

Original Article - Year 2021 - Volume 36 -
Reconstruction after bipalpebral resection with preservation of the eyeball: aesthetic and functional challenge
Reconstrução após ressecção bipalpebral com preservação do globo ocular: desafio estético e funcional
ABSTRACT
Introduction: Eyelid reconstruction can be performed by primary closure, a graft of different lamellae, and local and/or regional flaps, single or combined. This reconstruction becomes more complex when the upper and lower eyelids are resected to total thickness, and the eyeball is preserved. The objective is to report the techniques used for periorbital reconstruction in bipalpebral resection cases (upper and lower) with preservation of the eyeball by the Group of Orthopalpebral Surgery of the Division of Plastic Surgery and Burns of HCFMUSP.
Methods: All cases that met the inclusion criteria from 2000 to 2019 were reviewed, and epidemiological, surgical, and postoperative follow-up data were described.
Results: Only two cases were submitted to total exeresis of the periorbital tissue and remained susceptible to eyeball preservation. Both were reconstructed with frontal flaps with complete occlusion of the eyeball at the first moment, followed by the release in stages, keeping the globe viable after reconstruction completion. Discussion: Similar reports are scarce in the literature, and, in these cases, surgical results were functionally acceptable but with significant aesthetic limitations.
Conclusion: We suggest a new option for total reconstruction of the upper and lower eyelid (with a single pedicular flap, devoid of connective graft and in multiple stages) that protects and conserves the eyeball during the various stages of surgery. The results were functionally favorable, considering the severity of the cases.
Keywords: Eyelids; Eyelid neoplasms; Eyelid diseases; Surgical flaps; Eye neoplasms.
RESUMO
Introdução: A reconstrução palpebral pode ser realizada por fechamento primário, enxerto de diferentes lamelas e retalhos locais e/ou regionais, únicos ou combinados. Essa reconstrução se torna mais complexa quando a pálpebra superior e a inferior são ressecadas em espessura total e o globo ocular é preservado. O objetivo é relatar as técnicas utilizadas para reconstrução periorbital em casos de ressecção bipalpebral (superior e inferior) com preservação do globo ocular pelo Grupo de Cirurgia Órbitopalpebral da Divisão de Cirurgia Plástica e Queimaduras do HCFMUSP.
Métodos: Foram revistos todos os casos que se encaixaram nos critérios de inclusão no período de 2000 a 2019, sendo descritos dados epidemiológicos, cirúrgicos e de seguimento pós-operatório.
Resultados: Apenas dois casos foram submetidos à exérese total do tecido periorbital e permaneceram passíveis de preservação do globo ocular. Ambos foram reconstruídos com retalhos frontais com oclusão total do globo ocular no primeiro momento, seguido pela liberação em etapas, mantendo o globo viável após a finalização da reconstrução. Discussão: São escassos os relatos semelhantes na literatura e, nestes casos, os resultados cirúrgicos se mostraram funcionalmente aceitáveis, mas com limitações estéticas importantes.
Conclusão: Sugerimos uma nova opção para a reconstrução total da pálpebra superior e inferior (com um único retalho pedicular, desprovido de enxerto conjuntivo e em múltiplos estágios) que fornece proteção e conservação do globo ocular durante as diferentes etapas da cirurgia. Os resultados foram funcionalmente favoráveis, considerando a gravidade dos casos.
Palavras-chave: Pálpebras; Neoplasias palpebrais; Doenças palpebrais; Retalhos cirúrgicos; Neoplasias oculares
INTRODUCTION
Eyelid reconstruction, after tumor resection, can be performed in different ways, from more straightforward techniques such as primary closure and full-thickness skin grafts to more elaborate and complex options, mainly local and locoregional flaps. Regardless of the technique, the most important is to perform a reconstruction that repairs the functions of all eyelid lamellae1,2.
In oncological reconstruction cases, advanced tumors generate more extensive (more than one affected subunit) and deep skin resections, requiring the combination of two or more flaps. Extensive and full-thickness eyelid resections in cases of locally advanced malignant tumors may occur with enucleation or exenteration of the eyeball due to the chance of involvement of the eyeball and/or by reconstructive difficulty, and flaps are needed that allow only the coverage of the defect created3,4.
Rare are the cases in which the resection of both eyelids’ total thickness (upper and lower, medial and lateral corner) can preserve the eyeball3,4. In these situations, it is of fundamental importance to perform immediate eyelid reconstruction, aiming primarily at maintaining their functional capacity, since chronic malocclusions can lead to recurrent keratitis, corneal ulcers, and eye loss. In the impossibility of a functional reconstruction, with satisfactory opening and occlusion, the eyeball becomes dispensable5.
The literature is scarce in the discussion of extensive eyelid resections with preservation of the eyeball that describes reparations with local flaps that allow, at the end of reconstruction, a satisfactory eyelid function6-8.
OBJECTIVE
The objective of this work is to report the experience of plastic surgeons of the Orbitopalpebral Surgery Group (Division of Plastic Surgery and Burns of the Hospital das Clínicas of the Faculty of Medicine of the University of São Paulo - HCFMUSP) in cases of total or subtotal eyelid resection (upper and lower) in total thickness with preservation of the eye globe.
METHODS
This was an observational, retrospective, and descriptive study, conducted after approval by the( )research ethics committee of USP (CAPPesq) no. 2,876,023 at the outpatient clinic of the Orbitopalpebral Surgery Group of the Division of Plastic Surgery and Burns of HCFMUSP. After tumor resection, all eyelid reconstruction cases performed from 2000 to 2019 by this group were reviewed.
Only cases of total or subtotal bipalpebral resection (upper and lower) with resection of all lamellae and consequent to benign and/or malignant neoplasms with preservation of the eyeball were included in this study.
Epidemiological, surgical, and postoperative follow-up data were collected. All photographs present were previously authorized by the patients to be published.
RESULTS
The team of arbitrary surgery of this hospital performs, on average, 1 to 2 surgeries/week of eyelid reconstruction after tumor exeresis. Among the more than 1,400 cases of operated tumors, in these 20 years, two cases of bipalpebral resection were identified and treated in total thickness with the possibility of preservation of the eyeball.
Case 1
A 54-year-old female patient presented ulcerated lesion in the upper and lower right eyelid region, medial corner, glabella region, and nasal root, as well as scar areas with tumor activity in the periphery in the left lower eyelid and nasal dorsum, whose biopsy was shown to be sclerodermiform basal cell carcinoma.
Complete resection of the lesion in monobloc with intraoperative freezing was performed, resulting in an extensive defect of the entire upper and lower eyelid region, including lateral and medial corner, glabella, and 2/3 upper nose, keeping the eyeball intact.
For coverage of the entire bloody area, a temporofrontal cutaneous flap with lateral pedicle to the right was used, based on the superficial temporal artery and concomitant grafting of the donor area with partial-thickness skin. This flap was positioned with its bloody area directly on the eyeball, occluding the entire anterior face of the eyeball, as well as the neighboring regions (Figure 1).

After four weeks, the patient evolved with bulging over the eye by tear retention, which temporarily functioned as a tissue expander and was punctured. This process was mentioned in other studies 6, which proposed maintaining small eyelid drainage opening in a medial corner for its prevention5.
After four weeks, in a 2nd surgical time, the flap was repositioned in the donor area previously grafted, keeping its deep part intact above the eyeball. Thus, it resulted in a bloody area in the glabella, 2/3 upper nose, and orbital region. Glabella, nasal dorsum and 1/3 middle of the left face were submitted to new skin grafting, and the orbital region covered by a flap of transposition of face, bipartite, and sutured to the neoconjunctiva developed naturally (Figure 2). It is noteworthy that, after the transverse opening of the thin layer on the eye, it was found that it remained viable and without corneal ulceration (Figure 2). The flap’s inner face acquired a macroscopic aspect identical to the normal conjunctiva, and later preservation of normal visual function was observed.
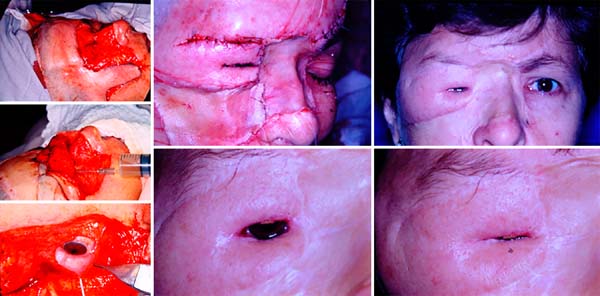
After three months, the patient was able to perform only partial occlusion movements. On this occasion, the surgery proposed by Gilles was performed with temporal fascia to improve eyelid closure. The eyelid opening was obtained after another three months, through a frontal suspension, with silicone eyelid suspension, thus ensuring a greater field of view. The flap was also indicated, but the patient refused to undergo the procedure. She was followed for two years in the outpatient clinic without complications of surgery.
Case 2
An 80-year-old female patient presented recurrence of basal cell carcinoma operated for seven years, showing hyperemia lesion, nodulations, telangiectasias, and pearly edges, which affect 2/3 of the upper eyelid and the entirety of the lower right, medial corner, and part of the lateral corner. Besides, he also had scars from multiple previous surgeries with basal cell carcinoma recurrences.
Complete resection of the lesion was performed, with free surgical margins after an intraoperative freezing examination. The resulting defect consisted of the total absence of medial and lateral corner, lower eyelid, and 80% of the upper eyelid. In this case, there was also no need for enucleation or exenteration.
The reconstructive option that would allow immediate eyeball protection and partial restoration of eyelid function in the future was the midfrontal flap, which was planned for reconstruction in 4 surgical times:
First time: demarcation was performed, the midfrontal flap was surveyed based on the left supratroclear artery (with thinner thickness in the 2/3 distal) and transposition of the same on the defect created. Only 20% of the upper eyelid in its lateral part was spared. Thus, the flap was sutured to the residual upper eyelid and periorbital region, completely covering the eyeball without any conjunctival lining. The donor area was recovered at the expense of partially thick skin grafts (Figure 3).

Second time: performed after 21 days, consisting of the pedicle section at the level of the medial corner, returning part of it to the donor area. The flap’s medial edge, already separated from the pedicle, was sutured to the defect’s medial face (Figure 4).
Third time: after 21 days, the patient underwent a new procedure, which consisted of partially incising the flap already autonomized, recreating the palpebral cleft. After 21 days, the patient underwent a new procedure, which consisted of partially incising the flap already autonomous, recreating the eyelid cleft. The intact eyeball and neoformed conjunctiva were identified on the flap’s internal face in contact with the globe (Figure 4). There was a process of neoformation of conjunctival tissue over subcutaneous cellular tissue, similar to cartilage grafting, as seen in some studies9,10.
Fourth time: after three weeks, flap slimming and auricular scathing cartilage grafting on the upper and lower eyelid scans were performed, aiming at aesthetic and functional improvement (Figure 4). The patient evolved with good eyelid opening and closure at the expense of the remnant of the upper eyelid lifter muscle (Figure 5).
DISCUSSION
Full-thickness uni-eyelid defects can be treated with excellent aesthetic and functional results through the use of local flaps, including the use of contralateral eyelid tissue7. On the other hand, full-thickness bipalpebral defects are challenging for the reconstructive surgeon due to the area’s size to be reconstructed and the scarcity of adjacent tissue sufficient to cover it, mainly when previous surgeries have already been performed on site5,7. Situations in which all or most of the orbital region is resected and the eyeball is preserved are rare, usually secondary to tumor burns, traumas, or excisions5.
The primary goal of reconstruction is to protect and maintain eye function since chronic exposure can lead to recurrent keratitis, corneal ulcer, and, eventually, even blindness. Thus, reconstructive procedures should be used to obtain occlusion and eyeball protection immediately after the eyelid lesion. On the other hand, restoring eyelid functionality with sufficient mobility, allowing opening and eyelid occlusion within each case’s limitation, is fundamental. Facial symmetry and social reintegration are important objectives but not always achieved1,2,11.
There are few options described in the literature for this complex reconstruction, but they are usually based on individual reconstructions of the anterior and posterior lamella5. This article describes their total thickness bipalpebral reconstruction experience with regional flaps, associating auricular cartilage grafting in the 2nd case. With the proposed surgery, the procedure’s technical difficulty is reduced, and donor areas of conjunctiva graft are spared, without prejudice to the eyeball. With the direct coverage of the flap’s eye, the process of neoformation of connective tissue occurs on the subcutaneous cellular tissue and acquires a conjunctival aspect11,12.
In addition to the advantages mentioned, the final result has a lower total thickness, although it is still necessary to lose weight to improve eyelid mobility. Another factor contributing to the maintenance of eyelid function, available only in case 2, is the remnant of the upper eyelid liftmuscle7. In some cases, resection of the eyelid tissue is almost complete. However, when still partially present, the upper eyelid lift muscle can guarantee upper eyelid functionality, as seen in case 2.
Total reconstruction in the upper and lower eyelids using a frontal flap of varied characteristics usually leaves the reconstructed area with significant thickness and stiffness. Eyelid movement is extremely restricted due to subtotal or total resection of the lifter, and occlusion is compromised by complete resection of the orbicularis muscle. The literature suggests a tendency of thick, rigid, and immobile eyelids after the new eyelid cleft5, but such aspects were not observed in the reported cases.
In total eyelid reconstructions using a frontal, frontotemporal flap or “masquerade graft” technique, it is always imperative to maintain a 3mm orifice for lacrimal drainage avoiding tear accumulation or cysts that can generate infectious processes. This opening, usually in the nasal corner, is also essential for irrigation and mechanical cleaning of the eyes in this surgical phase10,13. However, in the cases presented, we could keep the globe occluded, and the tear accumulation served as protection for the eyeball.
Concerning the definition of the new eyelid cleft position, it should be programmed with an awake patient and in orthostasis7. Reconstitution of the palpebral cleft late does not cause any structural damage to the eyeball, only temporary obstruction of vision. One of the most significant advantages observed in using a single flap, as in the cases described, is occlusion and protection of the eyeball while the flap autonomization occurs. The literature cases that report reconstruction with independent flaps for the upper and lower eyelid present a higher rate of keratopathies by corneal exposure5.
CONCLUSION
After bipalpebral resection with preservation of the eyeball, we suggest a new reconstruction option based on a single flap and the neoformation of connective tissue, providing protection and conservation of the eyeball during the different surgery stages. The results were functionally favorable, considering the severity of the cases.
REFERENCES
1. Mustardé JC. Reconstruction of eyelids. Ann Plast Surg. 1983;11:149-69.
2. Codner MA, McCord CD, Mejia JD, Lalonde D. Upper and lower eyelid reconstruction. Plast Reconstr Surg. 2010 Nov;126(5):231e-45e. DOI: https://doi.org/10.1097/PRS.0b013e3181eff70e
3. Alghoul M, Pacella SJ, McClellan WT, Codner MA. Eyelid reconstruction. Plast Reconstr Surg. 2013 Ago;132(2):288e-302e. DOI: https://doi.org/10.1097/PRS.0b013e3182958e6b
4. DiFrancesco LM, Codner MA, McCord CD. Upper eyelid reconstruction. Plast Reconstr Surg. 2004 Dez;114(7):98e-107e. DOI: https://doi.org/10.1097/01.PRS.0000142743.57711.48
5. Sousa JL, Leibovitch I, Malhotra R, O'Donnell B, Sullivan R, Selva D. Techniques and outcomes of total upper and lower eyelid reconstruction. Arch Ophthalmol. 2007 Dez;125(12):1601-9.
6. Badilla J, González-Arias S. Scalping forehead transposition flap for total eyelid reconstruction with periocular involvement associated with a conjunctival cyst formation. Int J Orbital Disord Oculoplastic Lacrimal Surg. 2014;33(3):206-9. DOI: https://doi.org/10.3109/01676830.2013.859278
7. Bertrand B, Colson Junior TR, Baptista C, Georgiou C, Philandrianos C, Degardin N, et al. Total upper and lower eyelid reconstruction: a rare procedure-a report of two cases. Plast Reconstr Surg. 2015 Out;136(4):855-9. DOI: https://doi.org/10.1097/PRS.0000000000001600
8. Lalonde DH, Osei-Tutu KB. Functional reconstruction of unilateral, subtotal, full-thickness upper and lower eyelid defects with a single hard palate graft covered with advancement orbicularis myocutaneous flaps. Plast Reconstr Surg. 2005 Mai;115(6):1696-700. DOI: https://doi.org/10.1097/01.PRS.0000161455.07552.48
9. Converse JC, Smith B. Repair of severe burn ectropion of the eyelid. Plast Reconstr Surg Transplant Bull. 1959 Jan;23(1):21-6.
10. Snyder GB, Edgerton MT. Masquerade graft technique for simultaneous reconstruction of the upper and lower lids in patients with blastomicosis, amyloidosis or other chronic septic destructive lesions. Plast Reconstr Surg. 1964 Ago;34:163-8.
11. Friedhofer H, Salles AG, Jucá MCCR, Ferreira MC. Eyelid reconstruction using cartilage grafts from auricular scapha. Eur J Plast Surg. 1999;22(2-3):96-101.
12. Nigro MVAS, Friedhofer H, Natalino RJM, Ferreira MC. Comparative analysis of the influence of perichondrium on conjunctival epithelialization on conchal cartilage grafts in eyelid reconstruction: experimental study in rabbits. Plast Reconstr Surg. 2009 Jan;123(1):55-63. DOI: https://doi.org/10.1097/PRS.0b013e3181904b6d
13. O'Reilly P, Malhotra R. Our experience with the masquerade procedure for total eyelid loss. Orbit. 2010 Dez;29(6):1313-6.
1. Hospital das Clínicas, Faculty of Medicine,
University of São Paulo, Department of Plastic Surgery and Burns, São Paulo,
SP,
Brazil.
2. Private Practice, Plastic Surgery, São Paulo,
SP, Brazil.
Institution: Hospital das Clínicas, Faculty of Medicine, University of São Paulo, São Paulo, SP, Brazil.
HF Conception and design study, Conceptualization, Final manuscript approval, Realization of operations and/or trials, Supervision
RCL Analysis and/or data interpretation, Conception and design study, Data Curation, Methodology, Realization of operations and/or trials, Writing - Original Draft Preparation
AHV Analysis and/or data interpretation, Final manuscript approval, Realization of operations and/or trials, Writing - Review & Editing
MBS Methodology, Project Administration, Realization of operations and/or trials, Writing - Review & Editing
MNSJ Methodology, Project Administration, Realization of operations and/or trials, Writing - Review & Editing
JFGUMR Methodology, Realization of operations and/or trials, Writing - Original Draft Preparation
JYT Realization of operations and/or trials
RG Conceptualization, Final manuscript approval, Writing - Review & Editing
*Corresponding author: Rodolfo Costa Lobato Rua Melo Alves, 55, Conjunto 23, Cerqueira César, São Paulo, SP, Brazil. Zip Code: 01417-010 E-mail: rodolfolobato49@yahoo.com.br
Article received: July 06, 2020.
Article accepted: July 23, 2020.
Conflicts of interest: none










 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter