

Original Article - Year 2019 - Volume 34 -
Submuscular implant in double pocket for augmentation mastopexy
Implante submuscular em duplo bolso para mastopexias de aumento
ABSTRACT
Introduction: The use of implants is steadily increasing. Reports have been published of implants in the subglandular, subfascial, total, and partial submuscular positions each with its indications, limitations, and complications.
Methods: This study presents a technique to cover the implant and support it using two muscle flaps. Between November 2009 and April 2012, 80 patients who submitted to inclusion of implants in the submuscular position in double pocket were analyzed, regardless of the access route, the degree of flaccidity, and ptosis.
Results: The versatility of this maneuver allows it to be used in a wide variety of breasts, from breast augmentation without flaccidity to mastopexy with implant, and may be carried out via the periareolar, inframammary, or open access routes. It was used in primary and secondary surgeries, with or without the use of breast tissue flap and removal of skin.
Conclusions: The coverage of the implant with the pectoral muscle by the double pocket technique displayed excellent results, with a low rate of complications and reinterventions. This technique is being studied in a larger sample with a longer follow-up to confirm the results obtained so far.
Keywords: Breast implant; Modalities of position; Muscle contraction; Reconstructive surgical procedures; Capsular contracture in implants
RESUMO
Introdução: A utilização de implantes mamários vem aumentando. O posicionamento do
implante na literatura é relatado como subglandular, subfascial, submuscular
total e parcial, cada qual com suas indicações, limitações e
complicações.
Métodos: Este trabalho mostra uma manobra para cobertura do implante e sua sustentação
utilizando dois retalhos musculares. Entre novembro de 2009 e abril de 2012,
foram analisados 80 casos de pacientes submetidas à inclusão de implantes em
posição submuscular em duplo bolso, independentemente da via de acesso, do
grau de flacidez e ptose.
Resultados: A versatilidade desta manobra permite que seja utilizada em uma ampla
variedade de mamas, desde aumento sem flacidez a mamopexia com implante,
podendo ser realizada por via periareolar, inframamária ou aberta. Foi
utilizada em cirurgias primárias e secundárias, com ou sem uso de retalho de
tecido mamário e retirada de pele.
Conclusões: A cobertura do implante com o músculo peitoral pela técnica de duplo bolso
demonstrou ótimos resultados, com baixo índice de complicações e
reintervenções. Esta técnica está sendo utilizada em uma maior casuística e
um seguimento mais longo tem sido feito para confirmar os resultados obtidos
até o momento.
Palavras-chave: Implante mamário; Modalidades de posição; Contração muscular; Procedimentos cirúrgicos reconstrutivos; Contratura capsular em implantes
INTRODUCTION
The inclusion of breast implants is increasingly common in mastopexies, with a wide variety of techniques described for positioning of the implant and breast modelling, to address flaccidity and ptosis.
An accurate preoperative assessment and the choice of the best augmentation mastopexy technique are crucial for good results, with no universal technique used to treat all types of breasts.
In 1960, Gonzales-Ulloa1 reported the use of an alloplastic material with mastopexy for the first time. In 1969, Goulian & Conway2 recommended the use of silicone implants for a repeat surgery after a mastopexy for cases of hypomastia associated with ptosis. The placement of the implant in the submuscular position was initially described by Dempsey & Latham, in 19683.
Mastopexy with a breast implant has a high rate of dissatisfaction, which necessitates reinterventions. However, many authors argue that it is still better than submitting the patient to two surgical procedures: a mastopexy followed by an implant surgery4,5.
A capsular contracture is the most frequent complication associated with mastopexy and implants6,7,8, and may arise anywhere from a few months to a long period of time after surgery, making the breast hard, sore, and deformed (HSD triad) in variable degrees. The cause of capsular contracture is multifactorial 9,10 and is related to an inflammatory reaction caused by an increase in factors such as subclinical infections and irritating factors, with increased cell proliferation associated with the presence of myofibroblasts.
According to Camirand et al.11, muscle contraction over the implant exerts a protective factor which leads to a capsular contracture. In addition to the submuscular planes (total, partial with muscle disinsertion in varying degrees, partial submuscular with dilatation, and construction of a pocket which may be superomedial or inferolateral), a breast implant can be placed in the supramuscular planes (subglandular or subfascial).
There is a layer of loose areolar retromammary fat between the pectoral fascia and the breast capsule (Giraldés ligament or breast suspender and its extensions, Cooper›s suspensory ligaments) called the Chassaignac space, constituting a plane of easy detachment because it is relatively avascular and not very resistant12. The laxity of the Chassaignac space may be responsible for the loss of breast support by promoting its slide in relation to the thorax13.
In order to obtain more harmonious and long lasting results in augmentation mastopexies, we developed an adaptable, reproducible and versatile technique of implant coverage with the pectoralis major muscle, creating a new relation between the breast, the implant, and the pectoralis major and minor muscles, which can be used in cases of mastopexy or even in isolated augmentations.
OBJECTIVE
The objective of this study is to describe the double pocket technique for augmentation mastopexies with submuscular implant and evaluate the preliminary results of this technique.
METHODS
Sample
A retrospective analysis was done for all patients submitted to mastopexy with submuscular implants with the double pocket from November 2009 to March 2012. A total of 80 female patients were operated by the author, with ages ranging from 17 to 54 years, with a mean of 32 years.
All patients underwent a history and physical examination, and were informed of the surgical plan, location and size of the scar, evolution and postoperative care.
All patients received a printed copy, were guided, and signed an informed consent form containing information on the influence of the individual characteristics on the evolution and surgical outcome, the adequacy between expectations and possibilities, and the possible need for surgical replacement to complement the result in the future.
The choice of volume and shape of the breast implant was based on the patient’s preferences during consultation on the placement of molds on the breasts14.
Patients with uncompensated comorbidities, body mass index greater than 35 and smoking more than 5 cigarettes per day were excluded from the study.
Surgical Technique
The need for skin removal and repositioning of the nipple areola complex (NAC) was evaluated with the patients in an orthostatic position to determine and mark reference points.
Photographs were taken of the patients in standardized positions before and after the surgery.
The patients were submitted to intravenous anesthesia with an intercostal or an epidural block and remained in supine position during the surgery, while an anesthesiologist continuously monitored the progress.
Antibiotic prophylaxis, asepsis, antisepsis, hemostasis, and minimal manipulation of the implant were performed.
The technique can be used in a wide variety of clinical presentations; from small breasts without sagging or tuberous breasts, to breasts with large flaccidity and ptosis, as in patients after a massive weight loss.
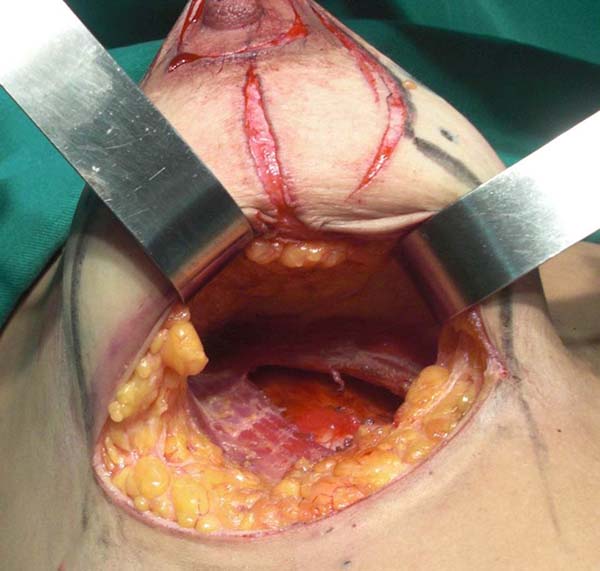
The subglandular detachment was performed through an access route, which varied from periareolar, vertical, or inframammary fold, with partial removal of the Chassaignac space, and identification of the pectoralis major fascia.
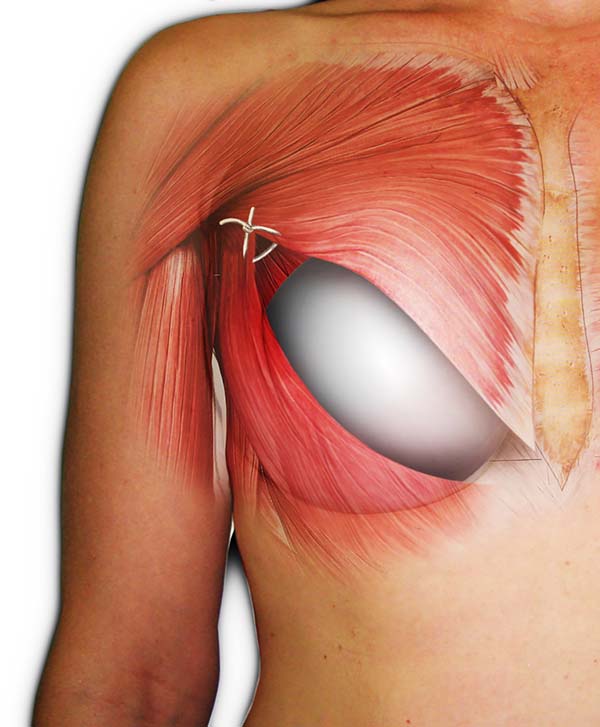
To gain access to the intermuscular plan (between the pectoralis major and minor), a blunt dissection was performed in the direction of the fibers of the pectoralis major, starting from the insertion of the muscle (rib edge) toward its origin, dividing the muscle in two muscular flaps (one superomedial and other inferolateral) (Figure 1) thus preserving the fibers, insertion, vascularization, innervation, and function of the muscle.
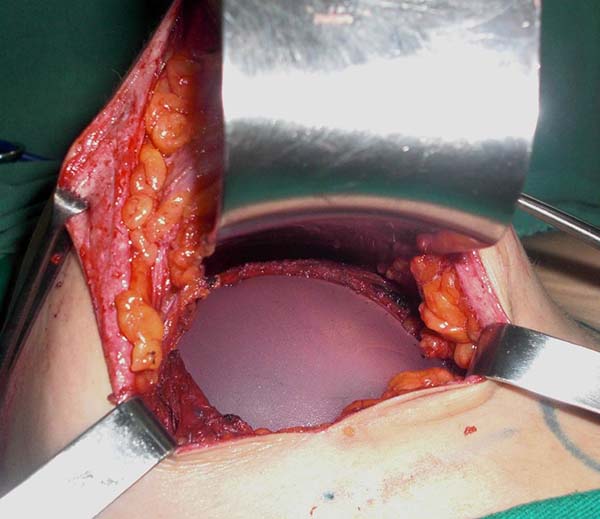
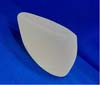
The implant was placed between the two pockets formed between the muscular fibers of the pectoralis major, remaining subglandular only in its anterior portion (Figure 2).
With this technique, the implant was placed on top of the pectoralis minor, covered in its inferolateral and superomedial portions by the pectoralis major, and with the scar capsule formed later on the pectoralis minor, providing stronger adherence to the thoracic wall. On each side the scar capsule was limited by loops formed by the pectoralis major muscle and the anterior portion adhered to the breast capsule. Thus, there was integration between the thoracic wall, the pectoralis major and minor muscles, the parenchyma and the breast implant, through the scar capsule (Figure 3a, 3b, 3c).
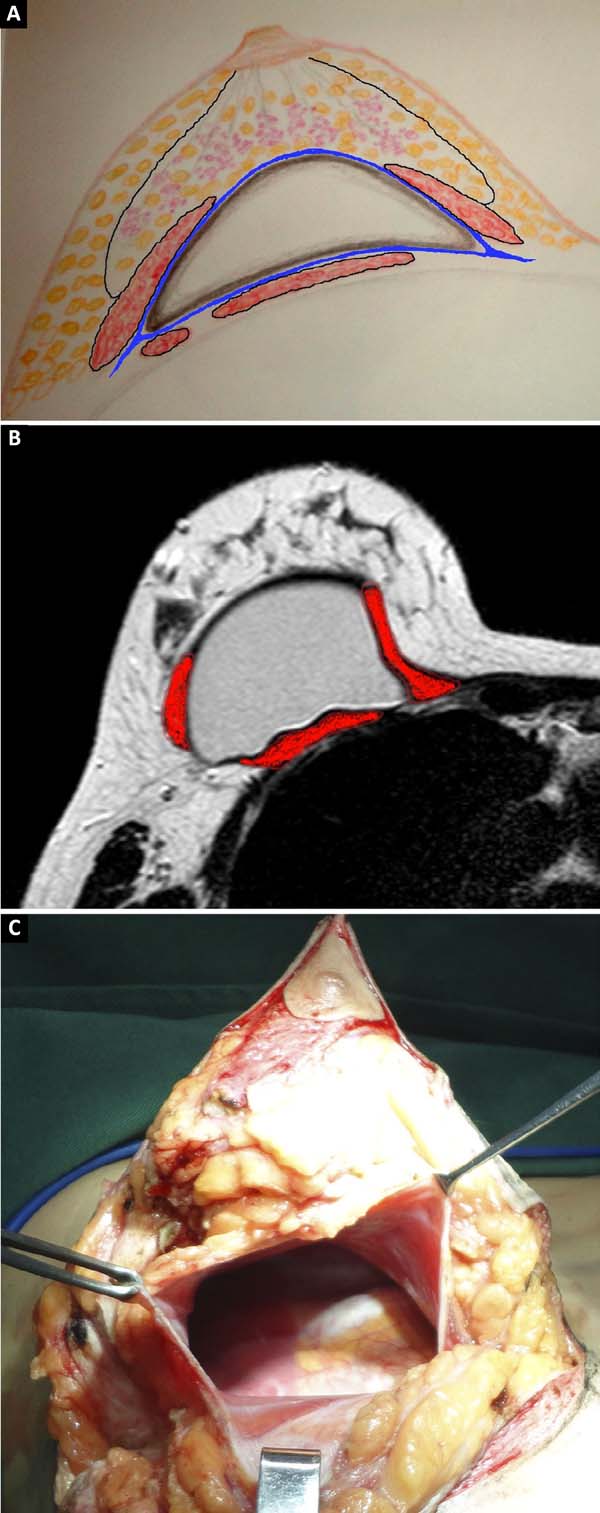
To avoid the possibility of cranial migration of the implant, a suture was performed with 2.0 polyglycolic acid sutures, encompassing the recently divulged edges of the pectoralis major and minor muscle, near the axilla, creating a barrier against the rise of the implant (Figure 4).
After rigorous hemostasis and placement, the implant was partially covered by the loops of the pectoralis major muscle (forming a superomedial pocket and another inferolateral pocket), another suture with polyglycolic acid 2.0 was performed to prevent the muscle from sliding to the sides of the implant, and uncovering the implant, but avoiding closure of the pocket of the pectoralis major.
In mastopexies, before the assembly of the breasts, the need for a breast tissue flap is evaluated, which may vary between a superior pedicle flap15, inferior flap16, bipediculated flap, or without flap with advancement of the lateral pillars of the breast over the muscle. In order to reduce skin tension, the breast is assembled with 3.0 polyglycolic acid threads anchored in the mammary capsule, based on the ligament mammoplasty technique17.
When necessary, the excess skin was resected corresponding to the prior marks, and the NAC was repositioned. A suture with colorless mononylon 4.0 was performed in the subdermal plane and with poliglecaprone 4.0 in the intradermal plane.
Postoperative care
The patients were discharged with a nonsteroidal anti-inflammatory drug (Ketoprofen) and cephalosporin (Cefadroxil) for 8 days. The sutures were covered by tape (Micropore®, 3M) after surgery, which was exchanged every 7 days during the first month. Surgical brassieres were used for 45 days, and a compressive band was positioned in the upper pole of the breast for 20 days which included rest, and prevented the abduction of limbs and sports activities for 60 days.
RESULTS
Between November 2009 and April 2012, a total of 80 patients were operated, with ages ranging from 17 to 54 years (mean = 33 years).
The volume of the implants (Silimed®, Eurosilicone®, Perthese® and SCI® brands, with textured surface and a high or super high round format) ranged between 220 and 380 cc (mean = 260 cc).
A secondary mammoplasty with change of the implant plane was performed in 15 cases (18%). Surgery associated with mammoplasty was performed in in 38 cases (25%). There were 16 cases (20%) of liposculpture and 22 cases (27%) of lipoabdominoplasty.
There were no intraoperative complications. The hospitalization time was up to 30 hours.
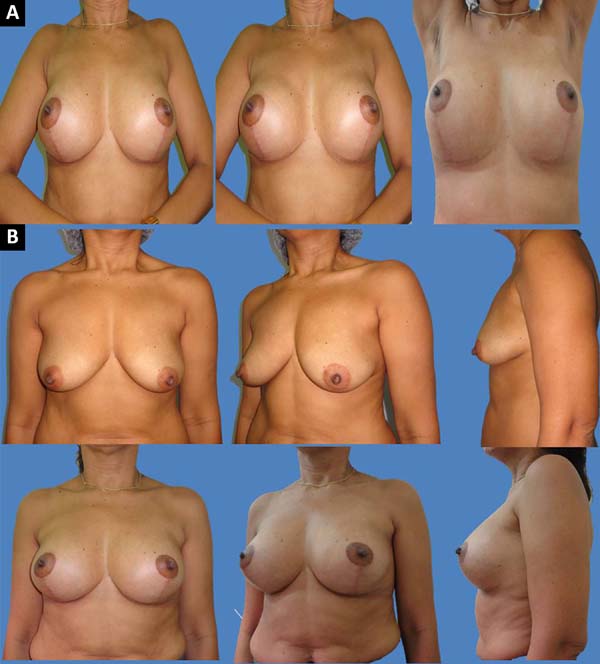
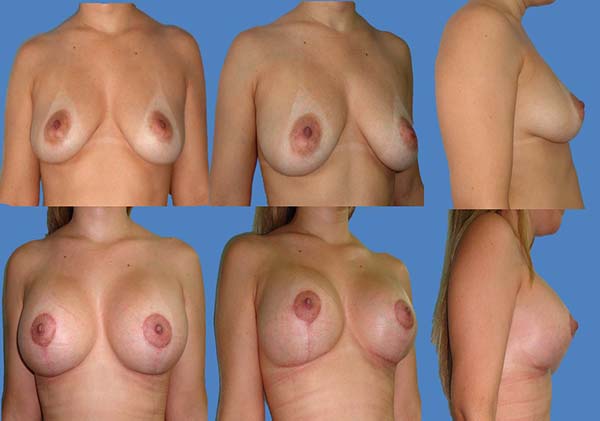
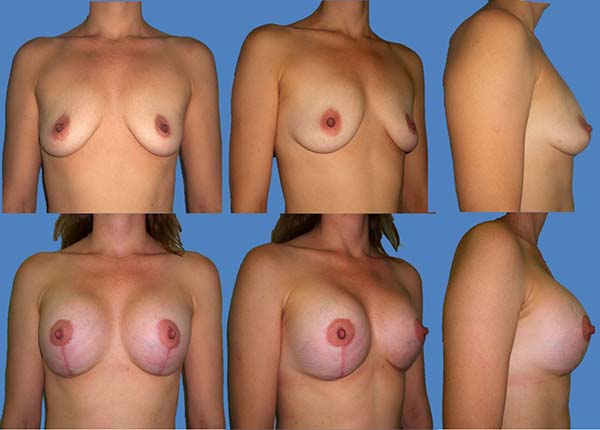
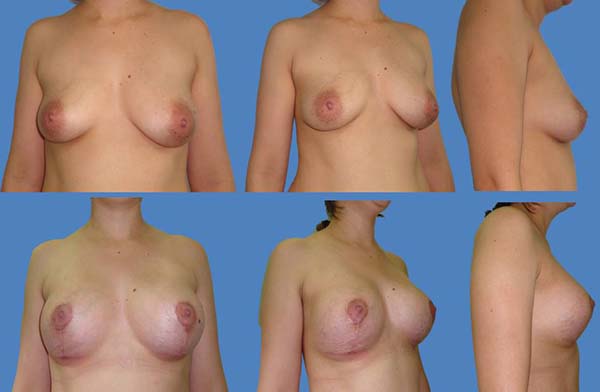
The scars ranged from periareolar, periareolar and vertical, and vertical periareolar and fold locations depending on the degree of sagging, ptosis and size of the implant (Figures 5-9).
An ecchymosis developed on the unilateral side in 1 case (1.25%), with a hematoma observed for more than 3 days. As it was small in volume on USG and without any growth, it was treated without surgery.
No patient presented with infection or implant extrusion.
Capsular contracture was seen in 1 case (1.25%), with good response to zafirlukast, USG, and manual lymphatic drainage18,19.
A late unilateral seroma, observed in 1 case after 60 days (1.25%), was confirmed by USG and re-operated after 6 months, as it evolved with pseudoptosis and asymmetry.
A superficial epitheliolysis of the skin at the junction of the vertical and horizontal scar occurred in 2 cases (2.5%), which were treated with daily dressings until healing.
A scar refinement was performed in 2 cases (2.5%): 1 case of an enlarged scar and 1 case of a hypertrophic scar.
In 3 cases (3.75%) a skin ellipse was withdrawn from the breast sulcus after 6 months, due to horizontal flaccidity. These patients had thin skin and stretch marks.
Mobilization of the implant by contraction of the pectoral muscle was spontaneously reported by 4 patients (5%), with no interference in their daily activities, without requiring intervention (Figures 10A-B).
There was no complaint of paresthesia in the breast or NAC after 3 months.
The follow-up duration ranged from 3 months to 24 months.
DISCUSSION
Several techniques have been described in the literature regarding the positioning of an implant. It may be placed in the subglandular position but to provide greater coverage of the implant with better results, a subfascial placement has been described. However, when positioning the implant in a vertical position, an alteration in its format20 is observed which can cause the rippling seen on the breast surface in cases of flaccid breasts or less breast tissue, thus justifying the need for greater coverage and support of the implant (Figure 11).
The objective of this paper is not to compare the present technique with other traditional ones. However, traditional submuscular techniques involve disinsertion of the pectoralis from the ribcage which leaves the implant covered by muscle only in its upper part, which may cause the implant to slip and make the implant palpable in the inframammary fold7.
In the “envelope flap” technique21, the author shows that, in order to position the implant in a submuscular position, besides the disinsertion, it is necessary to weaken the pectoralis major to avoid limiting the movement of the implant during contraction of the pectoralis major.
In techniques in which the implant is completely covered by muscle, muscle contraction causes a flattening with reduction of breast projection with a possible displacement of the implant towards the axillary region 22,23.
In double space techniques, where the implant is partially submuscular24-28, a muscular contraction can cause compression of the implant, change its shape and position, and project the breast in the medial lap in the lateral muscle pocket technique; while lateralization of the NAC or depression of the medial lap with lateralization of the implant may occur in the upper muscular pocket technique.
However, in the technique presented here, the muscle loops cover the implant in regions of greater fragility after breast augmentation surgery: inferolateral and superomedial quadrants.
In the superomedial quadrant, the muscle flap covers a good portion of the implant, and provides a more natural contour in the lap of the breast (tear- drop), which avoids visualization of the contour of the implant and rippling, and prevents symmastia by medially limiting the pocket.
In the inferolateral quadrant, given a good coverage of the implant, the muscle flap restricts the pocket laterally, preventing the implant from sliding towards the thorax, in addition to providing an inferior support to the implant.
Due to the lack of muscle disinsertion and reduction of the fold in the described technique, the implant is supported by the muscular fibers, preventing its downward slip, with a double inframammary fold. Compression by the fibers of the lateral muscular flap keeps the medial neck of the breast fuller and avoids rippling.
In this technique, the area where the implant is not covered by muscle coincides with the region where the breast parenchyma is thicker, the retroareolar region. By lateralizing the muscle fibers and bypassing the force vector of the muscle by contracting the pectoralis major, the implant is projected forwards rather than upwards.
This allows for a higher cone-shaped breast, and avoids the rise of the implant. Despite the fixation of the pectoralis major to the pectoralis minor muscle superiorly and the approximation of the loops anteriorly to the implant, a slip of the fibers or rupture of the fibers can occur, causing an asymmetry in the positioning of the implant.
In cases where the breasts have little flaccidity with ptosis, and an inframammary fold detachment can be constructed to fit the NAC, the breast has low implantation, and one can palpate the implant in the fold and have a double fold; for this reason, we did not lower the fold.
A muscle surrounding the implant can prevent the formation of seromas, infections and capsular contractures, by promoting increased local blood circulation, facilitating the absorption of liquids and massaging the scar capsule during muscular contraction.
CONCLUSION
The technique described in this paper presented a low index of scar enlargement or dehiscence, which can be attributed to the support of the implant by the muscle and the placement of breasts in deep planes using the mammary capsule as support, without skin tension.
By respecting the anatomy of the pectoralis muscle, this technique was shown to be safe in preserving the insertion, innervation, and irrigation of the pectoral muscles29, allowing the maintenance of muscle function and the smaller detachment of the breast which allowed a lesser extent of injury to the nourishing vessels of the breast.
Therefore, the submuscular double pocket technique provided an adequate coverage and good support of the implant, retained the positioning of the inframammary fold, avoided a deformity of the breast upon contraction of the pectoralis, obtaining good results, with a low index of reinterventions for different types of breasts.
Another study with a larger number of cases with a longer follow-up is currently being carried out to confirm the preliminary results reported here.
REFERENCES
1. Gonzales-Ulloa M. Correction of hypotrophy of the breast by means of exogenous material. Plast Reconstr Surg Transplant Bull. 1960;25(1):15-40. DOI: https://doi.org/10.1097/00006534-196001000-00002
2. Goulian D Jr, Conway H. Correction of the moderately ptotic breast. Plast Reconstr Surg. 1969;43(5):478-80. PMID: 5781824 DOI: https://doi.org/10.1097/00006534-196905000-00004
3. Dempsey WC, Latham WD. Subpectoral implants in augmentation mammaplasty. Preliminary report. Plast Reconstr Surg. 1968;42(6):515-21. PMID: 5722153 DOI: https://doi.org/10.1097/00006534-196812000-00001
4. Spear SL, Pelletiere CV, Menon N. One-stage augmentation combined with mastopexy: aesthetic results and patient satisfaction. Aesthetic Plast Surg. 2004;28(5):259-67. DOI: https://doi.org/10.1007/s00266-004-0032-6
5. Saldanha OR, Maloof RG, Dutra RT, Luz OAL, Saldanha Filho O, Saldanha CB. Mamaplastia redutora com implante de silicone. Rev Bras Cir Plást. 2010;25(2):317-24.
6. de Benito J, Sanches K. Secondary breast augmentation: managing each case. Aesthetic Plast Surg. 2010;34(6):691-700. DOI: https://doi.org/10.1007/s00266-010-9510-1
7. Bozola AR, Bozola AC, Carrazzoni RM. Inclusão de Próteses Mamárias de Silicone - Poliuretano. Rev Soc Bras Cir Plást. 2006;21(1):18-22.
8. Pitanguy I, Amorim NFG, Ferreira AV, Berger R. Análise das trocas de implantes mamários nos últimos cinco anos na Clínica Ivo Pitanguy. Rev Bras Cir Plást. 2010;25(4):668-74. DOI: https://doi.org/10.1590/S1983-51752010000400019
9. Becker H, Springer R. Prevention of capsular contracture. Plast Reconstr Surg. 1999;103(6):1766-8. DOI: https://doi.org/10.1097/00006534-199905000-00036
10. Bastos EM, Neto MS, Alves MT, Garcia EB, Santos RA, Heink T, et al. Histologic analysis of zafirlukast’s effect on capsule formation around silicone implants. Aesthetic Plast Surg. 2007;31(5):559-65. PMID: 17576504
11. Camirand A, Doucet J, Harris J. Breast augmentation: compression--a very important factor in preventing capsular contracture. Plast Reconstr Surg. 1999;104(2):529-38. DOI: https://doi.org/10.1097/00006534-199908000-00038
12. Maia CKF, Freitas GM, Monteiro SS. Anatomia da mama. In: Ribeiro RC, Saltz R, eds. Cirurgia da mama estética e reconstrutiva. Rio de Janeiro: Revinter; 2001.
13. Sampaio MM, Fraga M, Ferreira AP, Barros AC. Structured mammaplasty: a new approach for obtaining breast symmetry. Plast Reconstr Surg. 2013;131(2):300e-302e. PMID: 23358041 DOI: http://dx.doi.org/10.1097/PRS.0b013e318278d7d9
14. França ALF, Scevola MCO, Fachin SD, França PF, França NC. Mamasize: Um Novo Instrumento Auxiliar no Planejamento das Mamoplastias. Rev Soc Bras Cir Plást. 2005;20(4):204-6.
15. Gomes SR. Mastopexia com retalho de pedículo superior e implante de silicone. Rev Bras Cir Plást. 2008;23(4):241-7.
16. Mansur JRB, Bozola AR. Mastopexia e aumento das mamas com proteção e suporte inferior da prótese com retalho de pedículo inferior. Rev Bras Cir Plást. 2009;24(3):304-9.
17. Bono JEP. Mamoplastia Ligamentar. Rev Bras Cir Plást. 2008;23(3):192-9.
18. Rosique MJF, Rosique RG, Flores LRP, Amaral AB, Mélega JM. Uso de zafirlucaste para o tratamento de contratura capsular: estudo preliminar. Rev Bras Cir Plást. 2008;23(2):120-3.
19. Santos MAG, Boggio RF, Carlucci AR, Motoka E, Albano AM. Prevenção e tratamento da contratura capsular após implantação de prótese mamária. Rev Bras Cir Plást. 2010;25(2):304-8.
20. Migliori F. “Upside-down” augmentation mastopexy. Aesthetic Plast Surg. 2011;35(4):593-600. DOI: https://doi.org/10.1007/s00266-010-9623-6
21. Leão CEG. Mamaplastia de aumento: técnica em “aba de envelope”. Rev Bras Cir Plást. 2009;24(2):202-7.
22. Spear SL, Schwartz J, Dayan JH, Clemens MW. Outcome assessment of breast distortion following submuscular breast augmentation. Aesthetic Plast Surg. 2009;33(1):44-8. PMID: 19052809 DOI: https://doi.org/10.1007/s00266-008-9275-y
23. Pelle-Ceravolo M, Del Vescovo A, Bertozzi E, Molinari P. A technique to decrease breast shape deformity during muscle contraction in submuscular augmentation mammaplasty. Aesthetic Plast Surg. 2004;28(5):288-94. DOI: https://doi.org/10.1007/s00266-003-3023-0
24. Khan UD. Dynamic breasts: a common complication following partial submuscular augmentation and its correction using the muscle-splitting biplane technique. Aesthetic Plast Surg. 2009;33(3):353-60. PMID: 19280247 DOI: https://doi.org/10.1007/s00266-009-9320-5
25. Panettiere P, Marchetti L, Accorsi D, Del Gaudio GA. Augmentation mammaplasty of teardrop-shaped breasts using round prostheses. Aesthetic Plast Surg. 2003;27(1):20-6. DOI: https://doi.org/10.1007/s00266-002-0061-y
26. Khan UD. Muscle-splitting breast augmentation: a new pocket in a different plane. Aesthetic Plast Surg. 2007;31(5):553-8. DOI: https://doi.org/10.1007/s00266-006-0242-1
27. Daniel MJB. Inclusão de Prótese de Mama em Duplo Espaço - Prêmio Georges Arié 2004. Rev Bras Cir Plást. 2005;20(2):82-7.
28. Soares AB, Franco FF, Rosim ET, Renó BA, Hachmann JOPA, Guidi MC, et al. Mastopexia com uso de implantes associados a retalho de músculo peitoral maior: técnica utilizada na Disciplina de Cirurgia Plástica da Unicamp. Rev Bras Cir Plást. 2011;26(4):659-63. DOI: https://doi.org/10.1590/S1983-51752011000400021
29. Park HD, Min YS, Kwak HH, Youn KH, Lee EW, Kim HJ. Anatomical study concerning the origin and course of the pectoral branch of the thoracoacromial trunk for the pectoralis major flap. Surg Radiol Anat. 2004;26(6):428-32. DOI: https://doi.org/10.1007/s00276-004-0273-8
1. Clínica Debs, Porto Velho, RO,
Brazil.
2. Clínica Debs, Patrocínio, MG,
Brazil.
3. Clínica Rosique, Ribeirão Preto, SP,
Brazil.
Autor correspondente: Leandro Debs Procópio, Av. Carlos Gomes, nº 2119 - São Cristóvão, Porto Velho, RO, Brazil, Zip Code 76804-037. E-mail: doutorleandro@bol.com.br
Article received: July 25, 2018.
Article accepted: April 21, 2019.
Conflicts of interest: none.















 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter