. Recommend sunscreens with SPF 15 and higher; the use of broad-spectrum sunscreens represents as important strategy in the worldwide assault on skin cancers.
4. Do not indulge in prolonged sunbathing or tanning saloons or artificial tanning lamps. Skin tanning induced by repeated exposures to UVA radiation in tanning salons shows minimal photoprotection and in the long term contribures to photoaging changes.
5. Educate children as well as uninformed adults about good sun protection habits at home or in school and examine the skin regularly for moles and other recognizable changes.
The drastic changes required in our sun exposure habits, will be very difficult for the populations in general because of our culture. In a near future, as the ozone layer is being lost everyday, we'll need to have changes in our routine, such as the daily use of sunscreens, the use of UV-reflecting glasses for our cars and homes, and other things that are coming to help us to be sun wise.
Continued efforts need to be directed to the public to increase the acceptability and use of sun protection measures.
REFERENCES
1. ARMSTRONG, BK and KICKER, A. How Much Melanoma is Caused by Sun Exposure? Melanoma - Res. 1993 Dec; 3(6), 395-401.
2. BALES, ES et al. Characterization of Molecular Defects in Xeroderma Pigmentosum Group C. Nat - Genet. ]993 Dec; 5(4), 413-17.
3. BARNHILL, RL el al. Neoplams: Malignant Melanoma. In: FITZPATRICK, TB et al. Dermatology in General Medicine. McGraw Hill. 1993; 1078-111l.
4. BROWDER, JF & BEARS, B. Photoaging: Cosmetic effects of sun damage. Postgrad - Med. ]993 Jun; 93(8): 78-80.
5. DE FRANZO, AJ. Principles and Management of Injuries from Chemical and Physical Agents. In: GEORGIADE, GS et al. Textbook of Plastic, Maxillofacial of Reconstructive Surgery. Willian & Wilkins. 1992; 259-262.
6. FISHER, GJ et al. Cellular Immunologic and Biochemical Characterization of Topical Retinoic Acid Treated Human Skin. J. Invest. Dermatol. 1991 May; 96(5): 699-707.
7. GARLAND, CF et al. Rising Trends in Melanoma. An Hypotesis Concerning Sunscreen Efectiveness. Ann. Epidemiol. 1993 Jan; 3(1): 103-10.
8. GLEASON, JF et a1. Record Low Global Ozone in 1992. Science. 1993 Apr.; 23, 260: 523-526.
9. GRANSTEIN, RD. Photoimmunology. Semin. Dermatol. 1990 Mar; 9(1): 16-24.
10. HAWK, JLM and NORRIS, PG. Abnormal Responses to Ultraviolet Radiation: Idiopathic. In: FITZPATRICK, TB et al. Dermatology in General Medicine. McGraw Hill. 1993; 1661-1667.
11. HOLLOWAY, L. Atmospheric Sun Protection Factor on Clear Days: Its Observed Dependence on Solar Zenith Angle and its Relevance to the Shadow Rule for Sun Protection. Photochem. Photobiol. 1992 Aug; 56(2): 229-234.
12. KARAGAS, MR et a1. Risk of subsequent Basal Cell Carcinoma and Squamous Cell Carcinoma of the Skin Among Patients with Prior Skin Cancer, Skin Cancer Prevention Study Group. JAMA. 1992 Jun 24; 267(24): 3305-331O.
13. KOCHEVAR, IE et al. Photophysics, Photochemistry and Photobiology. In: FITZPATRICK, TB et al. Dermatology in General Medicine. McGraw Hill. 1993; 1627-1635.
14. KOTLER, R. Complications. In: Chemical Rejuvenation of the Face. Mosby Year Book. 1982; 158-217.
15. KRIPKE, ML. Carcinogenesis: Ultraviolet Radiation. In: FITZPATIUCK, TB et al. Dermatology in General Medicine. McGraw Hil. 1993; 797-804.
16. LARGENT, EJ et al. Nonionizing Radiation. In: PLOG, BA et al. FUNDAMENTALS OF INDUSTRIAL HYGIENE. 3. ed. National Safety Council. 1988; 227-235.
17. MARSHALL, B. Skin: the human fabric. In: The Human Body. Torstar Books. 1984: 63-81.
18. MCGEE, R and WILLIAMS, S. Adolescence and Sun Protection. N. Z. Med. J. 1992 Oct 14; 105(943): 401-403.
19. MILLER, AJ and LONG, C. Experimental Ultraviolet Index. National Meteorological Center. 1994 June 21; 1-17.
20. MILLER, G. Ultraviolet Radiation. In: NONIONIZING RADIATION - GUIDES SERIES. American Industrial Hygiene Association. 1991; 1-26.
21. NICOL, NH and FENSKE, NA. Photodamage: Cause Clinical Manifestations, and Prevention. Dermatol. Nurs. 1993 Aug; 5(4): 263-275.
22. PATHAK, MA et al. Preventive Treatment of Sunburn. Dermatoheliosis, and Skin Cancer with Sun - Protective Agents. In: FITZPATRICK, TB et al. DERMATOLOGY IN GENERAL MEDICINE. Mc Graw Hill. 1993; 1689-1715.
23. PATEL, NP et al. Properties of Topical Sunscreen Formulations. J. Dermat. Surg. Onc. 1992; 18: 316-319.
24. RHODES, AR. Neoplasms: Benign Neoplasias, Hyperplasias, and Dysplasias of Melanocytes. In: FITZPATRICK, TB et al. DERMATOLOGY IN GENERAL MEDICINE. McGraw Hill. 1993; 996-1060.
I - Research Assistant at West Virginia University.
II - Associate Professor and Chief of Plastic & Reconstructive Surgery at West Virginia University.
III - Director of the Program "Health and Medicine", Brazil.
IV - Plastic Surgeon, Cruz Alta, Brazil.
V - Medical Student, MS4.
From West Virginia University - School of Medicine
Address for Correspondence:
Julio Hochberg, MD
10 Catalpa St.
Morgantown, West Virginia 26505
USA


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter