

Articles - Year 2002 - Volume 17 -
Myectomy of the Orbicularis Oculi Muscle: A New Procedure Associated to Bleroplasty
Miectomia do Músculo Orbicular dos Olhos: Procedimento Associado à Bleroplastia
ABSTRACT
The authors deseribe myectomy at the lateral border of the orbieularis oculi muscle during blepharoplasty to attenuate periorbital wrinkles ("crow's feet"). There were no surgieal, aesthetic or functional complications with this procedure. All patients that underwent surgery presented wrinkle attenuation. Most evident results could be seen in those patients with a lesser degree of cutaneous photoaging. The authors conclude that this is a safe, fast, and easy procedure, which presents good aesthetic and functional results.
Keywords: Regional anatomy; blepharoplasty; mimetic muscles; facial nerve; rejuvenation
RESUMO
Os autores descrevem a realização de uma miectomia na margem lateral do músculo orbicular dos olhos durante a blefaroplastia visando a atenuação das rugas periorbitais ("pés-de-galinha"). Não houve complicações cirúrgicas, estéticas ou funcionais com este procedimento. Todas as pacientes operadas apresentaram atenuação das rugas, sendo o resultado mais evidente naquelas com menor grau de fotoenvelhecimento cutâneo.
Os autores concluem que este é um procedimento seguro, rápido e de fácil execução, apresentando bons resultados estéticos e funcionais.
Palavras-chave: Anatomia regional; blefaroplastia; músculos miméticos; nervo facial; rejuvenescimento
A limiting factor for blepharoplasty is the remaining periorbital wrinkles ("crow's feet") that persist even after face lifting. Procedures such as chemical and laser peelings or micro-abrasion are extremely valuable as a complementary treatment for facial rejuvenation surgeries. However, they work on static wrinkles, and interfere little on dynamic wrinkles, caused by the contraction of the facial mimic musculature present under face skin. Type-A botulinus toxin may be an alternative in these cases (1), leading to the temporary paralysis of the muscle to which it is applied and, therefore, attenuating such wrinkles.
In order to perform a longer-lasting treatment for dynamic wrinkles, we propose a standardized myectomy of the orbicularis oculi muscle during blepharoplasty, leading to partial and located rupture of the muscular sphincter in its lateral portion at the external corner of the palpebral rim, to minimize wrinkles at this site.
ANATOMY
ORBICULARIS OCULI MUSCLE
The orbicularis oculi muscle is an elliptic, thin and plain sphincter that involves the orbital opening and consists of 2 portions: orbital and palpebral(2,3).
Strong eyelid closing is performed with the help of the orbital portion, moving the skin of the forehead, temple and cheek towards the medium eyelid angle. This results in radiated skin folds in the lateral eyelid angle, which become permanent in elderly people or in those with an advanced degree of photoaging ("crow's feet").
MOTOR INNERVATION OF THE ORBICULARIS OCULI MUSCLE
In general, we observe 3 to 4 temporal branches of the facial nerve, in that the two latter communicate with each other and innervate the superior portion of the orbicularis oculi muscle. They enter the muscle laterally through its deepest side, penetrating it approximately 3 to 4 mm medially to its free border(4).
Zygomatic branches are usually found in pairs, crossing the external border of the zygomaticus major muscle in its superior third to reach the lower portion of the orbicularis oculi muscle taking motor innervation to it (3,4,5).
SURGICAL TECHNIQUE
Blepharoplasty is marked as usual, according to established technical principies. We identity the orbital edge at the level of the lateral palpebral commissure for the superior eyelid incision. We draw a lateral lyoriented horizontal line of approximately 15 to 20 mm starting from this point, which will correspond to the height of the muscle trapezium to be resected during myectomy. The lateral and distal base of this trapezium must be approximately 7 to 10 mm; its apex, situated on the orbital edge, must be approximately 5 mm (Fig. 1).
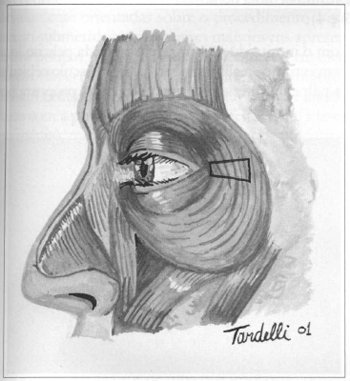
Fig. 1 - Drawing of muscular resection during myectomy.
With the help of Gilles skin hooks and a pair of delicate iris scissors, we detach and dissect the supradjacent skin and the deeper insertions of this imaginary muscular trapezium, releasing ir for resection (Fig. 2).
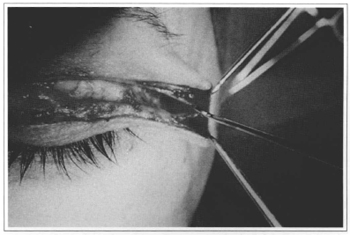
Fig. 2 - Muscle detachment.
With the pair of iris scissors, we cut the muscular trapezium and conduct hemostasis with the electrocautery (Figs. 3 and 4).
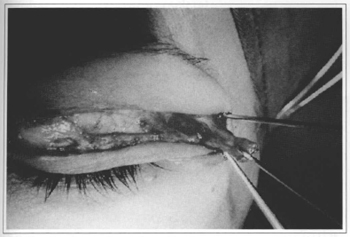
Fig.3 - Myectomy.
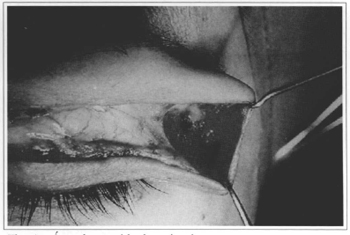
Fig. 4 - Area lacking muscle.
In order to prevent skin depression at the myectomy, we make a flap in the orbicular muscle of the lower eyelid, following the technique proposed by Hamra(6) for filling the site. We also improve the medium third of the face through the traction of the fat of the malar regionv(6,7,8) with the flap, which is attached to the orbital rim with colorless Monocryl 4-0.
The skin is closed with 2 to 3 simple Nylon 6-0 sutures in the incision's lateral portion, along with an intradermal suture with the same Nylon 6-0.
We use Micropore® tape dressing for smooth compression and a lateral cranial traction on the infra-orbital region skin.
RESULTS
We selected 6 female patients, duly informed about the procedure they would be submitted to. The youngest patients presented little signs of photoaging skin, but several periorbital wrinkles. Among those, many had already used botulinus toxin, and were dissatisfied with its brief effect (4 to 6 months on average).
After a postoperative follow-up that varied from 3 to 10 months, all patients stated they were pleased with the results obtained. All cases we operated presented some degree of improvement in periorbital wrinkles. Most dramatic results were observed on those individuals with a minimum quantity of static wrinkles and a clear presence of dynamic wrinkles (Figs. 5-8).
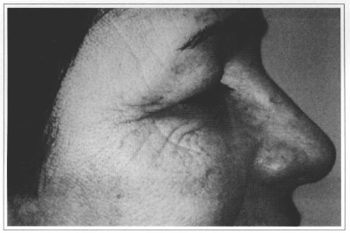
Fig. 5 - Dynamic preoperative period.
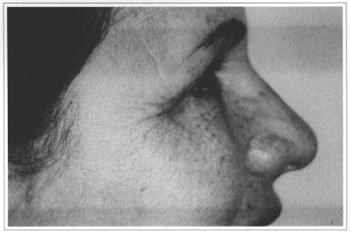
Fig. 6 - Dynamic postoperative period.
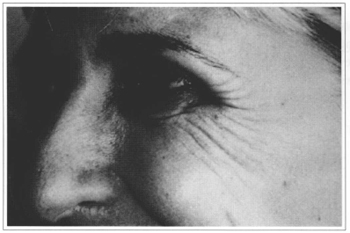
Fig. 7 - Dynamic preoperative period.
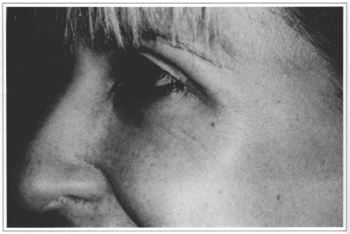
Fig. 8 - Dynamic posroperative period.
Postoperative edema and ecchymosis were minimal and similar to those in conventional blepharoplasty. None of the patients presented ectropium, lagophthalmus or scleral exposure. There were no cases with signs of skin suffering or suture dehiscence.
DISCUSSION
Using type A botulinus toxin to attenuate periorbital wrinkles is a well-established and a proven effective procedure, although ephemeral (1). The paralysis of the orbicular muscle in its portion lateral to the orbital rim, after injecting botulinus toxin in specific points and in a correct dosage, promotes noticeable attenuation of periorbital wrinkles without affecting eyelid closing.
Mühlbauer(9), in an article published in 1995, described myectomies, myotomies and neurotomies to correct facial expression wrinkles associated to aesthetic procedures, referring to them as Mimetic Modulation, although he did not describe how they were performed in detail.
These data have encouraged us to apply some of the procedures used for correcting blepharoespasm(10,11,12) to palpebrate aesthetic surgery, by changing some of the existing techniques, moderately resecting the orbicular muscle on the external lateral portion of the palpebral commissure, attenuating its contraction, and thus diminishing skin wrinkles at this site ("crow's feet"). Even if some terminal motor nerve fibers are damaged during myectomy, there will not be any major problems to eyelid contraction, and may even result in better and long-lasting results (9,10,11,12).
We believe that making an orbicular muscle flap as per the Hamra(6,7) technique directs a volume of noninnerved muscular tissue to the myectomy area, preventing depression in the area and that the free borders of the orbicular muscle unite again to form the palpebral sphincter. Moreover, it provides an increase of tension over the lower eyelid tarsus, preventing lagophthalmos by transitory paresis of the orbicularis oculi muscle in the postoperative period.
CONCLUSION
Based on our personal experience and relevant literature, we concluded that marginal myectomy of the orbicularis oculi muscle associated to aesthetic blepharoplasty proves to be an easy and fast procedure, with minimum risk of resulting injuries or functional damage to the musculature and to palpebrate and orbital skin. It also presents highly satisfactory aesthetic and functional results.
REFERENCES
1. Borodic GE, Cozzolino D. Blepharospasm and its treatment, with emphasis on the use of botulinum toxin. Plast Reconstr Surg. 1989; 83:546-554.
2. Gardner E, Gray DJ, O'Rahilly R. Anatomia: estudo regional do corpo humano. 4. ed. Rio de Janeiro: Guanabara Koogan; 1982. p. 618-49.
3. Zide BM, Jelks GW. Surgical Anatomy of the Orbit. 1. ed. New York: Raven Press; 1985. p.12-50.
4. Freilinger G, Gruber H, Happak W,Pechmann U. Surgical anatomy of the mimic muscle system and the facial nerve: Importance for reconstructive and aesthetic surgery Plast Reconstr Surg. 1987; 80: 686-90.
5. Lineaweaver W, Rhoton A, Habal MB.Microsurgical anatomy of the facial nerve. J Craniofac Surg. 1997; 8: 6-10.
6. Hamra ST. Repositioning the orbicularis oculi muscle in the composite rhyridectorny Plast Reconstr Surg. 1992; 90: 14-22.
7. Hamra ST. The Zygorbicular Dissection in Composite Rhytidectomy: An ideal midface plane.Plast Reconstr Surg. 1998; 102: 1646-57.
8. Lassus C. Benefits from Lifting of the Lower Eyelid. Aesth Plast Surg. 2000; 24: 424-428.
9. Mühlbauer W, Fairley J, Wingerden JV. Mimetic modulation for problem creases of the face. Aesth Plast Surg. 1995; 19: 183-191.
10. Callahan A. Blepharaspasm with resection of part of orbicularis nerve suply: correction of intractable cases. Arch Ophtalmol. 1963; 70: 508-511.
11. Castañares S. Blefaraespasmo. In: Coiffman F, editor. Cirugía Plástica, Reconstructiva Y Estética. 2. ed. Barcelona: Masson; 1994 p. 2499-503.
12. Jones TW Jr, Waller RR, Samples JR. Myectomy for essential blepharospasm. Mayo Clin Prac. 1985; 60: 663-8.
I - Senior Member of the Brazilian Society of Plastic Surgery and Assistant Physician of Santa Cruz Plastic Surgery Institute.
II - Senior Member of the Brazilian Society of Plastic Surgery
III - Senior Member of the Brazilian Society of Plastic Surgery and Director of Santa Cruz Plastic Surgery Institute.
Address for correspondence:
Antenor Bonatto Júnior, MD
R. Santa Cruz, 398
04122-000 - São Paulo - SP Brazil
Phone: (55 11) 5575-9863
e-mail: abonatto@terra.com.br
Worked performed at Santa Cruz Plastic Surgery Institute


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter