

Original Article - Year 2020 - Volume 35 -
Non-syndromic craniosynostosis: a retrospective analysis
Craniossinostoses não sindrômicas: uma análise retrospectiva
ABSTRACT
Introduction: Craniosynostoses are defined as premature
fusions of one or more cranial sutures. They can be classified
according to the sutures involved, correlated malformations
and genetic alterations, and maybe syndromic or not. Its
incidence is estimated at 1: 2,000-2,500 live births, with only
8% being syndromic. There are multiple surgical options
for the correction of these malformations, and early referral
to specialized centers for the treatment of these patients is
necessary for a better therapeutic indication. The diagnosis
is based on physical examination and computed tomography.
The surgical treatment brings significant aesthetic and
social improvements to patients. The objective is to analyze
retrospectively patient data who underwent surgery to
correct craniosynostosis at HC of UNESP-Botucatu.
Methods: Retrospective analysis of the medical records of patients who
underwent surgical correction of craniosynostosis between
2012 and 2017.
Results: The prevalence of scaphocephaly
and trigonocephaly was the same (38.5%). The mean age of
the approach was 24 months; the mean surgical time was
3h48min, lower in scaphocephaly, 2h50min. All patients
received blood transfusions in the perioperative period, with
a mean percentage of 24.9% in relation to the preoperative
blood volume. They underwent postoperative in a pediatric
ICU. There were no deaths or complications, and the results
were considered good by the team and family.
Conclusion: Open surgical treatment of non-syndromic craniosynostosis
is a safe procedure. Plastic surgery teams can achieve
results comparable to those described in the literature,
with low complication rates, good aesthetic results when
performed correctly and with a multidisciplinary approach.
Keywords: Craniosynostoses; Surgery, Plastic; Craniofacial abnormalities; Blood transfusion; Skull.
RESUMO
Introdução: Craniossinostoses são definidas como fusões prematuras de uma ou mais suturas cranianas. Podem ser classificadas de acordo com as suturas envolvidas, malformações correlacionadas e alterações genéticas, podendo ser sindrômicas ou não. Sua incidência estimada em 1:2.000-2.500 nascidos vivos, sendo apenas 8% sindrômicas. Existem múltiplas opções cirúrgicas para a correção destas malformações, e o encaminhamento precoce para centros especializados no tratamento destes doentes é necessário para uma melhor indicação terapêutica. O diagnóstico é pautado no exame físico e tomografia computadorizada. O tratamento cirúrgico traz melhoras significativas estéticas e no convívio social dos pacientes. O objetivo é analisar os dados, retrospectivamente, dos pacientes submetidos à cirurgia para correção de craniossinostoses, no HC da UNESP-Botucatu.
Métodos: Análise retrospectiva dos prontuários de pacientes submetidos à correção cirúrgica de craniossinostoses entre 2012 e 2017.
Resultados: A prevalência de escafocefalia e trigonocefalia foi igual (38,5%), idade média de abordagem de 24 meses, o tempo cirúrgico médio foi de 3h48min, sendo menor nas escafocefalias, 2h50min. Todos os pacientes receberam transfusão de sangue no perioperatório com média percentual em relação ao volume sanguíneo pré-operatório de 24,9% e fizeram pós-operatório em UTI pediátrica. Não houve óbitos ou complicações, e os resultados tidos como bom pela equipe e familiares.
Conclusão: O tratamento cirúrgico aberto das craniossinostoses não sindrômicas é um procedimento seguro. As equipes de cirurgia plástica conseguem alcançar resultados equiparáveis aos descritos na literatura, com baixas taxas de complicações, bom resultado estético, quando executado de maneira adequada, e com abordagem multidisciplinar.
Palavras-chave: Craniossinostoses; Cirurgia plástica; Anormalidades craniofaciais; Transfusão de sangue; Crânio
INTRODUCTION
Craniosynostosis is defined as an abnormal growth of the skull due to the premature fusion of one or more cranial sutures. They can be classified according to the sutures involved, correlated malformations, and maybe random or linked to syndromes and genetic changes. Its estimated incidence is 1: 2,000-2,500 live births1, with only 8% being syndromic or a family pattern2.
The sagittal suture is most commonly affected in non-syndromic craniosynostosis, and the cause is not known. Possibly spontaneous mutations in a gene occur, but other risk factors involved are: fetal constriction (nulliparity, multiple pregnancy, and macrosomia), low birth weight, preterm birth, maternal use of valproate, and hydrocephalus with shunt3,4.
When a suture closes early, the vault has restricted perpendicular growth, growing only parallel to this suture. This fact is known as Virchow’s law5. The classification of non-syndromic craniosynostosis is based on the affected suture. The sagittal synostosis, known as scaphocephaly, determines that the skull has the shape of a “boat” with the increase of the anteroposterior dimension. The bicoronal synostosis, known as brachycephaly, produces a flattened head that is determined by the increase in biparietal diameter. Metopid synostosis determines the skull in a triangular shape or trigonocephaly. Plagiocephaly is the general term that denotes asymmetry in the coronal plane. It may be anterior when the synostosis is unilateral coronal (right or left) or posterior when the synostosis is lambdoid (right or left), this one being a rarer form5.
There are multiple surgical options for the correction of these malformations. Early referral to a specialized center for these patients’ treatment is necessary for a better therapeutic indication. The basis for diagnosis is physical examination. However, there is often a delay in identifying this disease, especially in mild cases, when the shape of the head is not clearly abnormal, in symmetrical cases, with postnatal fusion, or due to the lack of knowledge of the attending professional6
After physical examination using craniometric measurements, we proceeded to the image diagnosis when there is a clinical suspicion of craniosynostosis. It is based on computed tomography with three-dimensional reconstruction, evaluating the fused suture, ventricular size, corpus callosum defects, and signs suggestive of increased ICP (intracranial pressure), such as “thumbprinting” or “beaten silver” patterns, loss of swollen folds and blunt cisterns. The increase in ICP is more common in multiple suture fusions or syndromic craniosynostosis7-9
Failure to treat patients can generate severe psychosocial losses for children when interacting with others during development, with repercussions in adult life. The increase in ICP is controversial in non-syndromic craniosynostosis cases, but some studies demonstrate this increase with rates varying between 4.5-24% of those affected10,11.
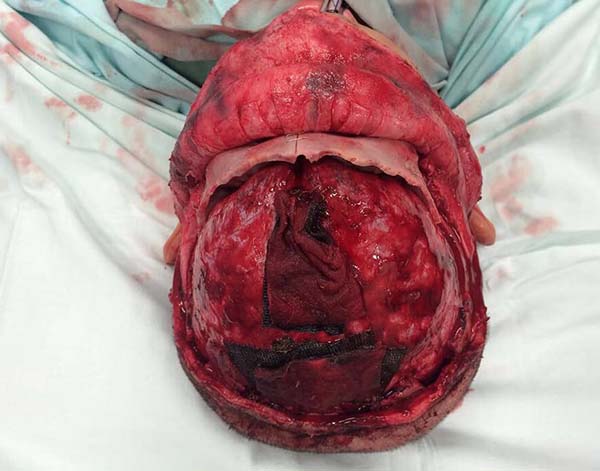
The literature points to several treatment philosophies, such as the total open reconstruction of the skullcap, minimally invasive craniectomy using a postoperative helmet, minimally invasive craniectomy using springs, and cranial distractors12-14. Each procedure has positive and negative points. Our service’s choice is due to the open reconstruction technique, which allows the removal of deformed portions, remodeling, and bone repositioning, with the possibility of extensive repairs, various osteotomies, and a single surgical time. The shape of osteotomies depends on the deformity presented and is discussed on a case-by-case basis.
With the proper care and perioperative management, it is possible to perform these complex procedures with low rates of complications15.
OBJECTIVE
The objective of this work is to retrospectively analyze data from patients with non-syndromic craniosynostosis surgically treated at the Hospital das Clínicas of UNESP-Botucatu together by the plastic surgery and neurosurgery teams.
METHODS
Data collection was performed by reviewing the medical records of patients diagnosed with non-syndromic craniosynostosis, carried out between 2012 to 2017 at the Hospital das Clínicas da Faculdade de Medicina de Botucatu.
The data collected were age, type of craniosynostosis, date, type and duration of surgery, blood transfusions, length of stay in the ICU, postoperative complications, neuropsychomotor development (NPMD).
We assessed if there was a delay in the NPMD to analyze each age group’s expected frames according to the child’s card and recommendations from the Ministry of Health16.
All surgeries were performed with sinuous bicoronal access for adequate exposure of the osteotomy areas. Osteosyntheses were performed with steel wires, not being necessary in cases of isolated scaphocephaly. Patients underwent the postoperative period in a pediatric ICU bed, and all required blood transfusion.
The institution’s ethics committee approved the work through report 3,524,698.
RESULTS
Patients’ mean age at surgery was 24 months, with a median of 16 months, a standard deviation of 24.63, and a confidence interval of 0.693 (p> 0.05).
The types of craniosynostosis found were five scaphocephaly (38.5%), five trigonocephaly (38.5%), two plagiocephalies (15.4%), and an association between plagiocephaly and scaphocephaly (7.6%) (Figures 1 to 5).
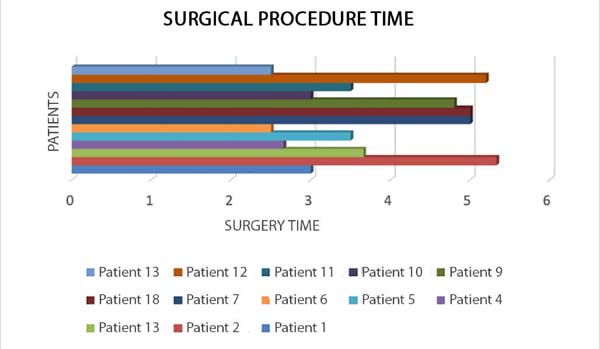
The surgical time varied between 2h30min and 5h20min, with an average of 3h48min, and the scaphocephaly required shorter procedure time, with variation between 2h30min and 3h30min (Figure 6).
Postoperative mortality and postoperative complication rate were 0%.
Blood transfusions were performed in all procedures, with a mean percentage of transfused blood of 24.9% in relation to the preoperative blood volume (Table 1).
| Pacient | Classification | Weight (KG) | Transfusion (Ml) | Percentage in Relation to Initial Blood Volume |
|---|---|---|---|---|
| 1 | Trigonocephaly | 8.1 | 120 | 18.50% |
| 2 | Plagiocephaly | 14.5 | 289 | 24.90% |
| 3 | Trigonocephaly | 13.1 | 200 | 20.30% |
| 4 | Scaphocephaly | 8 | 240 | 37.50% |
| 5 | Trigonocephaly | 8.3 | 100 | 15% |
| 6 | Scaphocephaly | 9.6 | 100 | 13% |
| 7 | Trigonocephaly | 15 | 218 | 19.40% |
| 8 | Plagiocephaly + Scaphocephaly | 7 | 376 | 67.10% |
| 9 | Plagiocephaly | 27 | 244 | 12.00% |
| 10 | Scaphocephaly | 9 | 150 | 20.80% |
| 11 | Scaphocephaly | 9.2 | 346 | 47.00% |
| 12 | Trigonocephaly | 13 | 149 | 15.30% |
| 13 | Scaphocephaly | 9.4 | 102 | 13.50% |
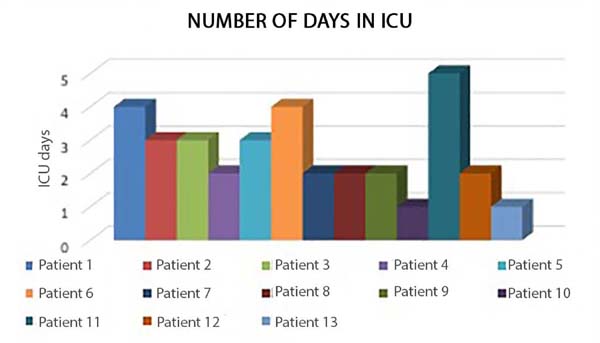
The children’s intensive care unit’s stay ranged from 1 to 5 days, with an average of 2.6 days of stay (Figure 7).
As for the aesthetic result and the need for surgical revision, considering the Whitaker classification, 12 were classified as level I and one as level II. The latter is awaiting a new procedure17.
NPMD delay occurred in 4 out of 13 patients, with a slight degree of delay (30%), in 2 of them related to speech.
DISCUSSION
The craniofacial surgical procedures and the possible morbidities associated with surgical techniques and general anesthesia are of great concern and discussion among specialists. Blood loss and subsequent change in coagulability are still the main mortality factors in children’s surgeries due to lower blood volume and higher energy expenditure. Regarding anesthesia, the risk of laryngeal and bronchospasm is higher in this population. However, with advances in surgical techniques and anesthetic care, the literature has shown that craniosynostosis surgeries are safe, with reduced rates of complications and mortality18-20.
With a mean of 24 months (p> 0.693), the patients’ age of approach was above the reports in the literature. This fact occurred due to a surgery performed on a child who was eight years and three months old, as he missed outpatient follow-up and returned at an advanced age, wanting surgery for aesthetic reasons. But even with a high average, the results were considered good by the surgical team5,21-23.
There was the same prevalence between scaphocephaly and trigonocephaly in our case series, with 5 cases (38.5%), differing from the literature that reports a higher prevalence of scaphocephaly1,2,15.
There has been an increase in the discussion about treatment with minimally invasive procedures, which would require less surgical time and less blood loss; however, there is a need for two or more approaches17,24. The treatment proposed in this series of cases showed good results for evaluating family members and staff and being reported as regular in only one scaphocephaly case, which kept the frontal region not very prominent, with quantified improvement by 70% by family members and discussion of a second future intervention. Therefore, according to Whitaker’s classification of surgical revision and result, where level I does not need new approaches, II the patient is submitted to soft tissue or small osteotomy correction, in III it is necessary osteotomies or larger bone grafts, and in IV, a new craniotomy and/or fronto-orbital remodeling is indicated; 12 patients are at level I and one of them at III, awaiting a new procedure17.
The complication rate was extremely low, with no case of infection in the postoperative period, with 0% mortality. Only one patient presented temporary convergent strabismus, returning to normal without the need for intervention and keeping our rates comparable to those found in the literature concerning mortality and lower in complications15,22,25,26.
The fixation of bone grafts can be performed with non-absorbable or absorbable materials to allow the growth of the skullcap15. The use of steel wires is the approach used in our service. Possible complications are extrusion, palpation, and intracranial translocation. The latter occurs due to the internal board’s bone resorption, with deposition on the external one during cranial development. However, they have a low incidence without related symptoms. Associated with these factors, the high cost and the learning curve for using absorbable materials justify our choice for steel wires. Isolated scaphocephaly was treated without fixation after osteotomies27.
Bleeding, a source of great concern occurs after the incision and comes from the scalp, skullcap, and dura. The presence of dural bone adhesions and the possible laceration of venous sinuses during craniotomy are imminent risk factors for difficult to control hemorrhage6,28. Blood transfusions were performed in all procedures, with an average transfused volume rate of 24.9% in relation to the patient’s blood volume, preoperatively; this rate is lower than studies that analyze the repairing technique craniosynostosis with open surgery22,29,30.
Although there are reports in the CSF fistula literature, we did not have this complication in our surgeries. The main associated risk factors are re-approaches due to fronto-orbital adhesions and distractions, which explains the absence in the sample presented, since such procedures were not performed31,32.
Most specialists recommend the postoperative period performed in a pediatric ICU. We consider it necessary for patients’ best control, with fine adjustment of the hydro electrolytic balance and ventilatory weaning 5,15,21,22. The unit’s stay ranged from 1 to 5 days, with an average of 2.6 days, longer than the one found, one day33.
The average surgical time of 3 hours and 48 minutes is above that reported in the reviewed publications. However, in the articles analyzed, the decrease in time is due to the fixation of biodegradable materials using ultrasound, which can reduce this step’s duration by 50%22,34. Another factor influencing the procedure’s time is that the surgeries were performed by residents, still on a learning curve35.
Several techniques are described for osteotomies in each specific type of craniosynostosis. The patients’ planning and approach are made by the craniofacial surgery team, which has neurosurgeons and plastic surgeons. Each case is evaluated, and the osteotomies are individually planned against the defect presented by the patient. We believe that in this way, the best results are obtained.
The patients’ follow-up varied between 10 months and six years, with a great psychosocial impact on the children approached. The follow-up to adulthood will answer the final repercussion of craniosynostosis correction in patients’ interpersonal relationships.
Much is discussed about the neurological repercussions in non-syndromic craniosynostosis, increased ICP, and delayed neuropsychomotor development, especially concerning disorders related to speech language1,2,7,11,36. In our retrospective analysis, we noted a considerable prevalence of NPMD delay, with 4 out of 13 patients showing a mild degree of delay (30%), in two of them related to speech. Three were older than 24 months. Two underwent surgical correction for trigonocephaly, one for scaphocephaly, and one for plagiocephaly, corroborating the findings by Kljajic et al. in 201934.
This study’s limitations were mainly the low number of cases analyzed, but this may reflect the difficulty of diagnosis and even access to consultations and referrals, which patients find in the public network. Another limitation is the fact that this study is retrospective, based on the analysis of medical records.
CONCLUSION
The conventional open treatment of non-syndromic craniosynostosis brings good results, comparable to those existing in the literature, with low rates of complications when appropriately performed, showing to be a safe technique. Even older children can benefit from the surgical procedure.
Despite a small sample, the article shows good results compared to articles already published and denotes the importance of standardization of accesses and techniques, with multidisciplinary involvement and discussion.
REFERENCES
1. Di Rocco F, Arnauld E, Renier D. Evolution in frequency of non-syndromic craniosynostosis. J Neurosurg Pediatr. 2009 Jul;4(1):21-5.
2. Lajeunie E, Crimmins DW, Arnaud E, Renier D. Genetic considerations in nonsyndromic midline craniosynostoses: a study of twins and their families. J Neurosurg. 2005 Out;103(4 Supl 1):353-6.
3. Sanchez-Lara PA, Carmichael SL, Graham Junior JM, LAmmer EJ, Shaw GM, Ma C, Rasmussen SA. Fetal constraint as a potential risk factor for craniosynostosis. Am J Med Genet A. 2010 Fev;152(2):394-400.
4. Singh RP, Dhariwal D, Bhujel N, Shaikh Z, Davies P, Nishikawa H, et al. Role of parental risk factors in the aetiology of isolated non-syndromic metopic craniosynostosis. Br J Oral Maxillofac Surg. 2010 Set;48(6):438-42.
5. Governale LS. Craniosynostosis. Pediatr Neurol. 2015 Nov;53(5):394-401.
6. Ghizoni E, Denadai R, Raposo-Amaral CA, Joaquim AF, Tedeschi H, Raposo-Amaral CE. Diagnóstico das deformidades cranianas sinostóticas e não sinostóticas em bebês: uma revisão para pediatras. Rev Paul Pediatr. 2006 Dez;34(4):495-502. DOI: https://doi.org/10.1016/j.rppede.2016.02.005
7. Selber J, Reid RR, Chike-Obi CJ, Sutton LN, Zackai EH, Mc-Donald MD, et al. The changing epidemiologic spectrum of single-suture synostoses. Plast Reconstr Surg. 2008;122:527-33.
8. CostaVal JA, Mandic LF, Gusmão SN. Head measurements for the diagnosis of craniosynostosis. Arq Bras Neurocir. 2017 Abr;36(2):91-5.
9. Palhares A. Cranioestenoses e craniofaciestenoses. In: Mélega JM, Viterbo F, Mendes FH, eds. Cirurgia plástica - os princípios e a atualidade. Rio de Janeiro: Guanabara Koogan; 2011. p. 481-7.
10. Wall SA, Thomas GP, Johson D, Byren JC, Jayamohan J, Magdum SA, et al. The preoperative incidence of raised intracranial pressure in nonsyndromic sagittal craniosynostosis is underestimated in the literature. J Neurosurg Pediatr. 2014 Dez;14(6):674-81.
11. Eley KA, Johson D, Wilkie AO, Javamohan J, Richards P, Wall SA. Raised intracranial pressure is frequent in untreated nonsyndromic unicoronal synostosis and dos not correlate with severity of phenotypic features. Plast Reconstr Surg. 2012 Nov;130(5):690-7.
12. Proctor MR, Rogers GF. Helmets end synostosis. J Neurosurg Pediatr. 2012;9:680-1.
13. Jimenez DF, Barone CM. Endoscopic techniques for craniosynostosis. Atlas Oral Maxillofac Surg Clin North Am. 2010 Set;18(2):93-107.
14. Lauritzen CGK, Davis C, Ivarsson A, Sanger C, Hewitt TD. The evolving role of springs in craniofacial surgery: the first 100 clinical cases. Plast Reconstr Surg. 2008 Fev;121(2):545-54.
15. Kerry AM, James CL, Mark MS, Neil AF, Jeffrey AA. Twenty-year outcome experience with open craniosynostosis repair: an analysis of reoperation and complicantion rates. Ann Plast Surg. 2018 Abr;80(4Supl 4):S158-S63.
16. Ministério da Saúde (BR). Secretaria de Atenção à Saúde. Departamento de Ações Programáticas Estratégicas. Manual para uso da caderneta de saúde da criança [Internet]. Brasília (DF): Ministério da Saúde; 2005; Acesso em 17 de julho de 2020. Disponível em: http://bvsms.saude.gov.br/bvs/publicacoes/caderneta_saude_cri anca_menino.pdf
17. Wes AM, Naran S, Sun J, Mazzaferro D, Xu W, Nguyen P, et al. The Whitaker classification of craniosynostosis outcomes: an assessment of interrater reliability. Plast Reconstr Surg. 2017 Out;140(4):579e-86e. DOI: https://doi.org/10.1097/PRS.0000000000003688
18. Czerwinski M, Hopper RA, Gruss J, Fearon JA. Major morbidity and mortality rates in craniofacial surgery: an analysis of 8101 major procedures. Plast Reconstr Surg. 2010 Jul;126(1):181-6.
19. Goobie SM, Haas T. Bleeding management for pediatric craniotomies and craniofacial surgery; Paediatr Anaesth. 2014 Jul;24(7):678-89.
20. Brockel MA, Polaner DM, Vemulakonda VM. Anesthesia in the Pediatric Patient. Urol Clin North Am. 2018 Nov;45(4):551-60. DOI: https://doi.org/10.1016/j.ucl.2018.06.003
21. Alperovich M, Vyas RM, Staffenberg DA. Is craniosynostosis repair keeping up with the times? Results from the largest national survey on craniosynostosis. J Craniofac Surg. 2015 Set;26(6):1909-13.
22. Seruya M, Oh AK, Boyajian MJ, Posnick JC, Myseros JS, Yaun AL, et al. Long-term outcomes of primary craniofacial reconstruction for craniosynostosis: a 12-year experience. Plast Reconstr Surg. 2011 Jun;127(6):2397-406.
23. Ferreira MP, Collares MV, Ferreira NP, Kraemer JL, Pereira Filho AA, Pereira Filho GA. Early surgical treatment of nonsyndromic craniosynostosis. Surg Neurol. 2006 Fev;65(Supl 1):S22-S6. DOI: https://doi.org/10.1016/j.surneu.2005.11.038
24. Chan JW, Stewart CL, Stalder MW, Hilaire HS, McBride L, Moses MH. Endoscope-assisted versus open repair of craniosynostosis: a comparison of perioperative cost and risk. J Craniofac Surg. 2013 Jan;24(1):170-4.
25. Pearson GD, Havlik RJ, Eppley B, Nykiel M, Sadove AM. Craniosynostosis: a single institution's outcome assessment from surgical reconstruction. J Craniofac Surg. 2008 Jan;19(1):65-71.
26. Natghian H, Song M, Wall S, Johnson D. Review of the use of stainless wires in craniosynostosis surgery. J Craniofac Surg. 2019 Mar/Abr;30(2):550-3. DOI: https://doi.org/10.1097/SCS.0000000000005156
27. Neligan PC. Plastic surgery - Volume 3: Craniofacial, head and neck surgery and pediatriac plastic surgery. 4th ed. New York: Elsevier; 2017.
28. Faberowski LW, Black S, Mickle JP. Blood loss and transfusion practice in the perioperative management of craniosynostosis repair. J Neurosurg Anesthesiol. 1999 Jul;11(3):167-72.
29. Eaton AC, Marsh JL, Pilgram TK. Transfusion requirements for craniosynostosis surgery in infants. Plast Reconstr Surg. 1995 Fev;95(2):277-83.
30. Birgfeld CB, Dufton L, Naumann H, Hopper RA, Gruss JS, Haberkern CM, et al. Safety of open cranial vault surgery for single-suture craniosynostosis: a case for the multidisciplinary team. J Craniofac Surg. 2015;26(7):2052-8.
31. Esparza J, Hinojosa J. Complications in the surgical treatment of craniosynostosis and craniofacial syndromes: apropos of 306 transcranial procedures. Childs Nerv Syst. 2008 Set;24(12):1421-30. DOI: https://doi.org/10.1007/s00381-008-0691-8
32. Guo Z, Ding M, Mu X, Chen R. Operative treatment of coronal craniosynostosis: 20 years of experience. Surg Neurol. 2007 Dez;68(Supl 2):S18-S21. DOI: https://doi.org/10.1016/j.surneu.2006.07.009
33. Eckelt U, Nitsche M, Müller A, Pilling E, Pinzer T, Roesner D. Ultrasound aided pin fixation of biodegradable osteosynthetic materials in cranioplasty for infants with craniosynostosis. J Craniomaxillofac Surg. 2007 Jul;35(4-5):218-21.
34. Kljajic M, Maltese G, Tarnow P, Sand P, Ko¨lby L. The cognitive profile of children with nonsyndromic craniosynostosis. Plast Reconstr Surg. 2019 Mai;143(5):1037e-52e.
35. Coelho G, Rabelo NN, Adani LB, Cecilio-Fernandes D, Carvalho FRS, Pinto FG, et al. The craniosynostosis puzzle: new simulation model for neurosurgical training. World Neurosurg. 2020 Jun;138:e299-e304. DOI: https://doi.org/10.1016/j.wneu.2020.02.098
36. Naran S, Miller M, Shakir S, Ware B, Camison L, Ford M, et al. Nonsyndromic craniosynostosis and associated abnormal speech and language development. Plast Reconstr Surg. 2017 Jul;140(1):62e-9e. DOI: https://doi.org/10.1097/PRS.0000000000003423
1. Paulista State University, Botucatu School of Medicine, Botucatu, SP, Brazil.
PVCC Analysis and/or data interpretation, Conception and design study, Data Curation, Methodology, Project Administration
MSS Analysis and/or data interpretation, Conception and design study, Data Curation, Methodology, Writing - Original Draft Preparation
LCPP Analysis and/or data interpretation, Data Curation
Corresponding author: Murilo Sgarbi Secanho, Avenida Professor Mário Rubens Guimarães Montenegro, Unesp Campus de Botucatu, Botucatu, SP, Brazil. Zip Code: 18618-687. E-mail: murilosecanho@gmail.com
Article received: April 30, 2020.
Article accepted: July 23, 2020.
Conflicts of interest: none














 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter