

Original Article - Year 2020 - Volume 35 -
Epidemiological profile of patients with skin cancer treated at the Regional Hospital of Asa Norte/DF - Brazil
Perfil epidemiológico de pacientes portadores de câncer de pele atendidos no Hospital Regional da Asa Norte/DF - Brasil
ABSTRACT
Introduction: Skin cancer is the most common neoplasm in the Brazilian population, corresponding to 30% of all malignant tumors registered in the country. Non-melanoma malignant tumors are the type of cancer with the highest incidence and prevalence in Brazil. Basal cell carcinoma (BCC) is the most common, accounting for between 70% and 75% of cases. Squamous cell carcinoma (SCC) accounts for 20% of cases. The objective is to determine the epidemiological profile, the types and subtypes found in the histopathological results, the surgical conduct and its effectiveness in patients with a suspected malignant skin lesion.
Methods: A retrospective descriptive study, based on the analysis of electronic medical records for resection of skin lesions suspected of malignancy, carried out by the Plastic Surgery team at the Regional Hospital of Asa Norte, Brasília/DF, from January 2012 to December 2016.
Results: 533 patients were submitted to surgery, being female (51.6%), with a mean age of 68.97 years and 84% diagnosed with basal cell carcinoma with solid subtype. The compromised margins reached 11% of the sample. The most prevalent reconstructions were primary closure and local flaps.
Conclusion: The epidemiological profile of patients treated with lesions suspected of skin cancer showed prevalence in women over 60 years with a history of sun exposure. The face was the most affected site, the nose being the most common topography. BCC is the most common type, and the circumscribed solid subtype was the most prevalent. The most used type of reconstruction was primary closure and local flap.
Keywords: Basal cell carcinoma; Skin cancer; Margin compromise; Excision margins; Surgical flaps; Plastic surgery.
RESUMO
Introdução: O câncer de pele é a neoplasia mais comum na população brasileira,
correspondendo a 30% de todos os tumores malignos registrados no país. Os
tumores malignos não melanoma são o tipo de câncer de maior incidência e
prevalência no Brasil. O carcinoma basocelular (CBC) é o mais comum,
correspondendo entre 70% e 75% dos casos. O carcinoma epidermóide (CEC)
responde por 20% dos casos. O objetivo é determinar o perfil epidemiológico,
os tipos e subtipos encontrados nos resultados de histopatológico, a conduta
cirúrgica e sua eficácia, dos pacientes com suspeita de lesão maligna de
pele.
Métodos: Estudo retrospectivo descritivo, baseado na análise de prontuário eletrônico
de ressecção de lesões de pele suspeitas de maligna, pela equipe da Cirurgia
Plástica do Hospital Regional da Asa Norte, Brasília/DF, no período de
janeiro de 2012 a dezembro de 2016.
Resultados: Foram submetidos à cirurgia 533 pacientes, sendo sexo feminino (51,6%), com
média de idade de 68,97 anos e 84% com diagnóstico de carcinoma basocelular
com subtipo sólido. As margens comprometidas atingiram 11% da amostra. As
reconstruções mais prevalentes foram fechamento primário e retalhos
locais.
Conclusão: O perfil epidemiológico dos pacientes atendidos com lesões suspeitas de
câncer de pele demonstrou prevalência em mulheres e acima de 60 anos, com
história de exposição solar. A face foi o local mais acometido, sendo o
nariz a topografia mais comum. O CBC é tipo mais comum e o subtipo sólido
circunscrito foi o mais prevalente. O tipo de reconstrução mais utilizado
foi o fechamento primário e o retalho local.
Palavras-chave: Carcinoma basocelular; Câncer de pele; Comprometimento de margem; Margens de excisão; Retalhos cirúrgicos; Cirurgia plástica
INTRODUCTION
Skin cancer is the most common neoplasm in the Brazilian population, corresponding to 30% of all malignant tumors registered in the country. Among skin tumors, the non-melanoma type has the highest incidence and lowest mortality1.
Skin cancer has a growing incidence, according to the National Cancer Institute (INCA), an official body of the Ministry of Health. National rates are 60 cases/100,000 inhabitants, with basal cell carcinoma (BCC) being the most common type, corresponding to 70-75% of cases. The most common subtype is nodular (1,2,3.
The second most common type of malignant skin tumor is squamous cell carcinoma (SCC), with 15 to 20% of cases. Mortality due to BCC and SCC is low, as they rarely metastasize. However, they are locally aggressive and recurrent4.
Melanoma represents only 3% of malignant neoplasms; nevertheless, it is the most aggressive and metastatic. It was estimated 6260 new cases for the year 20181-4, with 2,920 men and 3,340 women.
This study’s objectives were to verify the epidemiological profile, types, and surgical management of patients with suspected skin malignancy at the Plastic Surgery Unit of Hospital Regional da Asa Norte, Brasília / DF.
METHODS
This is a descriptive retrospective study, based on the analysis of electronic medical records (TRAKcare) of patients undergoing surgical treatment for resection of a suspected lesion of skin malignancy, by the Plastic Surgery team at the Regional Hospital of Asa Norte, Brasília / DF, from January 2012 to December 2016.
A database was created in the Excel program, including all patients who underwent resection of a lesion in the team’s operating room.
Inclusion criteria
Patients undergoing resection of lesions with clinical characteristics of malignancy;
Patients operated by the Plastic Surgery Unit team;
Minimum outpatient follow-up of at least six months after the operation;
Patients who needed hospitalization for a procedure in the operating room with sedation associated with local anesthesia or general anesthesia for resectioning skin lesions (exeresis, incisional biopsies, excisional biopsies, and enlarged compromised margin).
Anatomopathological result checked in a later consultation.
Exclusion criteria
Incomplete data in the medical record;
Patients undergoing the surgical procedure who did not come for postoperative follow-up;
Cases of low complexity that were operated in the small surgery outpatient clinic of Plastic Surgery at Hospital Regional da Asa Norte, with no need for sedation or general anesthesia and a minimum stay of 6 hours.
RESULTS
Five hundred thirty-three patients who underwent resection of a suspected lesion in the period met the selection criteria. Regarding gender, 273 were females (51.6%) and 260 males (48.4%), with a mean age of 68 years (range, 1 to 102 years) and 1,484 injuries (mean of 2.78 injuries/patient) were resected.
As for the location, 69% of resections were in the head and neck, followed by the upper limb (15%), trunk (13%), and only 2% lesions in the lower limb.
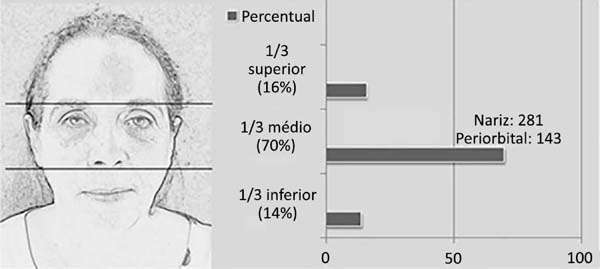
Considering the lesions located in the head and neck region, 975 (93%) were on the face, 47 (5%) on the scalp and 23 (2%) on the cervical region. Regarding the lesions located on the face, these preferentially affected the middle third of the face. The nose was the location with the highest number of resections, followed by the periorbital region (Table 1 and Figure 1).
| Head and neck regions | n. (%) | |
|---|---|---|
| Scalp | 23 (2%) | |
| Cervical region | 47 (5%) | |
| Face | 957 (93%) | |
| Total | 1027 (100%) | |
| Face location | n. (%) | |
| 1/3 upper face 153 (16%) | Front | 80 (8%) |
| Temporal | 73 (7%) | |
| 1/3 midface 669 (70%) | Julgar, Malar, zygomatic, buccinator | 124 (13%) |
| Periorbital | 143 (15%) | |
| Nose | 281 (29%) | |
| Ear | 121 (13%) | |
| 1/3 lower face 135 (14%) | Nasogenian | 29 (3%) |
| Mandible and chin | 44 (5%) | |
| Tongue and palate | 4 (0,5%) | |
| Lip | 58 (6%) | |
The results of the histopathological analysis identified that 188 (13%) resected lesions were benign, 377 (25%) pre-malignant (actinic keratosis), and 919 (62%) malignant. Among the malignant lesions, basal cell carcinoma 760 (84%) stood out, followed by squamous cell carcinoma 129 (14%).
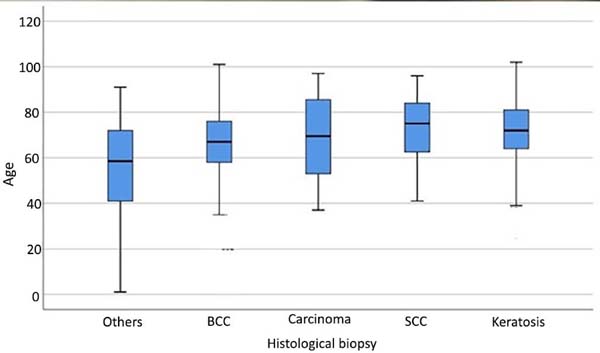
When the types of lesions were distributed by age, patients with BCC and pre-malignant lesions (keratoses) were a homogeneous group of older age, and basal squamous cell carcinoma showed greater age heterogeneity. On the other hand, younger patients were more frequent in other types of injuries (Figure 2).
The main subtypes identified for basal cell carcinoma were nodular in 520 cases (68%), superficial in 155 (20%), and sclerodermiform in 68 (9%). As for the margin compromised, 12% were compromised.
Regarding SCCs, 50% of the moderately differentiated SCC types were identified, followed by 33% well-differentiated SCC, 13% in situ SCC, and only 3% poorly differentiated SCC. Compromised margins were observed in less than 10%.
Only five cases of sarcoma were identified, one example of Marjolin’s ulcer and one case of cancer metastasis from another organ to the skin - a clear cell renal cell carcinoma (Figure 3).
Eight cases of malignant melanoma were found, and there was no margin compromise in the histopathological result (Table 2).
| Melanoma | n.8 |
|---|---|
| In situ | 1 |
| Lentigo maligna | 1 |
| Acral lentiginous melanoma | 2 |
| Superficial spreading malignant | 1 |
| Malignant | 1 |
| Nodular malignant | 2 |
The enlargement of the compromised margin was performed in 100 cases (11%), of which three had compromised margins again, being referred to the oncology service for complementary radiotherapy.
Regarding the surgical procedures for reconstruction of the defect created to the detriment of resection of the lesion, the majority (77%) needed only primary closure, 135 (9%) underwent skin graft, the majority being total skin (93%) of which the main donor area was the supraclavicular region and 188 (12%) flaps. Among the flaps consecrated for reconstruction, 47 flaps were medium-frontal/Indian, 40 nasogenian, 14 Limberg, and 12 retroauricular. The mid-frontal flap was used to reconstruct the nose, the inner canthus of the eye, and lower eyelid. Microsurgical flaps were performed in three reconstructions. Only six cases were submitted to closure by the second intention.
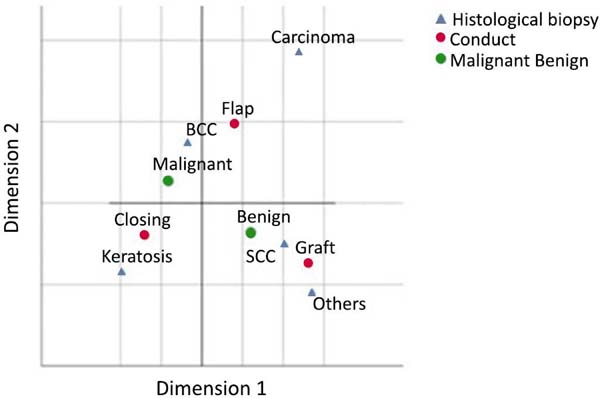
Through the perceptual map, it was verified that the grafts, in general, were more indicated when there was a result of histopathology of SCC, the flaps were more indicated in BCC and the primary closure in cases of BCC, actinic keratosis and benign lesions (Figure 4).
DISCUSSION
In the literature, we found a higher frequency of malignant skin neoplasia in men, but some studies show higher frequencies in women over 40 years of age. In our study, the average age was 68 years, affecting women more and being rare in children and blacks.
Those with previous skin diseases and light skin sensitive to sunlight (Fitzpatrick phototype I and II), burn scars, chronic ulcers, arsenic exposure, ionizing radiation, xeroderma pigmentosum, HPV infection and Gorlin and Bazex syndromes have risk factors that may be related to the appearance of BCC and SCC1-4.
The head and neck regions are the most affected by sun exposure and the chronic action of ultraviolet B rays (UVB), especially in tropical countries like Brazil1-4.
The most common skin cancer is BCC, which accounts for 70-80% of cases. Its most common subtype is nodular and the least aggressive. For 2018, 165,580 new cases were estimated, with 85,170 men, 80,410 women and 1,769 deaths.
The second most frequent is SCC. Melanoma is rarer, representing only 3% of malignant neoplasms. It is noteworthy that it is the most aggressive due to its high possibility of metastasis; data from this study reveal similarity with the literature1-7.
Early diagnosis is essential to avoid significant deformities resulting from the tumor and reduce the need for aggressive treatment methods.
The suggestive diagnosis is clinical and dermatoscopy can help. The definition of the histological type is made employing incisional or excisional biopsy for lesions above 1.0 cm8,9.
Treatments are the surgical procedure of tumor removal with a safety margin or the aid of freezing the piece in the intraoperative period or Mohs micrographic surgery, resulting in high efficacy with low recurrence10-11.
Curettage, electrocoagulation, liquid nitrogen cryosurgery, and 5% imiquimod and topical 5-fluoracil may be options for superficial BCC less than 1.0 cm8.
In patients without clinical conditions for surgical resection with extensive tumors, radiation therapy may be an alternative.
The margin recommended by the literature in the BCC is between 3-4 mm for circumscribed lesions, as in the nodular form, with a size smaller than 2 cm, and between 5-6 mm for tumors with poorly defined margins, such as superficial and infiltrative ones, or with size larger than 2cm.
While for SCC, margins are generally 4mm for the well-differentiated and 6mm for the undifferentiated.
In SCC with metastases and aggressive tumors with lymph node metastases, lymphadenectomy and complementary radiotherapy should be performed1-10.
We identified 11% of margin compromise in specimens, similarly reported by Su et al., in 20179. The index of margins compromised in the literature varies between 4% to 18%; its conduct is controversial in the literature10.
In melanoma, excisional biopsy is recommended as an initial approach. An incisional biopsy is acceptable for extensive lesions and/or in places where the entire lesion’s extraction causes a functional or aesthetic defect.
The enlargement of the margins of the primary lesion in melanoma varies according to the depth of invasion in millimeters (Breslow Index - Table 3)11-18. Sentinel lymph node biopsy is indicated if there are no clinical signs of lymph node involvement and one of the following factors: Breslow> 1mm; between 0.8mm and 1mm if mitotic index ≥ 1 / mm2, presence of ulceration or angiolymphatic invasion; and Breslow underestimated by a deep positive margin (Table 3)11-18.
| Tumor thickness (mm) | Margins (cm) |
|---|---|
| Melanoma in situ | 0,5 a 1cm |
| Breslow ≤ 1mm | 1cm |
| Breslow de 1,1 to 2mm | 1 to 2cm |
| Breslow > 2mm | 2cm |
Although there are established conducts for the treatment of skin cancer, there is no absolute consensus for all situations according to histological type, size, depth or location of the lesion, and aspects such as age, clinical conditions of the patient, aesthetic result, number lesions and whether the tumor is primary or recurrent.
CONCLUSION
In the treatment of skin cancer, multidisciplinary participation, and the plastic surgeon working with oncological principles are essential, performing tumor excision and reconstruction of the affected area to maintain function and restore aesthetics.
Our study showed a prevalence of females with a mean age of 68 years. The face is the most affected site, the nose being the most common topography. The circumscribed solid basal cell carcinoma was the most frequent subtype, and the most used type of reconstruction was primary closure. Such data corroborate the leading risk factor for non-melanoma skin cancer: chronic sun exposure.
REFERENCES
1. Barreiro G, Zanella FA, Rosa KGD, Calvett R, Senandes LS, Vizzotto MD, et al. O impacto de ações assistenciais na percepção da qualidade do Sistema Único de Saúde (SUS), Brasil: um estudo transversal. Rev Bras Cir Plást. 2016;31(2):242-5.
2. Instituto Nacional do Câncer (INCA). Estimativa 2012: incidência do câncer no Brasil [Internet]. Rio de Janeiro (RJ): INCA; 2012; [acesso em 2019 Jun 01]. Disponível em: http://www.inca.gov.br
3. Bariani RL, Nahas FX, Barbosa MVJ, Farah AB, Ferreira LM. Basal cell carcinoma: an updated epidemiological and therapeutically profile of an urban population. Acta Cir Bras. 2006 Mar/Abr;21(2):66-73.
4. Veríssimo P, Barbosa MVJ. Tratamento cirúrgico dos tumores de pele nasal em idosos. Rev Bras Cir Plást. 2009;24(2l):219-33.
5. Nasser N. Epidemiologia dos carcinomas basocelulares em Blumenau, SC, Brasil, de 1980 a 1999. An Bras Dermatol. 2005;80(4):363-8.
6. Carvalho MP, Oliveira Filho RS, Gomes HC, Veiga DF, Juliano Y, Ferreira LM. Auto-estima em pacientes com carcinomas de pele. Rev Col Bras Cir. 2007;34(6):361-6.
7. Maia M, Proença NG, Moraes JC. Risk factors for basal cell carcinoma: a case-control study. Rev Saúde Pública. 1995 Fev;29(1):27-37.
8. Chinem VP, Miot HA. Epidemiology of basal cell carcinoma. An Bras Dermatol. 2011;86(2):292-305.
9. Su SY, Giorlando F, Ek EW, Dieu T. Incomplete excision of basal cell carcinoma: a prospective trial. Plast Reconstr Surg. 2007 Out;120(5):1240-8.
10. Gregorio TCR, Sbalchiero JC, Leal PRA. Acompanhamento a longo prazo de carcinomas basocelulares com margens comprometidas. Rev Soc Bras Cir Plást. 2005;20(1):8-11.
11. Eliezri YD, Cohen PR. Cancer recurrence following Mohs micrographic surgery: a mechanism of tumor persistence. Plast Reconstr Surg. 1992 Jul;90(1):121-5.
12. Holmikvist K, Rogers G, Dahl P. A. Incidence of residual basal cell carcinoma in patients who appear free after biopsy. J Am Acad Dermatol. 2002;41(4):600-5.
13. Quintas RCS, Coutinho ALF. Fatores de risco para o comprometimento de margens cirúrgicas nas ressecções de carcinomas basocelular. Rev Bras Cir Plást. 2008;23(2):116-9.
14. Duz GL, Chagas JF, Faria JCM. Pesquisa de linfonodo sentinela em pacientes com melanoma cutâneo: correlação clínica e cintilográfica. Rev Bras Cir Plást. 2007;22(2):76-80.
15. Hayes AJ, Maynard L, Coombes G, Newton-Bishop J, Timmons M, Cook M, et al. Wide versus narrow excision margins for high-risk, primary cutaneous melanomas: long-term follow-up of survival in a randomized trial. Lancet Oncol. 2016 Fev;17(2):184-92.
16. Gershenwald JE, Scolyer RA, Hess KR, Sondak VK, Ling GV, Ross MI, et al. Melanoma of the skin. In: Amin MB, Edge SB, Greene FL, eds. AJCC Cancer Staging Manual. 8th ed. New York: Springer International Publishing; 2017. p. 563-85.
17. Gershenwald JE, Scoyler RA, Hess KR et al. American Joint Committee on Cancer (AJCC) on Cancer Staging Manual [Internet]. 8th Edition, 2016; [acesso em 2019 Ago 10]. Disponível em: http//www.cancerstaging.org
18. Gomes MWS, Galvão M, Moreira M, Caiado B, Cheldid R, Graziosi G. Perfil das reconstruções microcirúrgicas no INCA: análise retrospectiva de 46 casos. Rev Bras Cir Plást. 2012;27(3):35.
1. Hospital Regional da Asa Norte, Plastic
Surgery Unit, Brasília, DF, Brazil.
AVRFN Analysis and/or data interpretation, Realization of operations and/or trials
JLM Analysis and/or data interpretation, Writing - Review & Editing
CGF Realization of operations and/or trials
JLON Realization of operations and/or trials
MAPC Realization of operations and/or trials
Corresponding author: Altino Vieira de Rezende Filho Neto SMAS Trecho 1, Lote C, Bloco J, Apart. 703, Park Sul Guara, Brasília, DF, Brazil. Zip Code: 71218-010 E-mail: altinofn@hotmail.com
Article received: September 22, 2019.
Article accepted: July 15, 2020.
Conflicts of interest: none.










 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter