

Original Article - Year 2019 - Volume 34 -
Evaluation of Tension Reduction on Abdominoplasty Scar Using Baroudi Adhesion Sutures
Avaliação da redução tensional sobre a cicatriz em abdominoplastia com o uso de pontos de adesão de Baroudi
ABSTRACT
Introduction: In 1988, Baroudi et al. published a paper
describing the use of adhesion points between the dermoadipose
flap and the anterior rectus abdominis sheath to reduce seroma
formation. This study aimed to demonstrate a probable
correlation between the use of Baroudi adhesion points and
reduction in flap tension force by measuring the distance
from the lower abdominal scar to the xiphoid before and
after using Baroudi points in dermolipectomy transoperatory.
Methods: This was a prospective observational study that
selected patients who underwent lipoabdominoplasty at
the Santa Casa de Misericórdia Plastic Surgery Service of
Porto Alegre from January to April 2019. The transoperatory
measurements of distance from the sternal xiphoid appendix
to the umbilical scar and from the pre-xiphoid to the postxiphoid
scar before and after execution of Baroudi's adhesion
points were compared. Statistical analysis was performed
using Excel® software.
Results: A reduction in the distances
between the xiphoid-umbilical scar appendix and xiphoidscar
appendix was verified after execution of Baroudi
suture (mean 1.5 cm), indicating a decrease in scar tension.
Conclusion: There was a decrease in the xiphoid-umbilical
scar and xiphoid-lower abdominal scar distance after Baroudi
stitches, indicating lower scar-tissue tension. Further studies
should be conducted to evaluate these measurements in the
long term and their correlation with a better-quality scar.
Keywords: Dermolipectomy; Baroudi Points; Healing tension; Abdominal scar; Abdomen measurements.
RESUMO
Introdução: Em 1988, Baroudi et al. publicaram um trabalho descrevendo a utilização de pontos de adesão entre o retalho dermoadiposo e a bainha anterior do músculo reto do abdome, no intuito de diminuir a formação de seroma. O presente estudo propõe-se a demonstrar uma provável correlação entre os pontos de adesão de Baroudi com a força tensional do retalho, através da medida da distância da cicatriz abdominal inferior ao xifoide antes e após os pontos de Baroudi, no transoperatório de dermolipectomia.
Métodos: Trata-se de um estudo prospectivo observacional. Foram selecionadas submetidas a lipoabdominoplastia no Serviço de Cirurgia Plástica da Santa Casa de Misericórdia de Porto Alegre, no período de janeiro a abril de 2019. Aferiram-se as medidas transoperatórias da distância do apêndice xifoide esternal à cicatriz umbilical, e da primeira à cicatriz cirúrgica, pré e pós-realização dos pontos de adesão de Baroudi. A análise estatística foi realizada com o software Excel®.
Resultados: Verificou-se a diminuição das distâncias apêndice xifoide-cicatriz umbilical e apêndice xifoide-cicatriz após a realização da sutura de Baroudi (média de 1,5cm), pressupondo-se diminuição da tensão da cicatriz.
Conclusão: As medidas aferidas no presente estudo mostraram uma diminuição da distância xifoide-cicatriz umbilical e xifoide-cicatriz abdominal inferior após a realização dos pontos de Baroudi, evidenciando uma menor tensão na cicatriz. Sugere-se estudos para avaliar como essas medidas se comportam a longo prazo e se realmente se correlacionam a uma cicatriz de melhor qualidade.
Palavras-chave: Dermolipectomia; Pontos de Baroudi; Tensão cicatricial; Cicatriz abdominal; Medidas do abdome
INTRODUCTION
Abdominal dermolipectomy, also known as abdominoplasty, has been performed for decades, and it has gradually evolved to the more elaborate techniques currently in use.
From the surgical point of view, there has been a considerable evolution with respect to scar extension and dermoadipose flap detachment.
In the late 1970s, reduced incision abdominoplasty was introduced, which provided good results in selected cases. However, changes in the supraumbilical region could not be properly corrected with this technique, and this limitation with excess skin was evident when the patient sat, leading to patient and doctor dissatisfaction in most cases.
In the 1980s, the introduction of liposuction associated with abdominal plastic surgery yielded better results. However, there were considerable complication rates, especially with seromas1.
n 1988, Baroudi et al. published a paper describing the use of adhesion points between the dermoadipose flap and the anterior rectus abdominis sheath to reduce dead space and consequent seroma formation, a frequent complication previously observed due to extensive detachment in the classic abdominoplasty2. In 1999, Avelar et al.3 described the technique of mini-tummy tuck without flap detachment in the lower abdominal portion. In 2001, Saldanha4 introduced the lipoabdominoplasty technique with preservation of the perforating vessels, showing a significant reduction in flap necrosis rates and introducing a new direction in abdominal plastic surgery. Lipoabdominoplasty with liposuction reduces supraumbilical dermoadipose flap detachment and preserves blood circulation in the flap3.
Abdominoplasty is based on the variable length of detachment of the fasciocutaneous layer of the abdomen encompassing the xipho-pubic region, flank region, and costal arches, with subsequent resection of the dermoadipose panicle excess and lowering of the flap. The tension generated by the flap approach towards the lower incision seems to be responsible for scar enlargement, tendency of more cranial scar positioning, suture dehiscence, and necrosis of the lower flap portions4.
Since 2005, lipoabdominoplasty has been the preferred technique for treatment of abdominal deformities at the Santa Casa de Misericórdia Plastic Surgery Service of Porto Alegre/Federal University of Health Sciences of Porto Alegre. This consists of performing epigastrium and flank liposuction with reduced dermoadipose flap detachment. During the synthesis, Baroudi adhesion points are made to reducing the dead space and facilitate the flap descent associated with better positioning. The number of points executed does not follow any predetermined rigid standard and are performed as needed5.
Although several studies have been conducted on the use of Baroudi points for seroma reduction, limited data are available on the use of Baroudi adhesion points for scar tension reduction and subsequent improvement in its appearance.
Therefore, the present study proposed to demonstrate a probable correlation between Baroudi adhesion points and flap tension force, verifying the positioning, maintenance, and scar quality after abdominoplasty by using these points6.
OBJECTIVE
The main objective of the present study was to quantify the reduction of scar tension after abdominoplasty using Baroudi adhesion points.
Additionally, the transoperatory measurements of the distance from the sternal xiphoid appendix to the umbilical scar before and after the execution of Baroudi adhesion points was compared to correlate these measurements with the healing quality.
METHODS
Inclusion criteria
Female non-smoking patients aged 18-60 years and with a body mass index (BMI) of <28 kg/m2 who underwent lipoabdominoplasty at the Santa Casa de Misericórdia Plastic Service of Porto Alegre from January to April 2019 were included.
Methods
All included patients underwent standardized pre-, trans-, and postoperative care.
The transoperatory measurements of distance from the sternal xiphoid appendix to the umbilical scar and from the pre-xiphoid to the post-xiphoid scar before and after execution of Baroudi’s adhesion points were measured. The difference between these two measurements was evaluated in the results.
Consecutive prospective statistical analysis of the data was performed using Excel software®.
The present study was not interventional. The surgical procedure for abdominal dermolipectomy was performed in each patient as indicated by the case after the consent form and authorization for surgery were obtained. Lipoabdominoplasty was used as the surgical technique, and the study included patients who met the inclusion criteria. All standards issued by the National Health Agency were strictly followed. Patients and/or guardians received proper guidance on the procedures performed.
The Santa Casa de Misericórdia Plastic Surgery Service of Porto Alegre/Federal University of Health Sciences of Porto Alegre is committed to maintain confidentiality of data contained in the medical records, ensuring that patients are not identified during the course of the research.
RESULTS
Eighteen patients were included in the study, and their transoperatory measurements are listed in Table 1.
| Patient | Pre-Xiphoid Umbilical | Post-Xiphoid Umbilical | Pre-Xiphoid Scar | Post-Xiphoid Scar |
|---|---|---|---|---|
| 1 | 10.0cm | 9.0 cm | 20.0 cm | 19.0 cm |
| 2 | 10.4cm | 8.9 cm | 20.4 cm | 18.9 cm |
| 3 | 11.8 cm | 9.8 cm | 21.8 cm | 19.8 cm |
| 4 | 10.4 cm | 8.4 cm | 20.4 cm | 18.4 cm |
| 5 | 12.2 cm | 10.7 cm | 22.2 cm | 20.7 cm |
| 6 | 10.8 cm | 9.8 cm | 20.8 cm | 19.8 cm |
| 7 | 12.6 cm | 11.6 cm | 22.6 cm | 21.6 cm |
| 8 | 11.2 cm | 9.7 cm | 21.2 cm | 19.7 cm |
| 9 | 13.0 cm | 11.0 cm | 23.0 cm | 21.0 cm |
| 10 | 11.6 cm | 9.6 cm | 21.6 cm | 19.6 cm |
| 11 | 13.2 cm | 11.7 cm | 23.2 cm | 21.7 cm |
| 12 | 11.4 cm | 10.4 cm | 21.4 cm | 20.4 cm |
| 13 | 12.8 cm | 11.8 cm | 22.8 cm | 21.8 cm |
| 14 | 11.0 cm | 9.5 cm | 21.0 cm | 19.5 cm |
| 15 | 12.4 cm | 10.4 cm | 22.4 cm | 20.4 cm |
| 16 | 10.6 cm | 8.6 cm | 20.6 cm | 18.6 cm |
| 17 | 12.0 cm | 10.5 cm | 22.0 cm | 20.5 cm |
| 18 | 10.2 cm | 9.2 cm | 20.2 cm | 19.2 cm |
| Mean | 11.5 cm | 10.0 cm | 21.5 cm | 20.0 cm |
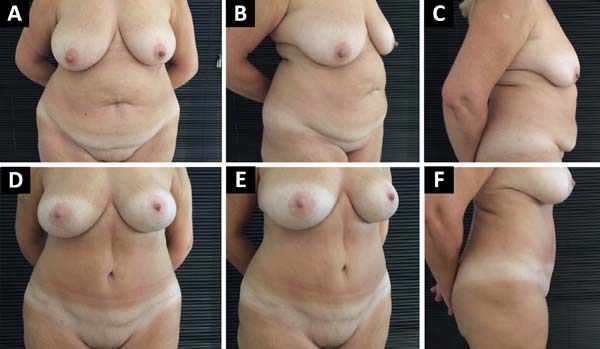
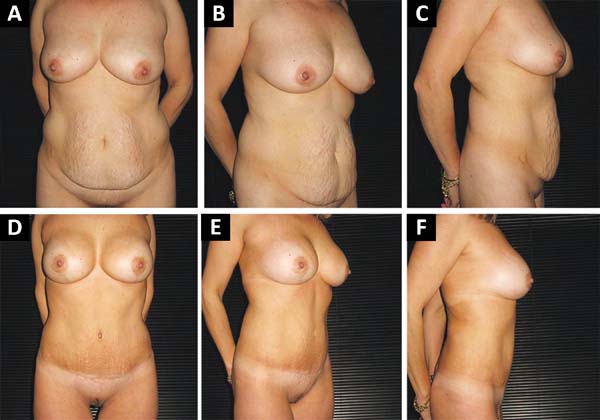
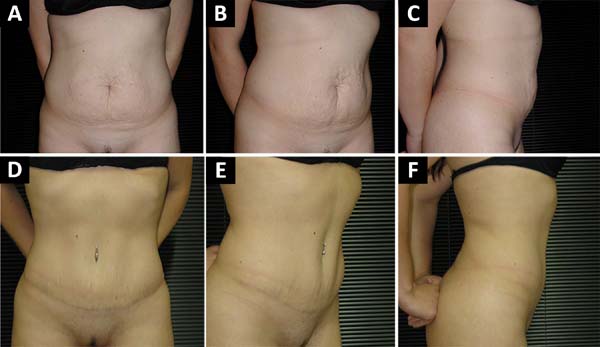
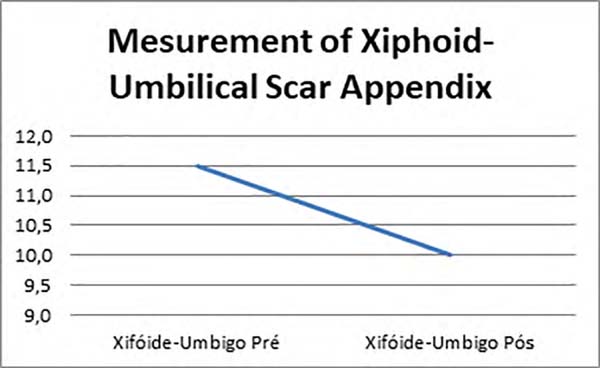
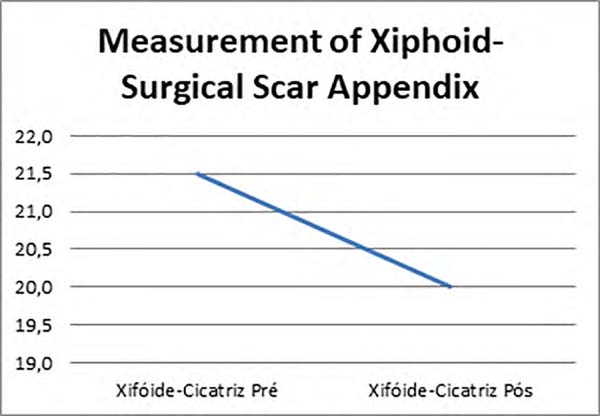
A decreased in the distance of the xiphoid-umbilical scar appendix and the xiphoid-surgical scar appendix (Figures 1, 2 and 3) was observed after the use of Baroudi adhesion points (Figures 4 and 5).
DISCUSSION
There have been complications associated with the evolution of abdominoplasty, especially for seroma and flap necrosis, which vary according to the case. The main cause of complications is the large displacement in classical surgery that sliced lymphatic and perforating vessels. To minimize such complications, various techniques were proposed to reduce dissections. Baroudi’s adhesion points were undoubtedly a simple and efficient solution to a frequent and sometimes complex problem. In abdominoplasty, the adhesion technique initially described by Baroudi and Ferreira to detached flaps is an effective method to eliminate seroma and use a suction drain7,8. Its benefits were reiterated by Nahas et al. in 20079, Pollock et al. in 200010, and Roje et al. in 200611.
Based on our study results, it was possible to refute the null hypothesis that there is no significant difference in distances with and without the use of Baroudi adhesion points.
The reduction in the distance of the xiphoid-umbilical scar appendix and xiphoid-surgical scar appendix was verified after the execution of Baroudi suture (mean 1.5 cm), assuming a reduction in scar tension and a reduction in the surgical scar distance of the xiphoid appendix at the expense of narrowing the distance between it and the umbilical scar.
Follow-up of these patients is necessary to verify the long-term postoperative scar evolution.
CONCLUSION
There was a decrease in the xiphoid-umbilical scar and xiphoid-abdominal scar distances after the Baroudi stitches on the abdominal flap, showing a lower tension on the scar after using these adhesion points. Further studies should be conducted to evaluate how these measures behave in the late postoperative period until scar maturation and if they actually correlate with a better-quality scar.
REFERENCES
1. Matarasso A, Swift RW, Rankin M. Abdominoplasty and abdominal contour surgery: a national plastic surgery survey. Plast Reconstr Surg. 2006 May;117(6):1797-1808. DOI: https://doi.org/10.1097/01.prs.0000209918.55752.f3
2. Baroudi R, Ferreira CA. Seroma: how to avoid it and how to treat it. Aesthet Surg J. 1988 Nov/Dec;18(6):439-41. DOI: https://doi.org/10.1016/S1090-820X(98)70073-1
3. Zimman OA, Butto CD, Ahualli PE. Frequency of seroma in abdominal lipectomies. Plast Reconstr Surg. 2001 Oct;108(5):1449-51. PMID: 11604669 DOI: https://doi.org/10.1097/00006534-200110000-00071
4. Nahas FX, Ferreira LM, Ghelfond C. Does Quilting Suture Prevent Seroma in Abdominoplasty?. Plast Reconstr Surg. 2007 Mar;119(3):1060-64;discussion:1065-6. DOI: https://doi.org/10.1097/01.prs.0000242493.11655.68
5. Andrades P, Prado A, Danilla S, et al. Progressive tension sutures in the prevention of postabdominoplasty seroma: a prospective, randomized, doublo-blind clinical trial. Plast Reconstr Surg. 2007 Sep;120(4):935-46;discussion:947-51. DOI: https://doi.org/10.1097/01.prs.0000253445.76991.de
6. Arantes HL, Rosique RG, Rosique MJ, Mélega JM. The use of quilting suture in abdominoplasty does not require aspiratory drainage for prevention of seroma. Aesthetic Plast Surg. 2010 Feb;34(1):102-4. DOI: https://doi.org/10.1007/s00266-009-9453-6
7. Baroudi R, Ferreira CA. Contouring the hip and the abdomen. Clin Plast Surg. 1996 Oct;23(4):551-72;discussion:572-3.
8. Baroudi R, Ferreira CA. Seroma: how to avoid it and how to treat it. Aesthetic Surg J. 1998 Nov/Dec;18(6):439-41. DOI: https://doi.org/10.1016/S1090-820X(98)70073-1
9. Nahas FX, Ferreira LM, Ghelfond C. Does quilting suture prevent seroma in abdominoplasty?. Plast Reconstr Surg. 2007;119(3):1060-6. DOI: https://doi.org/10.1097/01.prs.0000242493.11655.68
10. Pollock H, Pollock T. Progressive tension sutures: a technique to reduce local complications in abdominoplasty. Plast Reconstr Surg. 2000 Jun;105(7):2583-8;discussion:2587-8.
11. Roje Z, Roje Z, Karanovic N, Utrobicic I. Abdominoplasty complications: a comprehensive approach for the treatment of chronic seroma with pseudobursa. Aesthetic Plast Surg. 2006 Sep/Oct;30(5):611-5. DOI: https://doi.org/10.1007/s00266-004-0142-1
1. Santa Casa de Misericórdia de Porto Alegre, Porto Alegre, RS, Brazil.
2. Universidade Federal de Ciências da Saúde de Porto Alegre, Porto Alegre, RS, Brazil.
Corresponding author: Thiago Melo de Souza Rua Professor Annes Dias, 135, Centro Histórico, Porto Alegre, RS, Brasil. Zip Code: 90040-001. E-mail: thiagosouza.md@gmail.com
Article received: July 19, 2019.
Article accepted: September 01, 2019.
Conflicts of interest: none.







 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter