

Original Article - Year 2020 - Volume 35 -
Cephalic vein transposition for head and neck microsurgical reconstruction: anatomical study in cadavers
Transposição da veia cefálica para reconstrução microcirúrgica de cabeça e pescoço: estudo anatômico em cadáveres
ABSTRACT
Introduction: Cephalic vein transposition is an interesting
alternative as a donor vein in head and neck cancer reconstruction
in patients with a cervical radiotherapy history. This work aims
to evaluate the cephalic vein anatomical characteristics in
cadavers.
Methods: Six cephalic veins from three cadavers
were dissected. The veins were sectioned in the medial part of
the arm and transposed to the neck over the clavicles.
Results: The veins had an average length of 18.75 ± 1.84 cm and several
tributaries with a variation of 7-9. The diameter coincided in both
veins of each corpse. The anatomical parameter used to identify
them (deltopectoral groove) proved reliable, allowing predictable
dissection.
Conclusion: The cephalic vein has constant
characteristics and is easy to locate, being an option relevant
to the reconstructive plastic surgeon's therapeutic arsenal.
Keywords: Head and neck neoplasms; Reconstructive surgical procedures; Microsurgery; Autologous transplantation; Radiotherapy.
RESUMO
Introdução: A transposição de veia cefálica é uma alternativa interessante como veia doadora na reconstrução oncológica de cabeça e pescoço em pacientes com história de radioterapia cervical. O objetivo do trabalho é avaliar as características anatômicas da veia cefálica em cadáveres.
Métodos: Foram dissecadas seis veias cefálicas de três cadáveres. As veias foram seccionadas na parte medial do braço e transpostas até o pescoço por cima das clavículas.
Resultados: As veias apresentaram média de comprimento de 18,75±1,84cm e número de tributárias com variação de 7-9. O diâmetro coincidiu em ambas as veias de cada cadáver. O parâmetro anatômico usado para identificá-las (sulco deltopeitoral) se mostrou confiável, possibilitando uma dissecação previsível.
Conclusão: A veia cefálica tem características constantes e fácil localização, sendo uma opção relevante ao arsenal terapêutico do cirurgião plástico reconstrutor.
Palavras-chave: Neoplasias de cabeça e pescoço; Procedimentos cirúrgicos reconstrutivos; Microcirurgia; Transplante autólogo; Radioterapia
INTRODUCTION
Head and neck cancers, closely related to alcoholism and smoking, have a significant prevalence in the Brazilian population. There was an increase in this type of cancer from 5.82 per 100 thousand inhabitants in 2000 to 11.54 in 2008, with squamous cell carcinoma being the most common histological type1. Only in 2008, 21,875 new cases were diagnosed1. A more recent study found 220,390 cases diagnosed between 2000 and 20142. Transposition of free flaps is one of the techniques of choice in head and neck cancer reconstruction3. The great vascularization of this region would generally allow microvascular anastomoses with cervical receptor vessels. However, many of these patients undergo adjuvant radiotherapy. Radiotherapy significantly changes the region’s vascular permeability, making it challenging to use recipient vessels (mainly veins) for the microsurgical flap3.
The grafting of veins from other parts of the body, such as the saphenous vein, is the standard choice in this situation reported above4. However, this option requires two anastomoses in the grafted vein; one in the recipient’s vessel and another in the vein of the flap itself. Thus, increasing the risk of thrombosis and the surgical time and increasing the failure rate of reconstruction4.
An alternative to vein grafting is the cephalic vein transposition5 because the cephalic vein is located far from the region undergoing radiotherapy. Furthermore, it has a relatively constant course and caliber, in addition to a slightly variable number of tributaries. The cephalic vein is extremely useful in head and neck reconstruction4,5. This venous transposition requires only a cervical anastomosis in the flap with a lower risk of thrombosis and less execution time.
OBJECTIVE
To evaluate the cephalic vein anatomical characteristics in cadavers for cervical transposition and its use in microsurgical flaps.
METHODS
Cadavers
The present study is primary. Six cephalic veins from three cadavers were dissected: a 71-year-old woman and two men, 50 and 62 years old, at the death verification service of the Faculdade de Medicina da Universidade de São Paulo (SVO-FMUSP), from October to December 2019. The Universidade Federal de São Paulo Research Ethics Committee (CEP analyzed and approved this study under number 0675/2019, after its registration at Plataforma Brasil.
Surgical technique
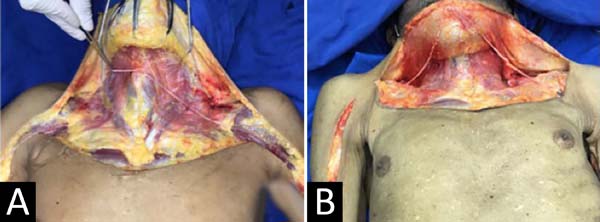
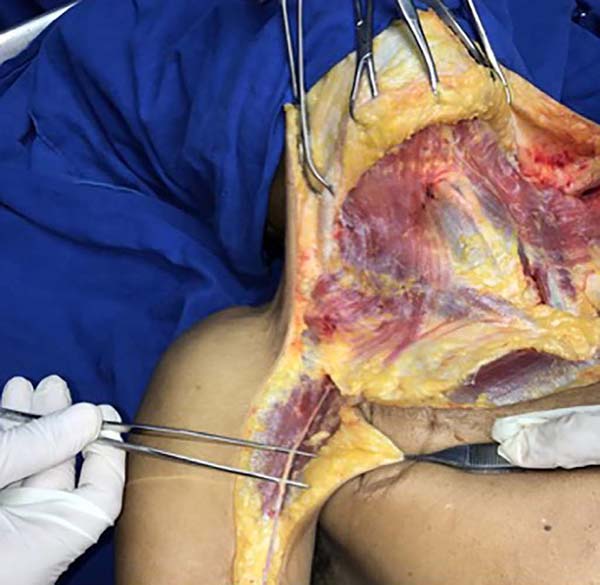
First, the deltopectoral groove was identified to delimit the incision; the cut was made between 1 and 2 cm lateral to the groove to avoid direct injury to the cephalic vein. The distal incision progressed to the humeral mid-level, on the arm’s lateral surface (usual topography of the cephalic vein). When identified the vein, its tributaries and the distal vein were connected, besides rotating the axilla from distal to proximal (Figures 1 and 2). The vein was transposed up to the neck over the clavicle, as shown in Figure 3.
RESULTS
The veins had an average length of 18.75 ± 1.84cm and the number of tributaries with a variation of 7-9. The diameter coincided in both veins of each cadaver, as shown in Table 1. The anatomical parameter used to identify them (deltopectoral groove) proved reliable, allowing predictable dissection.
| Cephalic Vein | Side | Gender | Age | Height\Weight (m\Kg) | No. of Tributaries | Length (cm) | Diameter (mm) |
|---|---|---|---|---|---|---|---|
| 1 | D | Male | 50 | 1,60\71 | 8 | 19 | 4 |
| 2 | E | Male | 50 | 1,60\71 | 7 | 19,5 | 4 |
| 3 | D | Male | 62 | 1,63\62 | 9 | 20,3 | 3 |
| 4 | E | Male | 62 | 1,63\62 | 8 | 18,9 | 3 |
| 5 | D | Female | 71 | 1,52\55 | 7 | 17,8 | 3 |
| 6 | E | Female | 71 | 1,52\55 | 8 | 17 | 3 |
DISCUSSION
Head and neck oncological reconstruction went through different stages. In the 40s, there were several attempts to correct these defects with local flaps and skin grafts, which did not show good long-term results, evolving with orofacial fistulas, dehiscences, necroses, and complex deformities resulting from reconstruction6. Other options have emerged over time, such as the temporofrontal pedicled flap7 and the pectoralis major myocutaneous flap8. However, the difficulty of axial rotation and the fact that there is little available tissue adjacent to the lesion caused free flaps to emerge as one of the main options for reconstruction in these cases9. They are more advantageous than pedicled axial flaps, as they allow better blood supply, less tension, greater malleability, moldability and tissue extension for reconstruction1,2.
In patients who have not undergone previous radiotherapy or surgical treatment, it is possible to use the neck and face’s recipient vessels, such as branches of the external carotid artery and tributaries of the internal jugular vein or the external jugular vein10. The transposition of veins in the thoracic region has been a viable option to circumvent vascularization impairment in patients undergoing cervicofacial radiotherapy10,11.
In this described technique, the transposed cephalic vein will be anastomosed to the flap vein, making a single anastomosis, reducing the risk of thrombosis, and decreasing the reconstruction’s failure rate. There are several possible options for vessels to be transposed. In addition to the cephalic vein, we have the thoracodorsal vein and the transverse cervical vein11. Among these options, the cephalic vein is one of the main alternatives, as it has an adequate diameter, predictable dissection and is located farther from the usual radiotherapy site for head and neck cancer12,13.
Our work corroborated data from the literature, showing the constant profile of the vein concerning the caliber and length, in addition to the little variable number of tributaries. It allows excellent venous drainage and is generally free from radiotherapy ablation due to its lateral thoracic location.
The literature has several reports on the successful use of the cephalic vein11,13,14, which confirms this technique as a reliable option in head and neck reconstruction.
CONCLUSION
The transposition of the cephalic vein is an interesting option for head and neck cancer reconstruction, as it has constant characteristics and a predictable location and maybe a suitable technique to the therapeutic arsenal of the reconstructive plastic surgeon.
REFERENCES
1. Casati MFM, Vasconcelos JA, Vergnhanini GS, Contreiro PF, Graça BT, Kanda JL, et al. Head and neck cancer epidemiology in Brazil: populational based cross-sectional study. Rev Bras Cir Cabeça Pescoço. 2012 Out/Dez;41(4):186-91.
2. Carvalho LGA, Santiago CPL, Andrade ACM, Valença AMG, Riveiro ILA, Castro RD. El câncer de cabeza y cuello en Brasil: un análisis de 15 años. Rev Cubana Estomatol. 2018 Out;55(3):22-8.
3. Hanasono MM, Barnea Y, Skoracki RJ. Microvascular surgery in the previously operated and irradiated neck. Microsurgery. 2009;29:1-7.
4. Maricevich M, Lin LO, Liu J, Chang EI, Hanasono MM. Interposition vein grafting in head and neck free flap reconstruction. Plast Reconstr Surg. 2018 Out;142(4):1025-34.
5. Chan D, Rabbani CC, Inman JC, Ducic Y. Cephalic vein transposition in the vessel-depleted neck. Otolaryngol Head Neck Surg. 2016;155(2):367-8.
6. McGregor IA. The pursuit of function and cosmesis in managing oral cancer. Br J Plast Surg. 1993 Jan;46(1):22-31.
7. McGregor IA. The temporal flap in intra-oral cancer: its use in repairing the post-excisional defect. Br J Plast Surg. 1963 Out;16:318-35.
8. Ariyan S. The pectoralis major myocutaneous flap. A versatile flap for reconstruction in the head and neck. Plast Reconstr Surg. 1979 Jan;63(1):73- 81.
9. Vanni CMRS, Pinto FR, Castro R, Kanda JL. Pedicle temporofrontal flap for head and neck reconstruction. Arq Bras Ciên Saúde. 2010 Mai/Ago;35(2):99-102.
10. Rinaldo A, Shaha AR, Wei WI, Silver CE, Ferlito A. Microvascular free flaps: a major advance in head and neck reconstruction. Acta Otolaryngol. 2002;122(7):779-84.
11. Vasilakis V, Patel HDL, Chen HC. Head and neck reconstruction using cephalic vein transposition in the vessel-depleted neck. Microsurgery. 2009 Jun;29(8):598-602.
12. Kubo T, Yano K, Hosokawa K. Management of flaps with compromised venous outflow in head and neck microsurgical reconstruction. Microsurgery. 2002;22(8):391-5.
13. Chan D, Rabbani CC, Inman JC, Ducic Y. Cephalic vein transposition in the vessel-depleted neck. Otolaryngol Head Neck Surg. 2016;155(2):367-8.
14. Inoue T, Fujino T. An upper arm flap, pedicled on the cephalic vein with arterial anastomosis, for head and neck reconstruction. Br J Plast Surg. 1986 Oct;39(4):451-3.
1. Federal University of the São Paulo, São Paulo, SP, Brazil.
RGFF Realization of operations and/or trials, Writing - Original Draft Preparation, Writing - Review & Editing
PNGD Resources, Writing - Original Draft Preparation
ACL Analysis and/or data interpretation, Investigation, Resources
FMVW Realization of operations and/or trials, Supervision
AWC Analysis and/or data interpretation, Formal Analysis, Supervision
JAM Formal Analysis, Supervision
LMF Final manuscript approval, Project Administration, Supervision
Corresponding author: Roney Gonçalves Fechine Feitosa, Rua Borges Lagoa 1083, Sala 62, Vila Clementino, SP, Brazil. Zip Code: 04038-032. E-mail: roneyfechine@gmail.com
Article received: April 27, 2020.
Article accepted: July 19, 2020.
Conflicts of interest: none








 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter