

Case Report - Year 2019 - Volume 34 -
Retroauricular island flap for partial ear reconstruction: case reports
Retalho retroauricular ilhado para reconstrução parcial de orelha: relato de casos
ABSTRACT
Partial ear defects can be treated in several ways, including primary closure, healing by secondary intention, or flaps. Several surgical options have been described for reconstruction in order to maintain the natural contour of the ear, without sacrificing healthy tissues or changing the aesthetics and function. In this article, we present two cases of reconstruction of chondrocutaneous defects of the ear after resection of basal cell carcinoma in the central region of the ear, with the production of a retroauricular island flap transposed through a cartilaginous window with the de-epidermized pedicle. The donor area healed following a primary closure. This procedure can be performed in a single stage, yields satisfactory aesthetic and functional results, and is safe because the retroauricular region is richly vascularized.
Keywords: Reconstructive surgical procedures; Acquired deformities of the ear; Surgical flaps; Neoplasms of the ear; External ear
RESUMO
Defeitos parciais de orelha podem ser tratados de diversas formas, dentre elas o fechamento primário, cicatrização por segunda intenção ou retalhos. Diversas opções técnicas foram descritas para a sua reconstrução de modo a manter o contorno natural da orelha, sem sacrificar tecido sadio ou alterar sua estética e função. Apresentamos neste artigo dois casos atendidos no Instituto do Câncer do Hospital de Base de São José do Rio Preto de reconstrução de defeitos condrocutâneos de orelha após ressecção de carcinoma basocelular em região central da orelha, com a confecção de retalho retroauricular ilhado transposto através de uma janela cartilaginosa e com o pedículo desepidermizado. Área doadora com fechamento primário. Tal procedimento constitui técnica segura, pois a região retroauricular é ricamente vascularizada, é de fácil execução, em único estágio e com resultado estético e funcional satisfatório.
Palavras-chave: Procedimentos cirúrgicos reconstrutivos; Deformidades adquiridas da orelha; Retalhos cirúrgicos; Neoplasias da orelha; Orelha externa
INTRODUCTION
Ear neoplasms are relatively common as they are susceptible to sun exposure. Surgery by excision and reconstruction of partial ear defects without changing their natural shape or reducing their size is the best approach for treatment. Alternative techniques involving healing by secondary intention or excisions reduce the size or deform the ear as healthy tissues need to be removed. Skin grafts in ear reconstruction are subject to contraction, loss of natural contour, and aesthetic deformity1.
The retroauricular region has conventionally been used as the skin graft donor site for surgery. However, in 1959, Owens2 introduced the concept of transposing a retroauricular skin flap through an opening in the cartilage to another portion of the ear with a de-epidermized pedicle. This technique minimizes the risks of cartilaginous exposure and chondritis in healing by secondary intention, and has superior aesthetic outcomes in terms of contour, color, shape of the external auricular meatus, and subsequent hearing loss. We present two cases of partial ear reconstruction after resection for skin cancer.
CASE REPORT
Two patients were treated at the Cancer Institute of the Hospital de Base de São José do Rio Preto - São Paulo, in 2017 and 2018 after being diagnosed with basal cell carcinoma by incisional biopsy. The lesions were slow growing, ulcerated, and friable. They were excised under local anesthesia with 2% lidocaine solution and 1:100,000 vasoconstrictors, with the surgical margins including cartilage and posterior perichondrium.
Case 1
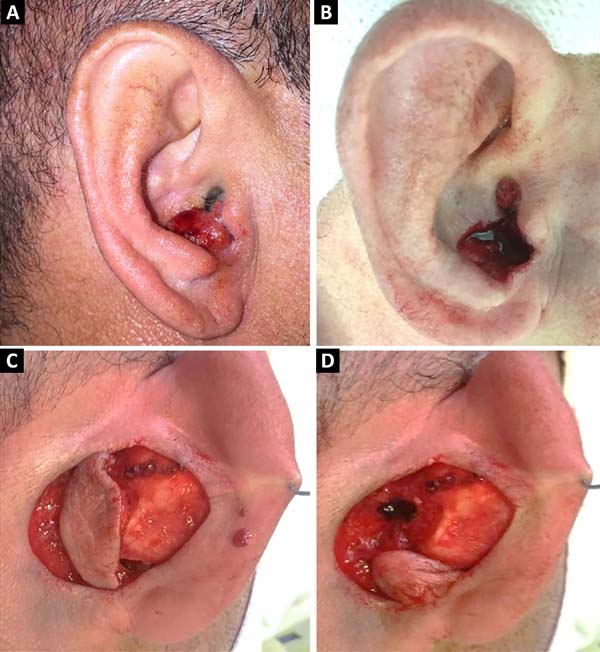
A 40-year-old male patient had a 1.5 cm nodular lesion in the right auricle close to the auditory meatus. After resection of the lesion, a retroauricular flap was made with an axial lower pedicle based on the lower branch of the posterior auricular artery. After transposition through the cartilaginous defect, the skin island was left in a shape and extension similar to the resected skin defect, and an area of 1 x 1 cm2 corresponding to the arterial pedicle was de-epidermized and primary closure of the donor area was performed (Figures 1 and 2). The patient did not develop any post-surgical necrosis, flap congestion, wound dehiscence, hematoma. or infection (Figure 3). The pathological report revealed that it was an infiltrative and expansive basal cell carcinoma without epidural or vascular invasion with tumor-free surgical margins.
Case 2
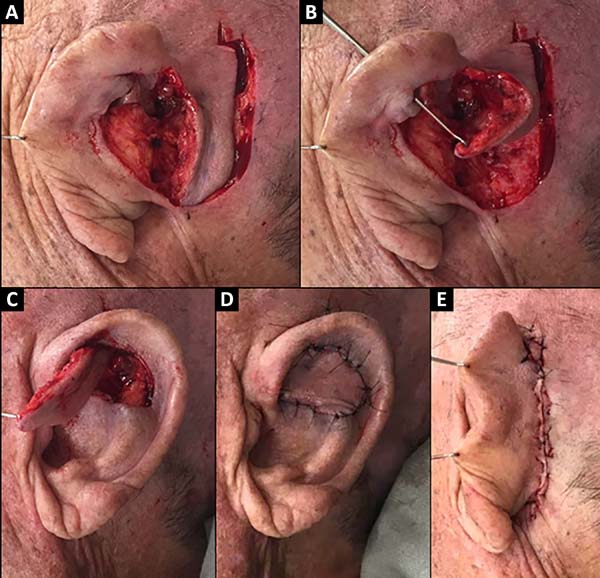
A 74-year-old male patient presented with a 2.5 cm lesion in the conchal and left antihelix region. Resection of the lesion including cartilage and perichondrium was performed, resulting in a defect of 3.5 x 3 cm size (Figure 4). A retroauricular flap was made with an axial superior pedicle based on the superior auricular artery, a branch of the superficial temporal artery. The flap was transposed through the cartilaginous window, with a small portion of the pedicle de-epidermized and the flap accommodated to the bed similar in shape and extension. Primary closure of the donor area was performed (Figure 5). The results were satisfactory, without signs of inflammation or other complications with good aesthetic results (Figure 6).
DISCUSSION
Several authors have described the use of the retroauricular flap and have adapted the technique to add their own modifications. In 1972, Masson3 described the technique of reconstruction of auricle based on a retroauricular flap, without a de-epidermized pedicle. Renard4 performed a superior de-epidermized pedicle retroauricular flap reconstruction for defects in the auricle, and for more extensive ones involving the antihelix. Wood-Smith et al.5 reported the treatment of extensive lesions in the auricle using two retroauricular flaps, one from the posterior surface of the ear and the other from the superior pedicle. Yoav et al. 6, in turn, used a myocutaneous flap based on the posterior auricular muscle.
Several studies have analyzed the surgical treatment of ear lesions. Some authors advocate a skin graft as the first option, while others advocate second-intention healing for small auricular lesions, and still others advocate primary closure, depending on the location and size of the lesion7-9.
However, larger defects are associated with aesthetic and functional complications. Adequate excision of tumors from this region requires resection of cartilage for a safe tumor margin. A retroauricular flap has many advantages as it is a single-stage surgical procedure that can be performed under local anesthesia in an outpatient setting. When used for reconstruction of the auricle and other defects of the anterior face of the ear, the results are similar in terms of color and texture, with satisfactory aesthetic appearance6. It has low complications at the donor site, with scar behind the ear and being in most cases of primary closure. This flap has is safe due to its vascular supply, and is well documented in studies by Park et al. 10, among others11.
Therefore, it is a safe option for reconstruction of ear defects of the entire anterior surface and can be used even in large lesions.
CONCLUSION
The authors recommend that retroauricular flaps can be used in several ways, including treatment of ear defects. It is well vascularized, which makes it safe to harvest, it can be performed in a single stage, and it is useful for small and large lesions without causing serious complications or sacrificing healthy tissue. It has excellent aesthetic and functional results.
COLLABORATIONS
|
VBC |
Analysis and/or data interpretation, realization of operations and/or trials. |
|
MVC |
Analysis and/or data interpretation, realization of operations and/or trials. |
|
CCF |
Analysis and/or data interpretation, realization of operations and/or trials. |
|
GVS |
Analysis and/or data interpretation, realization of operations and/or trials. |
|
CGS |
Analysis and/or data interpretation, writing - review & editing. |
|
JGCK |
Realization of operations and/or trials. |
|
LAFK |
Analysis and/or data interpretation, realization of operations and/or trials, writing - original draft preparation. |
|
ARB |
Analysis and/or data interpretation, final manuscript approval. |
REFERENCES
1. Azaria R, Amir A, Hauben DJ. Anterior conchal reconstruction using a posteroauricular pull-through transpositional flap. Plast Reconstr Surg. 2004;113(7):2071-5. PMID: 15253199 DOI: https://doi.org/10.1097/01.PRS.0000121186.46720.B0
2. Owens N. An effective method for closing the external auditory canal. Plast Reconstr Surg Transplant Bull. 1959;23(4):381-7. PMID: 13645254
3. Masson JK. A simple island flap for reconstruction of concha-helix defects. Br J Plast Surg. 1972;25(4):399-403. PMID: 4567027 DOI: https://doi.org/10.1016/S0007-1226(72)80083-3
4. Renard A. Postauricular flap based on a dermal pedicle for ear reconstruction. Plast Reconstr Surg. 1981;68(2):159-64. DOI: https://doi.org/10.1097/00006534-198108000-00005
5. Wood-Smith D, Ascherman JA, Albom MJ. Reconstruction of acquired ear defects with transauricular flaps. Plast Reconst Surg. 1995;95(1):173-5. DOI: https://doi.org/10.1097/00006534-199501000-00031
6. Yoav PT, Horowitz Z, Bedrin L, Kronenberg J. Auricular reconstruction with a postauricular myocutaneous island flap: Flip-Flop Flap. Plast Reconstr Surg. 1996;98(7):1191-9. DOI: https://doi.org/10.1097/00006534-199612000-00010
7. Peled IJ. Healing of ear defects: primary or secondary. Plast Reconst Surg. 1997;100(1):277-8.
8. Ghassemi A, Modabber A, Talebzadeh M, Nanhekhan L, Heinz M, Hölzle F. Surgical management of auricular defect depending on the size, location, and tissue involved. J Oral Maxillofac Surg. 2013;71(8):e232-42.
9. Watson D, Hecht A. Repair of Auricular Defects. Facial Plast Surg Clin North Am. 2017;25(3):393-408.
10. Park C, Shin KS, Kang HS, Lee YH, Lew JD. A new arterial flap from the postauricular surface: its anatomic basis and clinical application. Plast Reconstr Surg. 1988;82(3):498-505. PMID: 3406183
11. Song R, Song Y, Qi K, Jiang H, Pan F. The superior auricular artery and retroauricular arterial island flaps. Plast Reconst Surg. 1996;98(4):657-67.
1. Faculdade de Medicina de São José do Rio
Preto, São José do Rio Preto, SP, Brazil.
Corresponding author: Lauro Arnoldo Ferreira Koehler, Rua Curitiba, nº 202, Bairro Olarias, Ponta Grossa, Paraná, Brazil. Zip Code: 84.035-030. E-mail: lauro_afk@hotmail.com
Article received: June 17, 2018.
Article accepted: February 10, 2019.
Conflicts of interest: none.












 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter