

Articles - Year 1997 - Volume 12 -
Posterior Intercostal Flap: Anatomical Considerations
Retalho Intercostal Posterior: Considerações Anatômicas
ABSTRACT
The author developed an anatomical study of the Posterior Intercostal Flap, by two series of fresh cadavers dissections in a range from T8 to T11. In the first series, intercostal arteries dye injections were performed in seven specimens in order to determine the coloured area. Second series consisted of twenty dissections that aimed the separation of artery, veins of each intercostal space reporting the distance between their major emerging branches as well as the rotation arches. One clinical application of the flap is presented for correction of pressure sore in a paraplegic patient. The author concluded about the safety of the procedure emphasizing the possibility of restoring sensibility to pressure areas in paraplegics, wich is very important to decrease the high recurrence ratio in those cases.
Keywords: Posterior intercostal flap, pressure sores, paraplegics
RESUMO
O autor fez um estudo anatômico em cadáveres frescos do retalho intercostal posterior de T8 a T11. No primeiro grupo, utilizou sete cadáveres para injetar corante nas artérias intercostais posteriores e determinar a área corada demarcada. No segundo grupo, dissecou vinte cadáveres, isolando a artéria, veia e nervo intercostais de cada espaço, anotando as distâncias de emergência de seus principais ramos e arco de rotação. Em seguida, relatou aplicação clínica em um caso de úlcera de pressão por paraplegia. Concluiu, por fim, que este retalho, além de muito seguro, garante sensibilidade às áreas de pressão em paraplégicos, sendo de grande utilidade para diminuir o alto índice de recidivas nestes casos.
Palavras-chave: Retalho intercostal posterior, úlceras de pressão, paraplégicos
In 1974, Dibbel(4) reported the first clinical case of application of a posterior intercostal flap (PIF) for the closure of sacral ulcers in a two and a half year old child, with secondary paraplegy because of myelomeningocele. It is known that paraplegic patients frequently develop pressure ulcers in several regions, mainly in those of the sacrum, trochanter and ischium. Such pathology requires correction through a series of surgical procedures that, however do not address the basic cause, meaning the insensibility of the affected regions, causing a high rate of recurrences and a series of subsequent surgeries, increasingly difficult to perform. Keeping the same reasons in mind, lesions of the finger tip and calcaneus are not satisfactorily solved with denervated flaps(4).
Intercostal spaces are excellent sources of innervated flaps as a result of the constant anatomy, vicinity of the neurovascular structures (which remain united in all the corresponding metamere) and by the potential large arch of rotation.
Furthermore, there are various intercostal spaces on each side, warranting that in one single patient, a series of flaps may, theoretically be elevated. This is useful when, because of scars, ulcers or radiodermatitis, certain regions cannot be used or there is a series of pressure ulcers.
Since 1976, Daniel(2,3,7) published some papers on the anatomical study of cadavers, showing the application of PIF in some clinical cases, standardizing the surgical procedure.
Although other authors(1,5,7,9,10,11) have also reported their experiments, use of PIF remains quite restricted and still requires further studies that confirm its advantages. The objective of this paper is the anatomical study of PIF, undertaken in fresh cadavers, and its application to a clinical case.
MATERIAL AND METHODS
Anatomical dissections were performed on 27 fresh cadavers ar the Morgue of the São Paulo Capital City (Serviço de Verificação de Óbitos da Capital - S.V.O.C).
Cadavers with abdominal scars liable to interfere with the results of the study were excluded.
Cadavers were divided into two groups:
Group I
The first group comprised 7 fresh cadavers, 5 males and 2 females, average age 52.57 years, 71.42% of Caucasian, 28.57% of Mulattoes, average weight 68 kg and average height 172.28 cm (Table I). The intercostal arteries of the eighth, ninth, tenth and eleventh intercostal spaces were approached (T8, T9, T1O and T11) by longitudinal incision of the skin along the paravertebral line (lateral costal transverse ligament), encompassing the mentioned spaces. In both the cranial and caudal direction the incision was extended perpendicular to the lateral direction, and then a skin and subcutaneous tissue flap were folded back disclosing the paraspineal muscles and the median border of the latissimus dorsi muscle. The latter was laterally folded back by means of a rhombus dissection, thus reaching the costal fold. Then, the intercostal muscles were divulsed, exposing the nervous-vascular bundle. At this point, a #27G Jelco® catheter, was introduced in the artery and a vital stain was injected (Methilene blue) to trace the irrigated cutaneous area (Table 3).
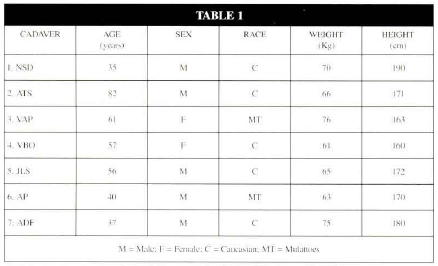
Table 1. Group 1 - Physical aspects of the dissecated cadavers.
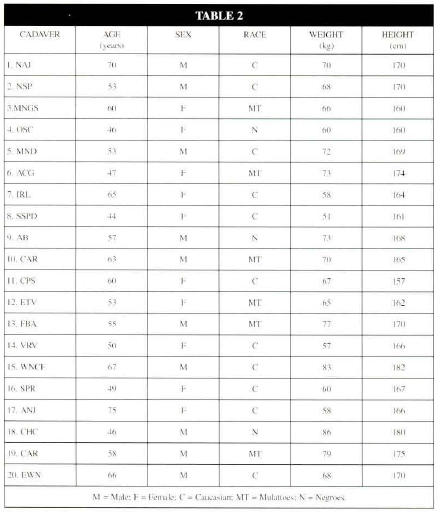
Table 2. Group 2 - Physical aspects of the dissecated cadavers.
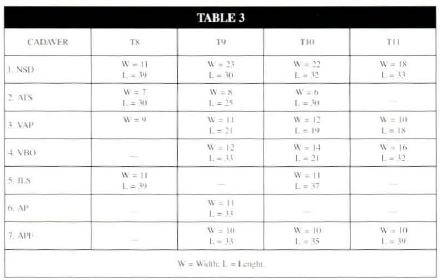
Table 3. Dimensions - in centimeters - of the irrigated cutaneous territory.
The length (of the paravertebral line to the more anterior point of the stained area) was marked as well as the width (the largest measure of stained skin perpendicular to the greatest axis) of the stained skin area for each artery (Table 3). The distances of the stained region to abdominal points: hemiclavicular line, xiphoid appendix, ipsilateral costal fold, ipsilateral upper anterior iliac crest and the umbilical scar (Figure 1 and Table 4) were also measured.
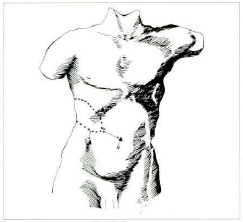
Fig. 1. Distances between stained area (dotted area) and anatomical references.

Table 4. Smaller distances - in centimeters - from the stained area to anatomical points.
In some arteries, in order to avoid overlapping of the stained areas, a red stain of acrylic paint was injected or the contralateral artery was used.
Group 11
For the second group 20 cadavers were selected: ten males and 10 females, average age of 56.85 years, average weight 68.5 kg. 55% were Caucasian, 30% Mulattoes and 15% Negroes (Table 2).
A longitudinal incision was performed on the paravertebral line, similar to that of the first group, extended laterally by horizontal incision somewhat under the eleventh rib. This incision was enlarged when the nervousvascular bundles from T11 to T8 were detached.
The intercostal muscles were incised until the neurovascular pedicle became apparent, next to the costal groove. The separation of the pedicle was undertaken, identifying its main branches and anatomical relations. Measures of the rotation arch (frorn the paravertebral line to the lateral margin of the rectus abdominalis muscle) were marked down as well as the main branches with regard to the paravertebral lines (Tables 5 and 6).
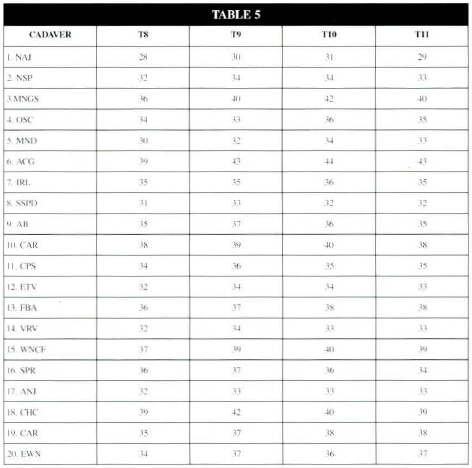
Table 5. Anatomical study of the distances - in centimeters from the lenght of the intercostal pedicle of the lateral margin of the rectus abdominalis muscle.
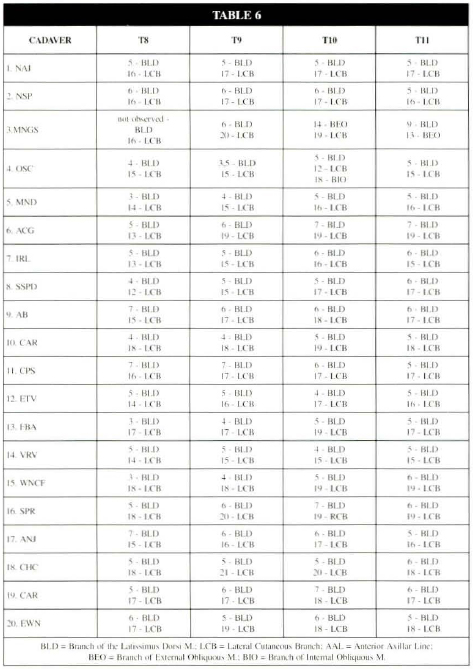
Table 6. Anatomical study of the distances - in centimeters - of the origin of the main branches of the posterior intercostal artery starting from the paravertebral line.
RESULTS
Group I
As presented in Table 3, a large cutaneous territory irrigated by the artery of each intercostal space was found.
In T8, the area corresponds to the limits beginning in the paravertebral region and going somewhat beyond the anterior middle line, encompassing the region of the nipple and the epigastric region, with an average lenght of 32.5 cm and an average width of 9.5 cm.
In T9, it goes from the paravertebral region to 2 cm before the anterior middle line, encompassing the epigastrium and mesogastrium region, with an average lenght of 29.16 cm and an average width of 12.5 cm.
In T1O the stained area largely overlaps the area of T9 with an addition in the lower direction, towards the hypogastrium region. It exhibits an average length of 29 cm and an average width of 12.5 cm. Both T1O and T9 represent the largest stained areas (approximatelly four intercostal spaces).
In T11 the irrigated area goes from the paravertebral region to 5 cm before the anterior middle line, exhibiting a visibly more oblique and lower axis, reaching the hypogastrium region and the upper-anterior iliac crest (Photo 1 and 2). It has an average lenght of 30.5 cm and an average width of 13.5 cm.
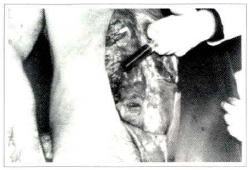
Photo 1. Dye injection into the artery.
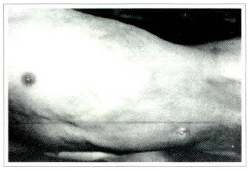
Photo 2. Stained area at T10.
Some variations in the pattern of the stained areas were observed.
In some cadavers, such areas did not reach the middle line, remaining at the level of the lateral border of the rectus abdominalis muscle. In others, there was a space between the non-stained area at level of the lateral border of the rectus abdominis muscle.
Group II
The posterior intercostal artery of each intercostal space exhibits a similar anatomy, only its overall length changes. In the cadavers, artery and vein have similar diameters of approximately 1.5 mm. The nerve exhibits a diameter of 3 mm, with 3 or 4 small bundles. The entire pedicle follows jointly, obeying in the cranial-caudal direction to the orientation of vein, artery and nerve. The unit progresses along the costal groove, below the internal and external intercostal muscles and above the intimus intercostal muscle. After exiting the costal groove, it proceeds a short way below the costal cartilage and, beyond that, it passes above the transverse muscle and below the internal obliquous until it reaches the posterior sheath of the rectus abdominalis muscle, perforating it and acquiring an inframuscular position. Thereupon, within the muscles intima, it forms an anastomosis with the deep epigastrium system. A gradual reduction of the structure's diameter is perceived as they proceed towards the anterior side. In the muscle portion after, leaving the costal grid, the pedicle takes over the form of a plexus, although it maintains the interrelation among structures.
Along the way, vessels constitute a variety of branches towards the adjacent muscle groups, ribs and subcutaneous. The most important being the lateral cutaneous branch that starts at the level of the posterior axillar line, crossing the internal and external obliquous muscles and, already in the subcutaneous, bifurcates in a posterior branch usually small and anterior longer and of a larger gauge and long. In some cadavers such bifurcation takes place within the fibers of the external obliquous. A constant branch for the latissimus dorsi was also found in all the dissected spaces (Figure 2).
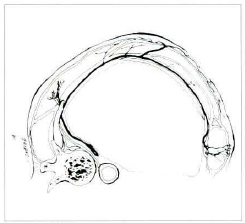
Fig. 2. Pedicle direction from its origin to the anastomotic area with the epigastric system.
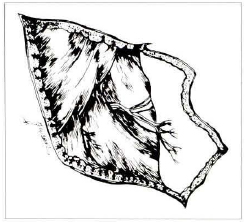
Fig. 3. Lateral cutaneous branch exiting between the latissimus dorsi and external obliquous muscles.
The median length of the pedicle was 34.25 cm in T8, 36.1 cm in T9, 36.4 cm in T1O and 35.6 cm in T11 (Table 5).
All pedicles of each space presented constant branches and with similar distances. For the latissimus dorsi muscle, the first branch arises at approximately 5 cm of the paravertebral line. The lateral cutaneous branch of the intercostal artery arises approximately between 15 and 17 cm of the paravertebral line.

Photo 3. Dissected pedicle. Notice the lateral cutaneous branches.
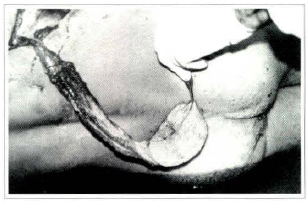
Photo 4. Dissected flap and rotation arch.
As an average, the branch for the latissimus dorsi muscle (BLD) and the lateral cutaneous branch (LCB) arise, respectively, at 5 and 15.85 cm in T8; 5.17 and 17.2 cm in T9; 5.47 and 17.45 cm in T10 and 5.65 and 17 cm in T11 (see Table 6).
In T9, T10 and T11 approximately at 17 cm, arises the branch that crosses the external obliquous muscle oriented towards the subcutaneous (lateral cutaneous branch - LCB). In T10 at 18 cm, arises a branch for the internal obliquous muscle.
CLINICAL CASE
Patient E.S.B., 26 years old, presenting paraplegia and a neurogenic urinary bladder for the last 15 months as a result of a firearm shot in the lumbar region wich a rachimedullar lesion at the T12-S1 transition level, presenting decubitus ulcers of about 8 x 6 cm in the sacrococcigeal regions, of 6 x 4 cm in the right trochanteric and of 2 x 2 cm in the left ischiatic regions. The patient had retained cutancous sensitivity at T10 level and exibited a good clinical and nutritional picture, being thus selected for surgery.
It was planned not to repair all the ulcers at the same surgical time, to permit changes of the decubitus in the postoperative period. Thus, the sacrococcigeal ulcer was chosen, as it was the largest.
Surgical Procedure
Patient under general anesthesia positioned for thoracostomy. Tracing of the skin flap in the periumbilical region measuring approximately 9 x 7 cm was performed along the path of the tenth intercostal space (T10). The skin was cut along the pathway of the tenth rib, detaching the subcutaneous from the subjacent, superficial fascia of the external obliquous muscle, thus exposing the entire tenth intercostal space, from the upper margin of the upper rib until the lower margin of the inferior rib. The latissimus dorsi muscle, in the vicinity of the posterior axillar line was partially incised and folded back to facilitate dissection of the T10 pedicle. Next, the external obliquous muscle was incised on the cranial margin of the tenth rib, folding it back and exposing its periosteum that was detached at the time when the internal and external intercostal muscles were disinserted. At umbilical level the skin of the flap was incised until the opening of the anterior sheath of the rectus abdominis muscle, dissecting the deep epigastrium vessels and making a ligature with 2-0 cotton sutures, after the section of the cranial and caudal portion of the rectus abdominis muscle which was inclued in the flap. With careful dissection at level of the linea alba, the miocutaneous flap was released, and from there proceeding in dorsal direction on the upper margin of the eleventh rib, freeing and elevating together the intercostal muscles and the nervous vascular bundle; the not important collateral branches were ligated with 4-0 cotton sutures. The flap was elevated, encopassing parts of the external and internal obliquous muscles and the internal and external intercostal muscles, leaving intact the transversus muscle, the intimus intercostal muscle and the pleura. The external and internal obliquous muscles found between the tenth and eleventh ribs were elevated together with the pedicle, 3 cm after the posterior axillar line to maintain the lateral cutaneous branch of the intercostal artery. A revival of the ulcer's margins and building of a subcutaneous tunnel to allow the passage of the flap until the receptor area. Final hemostasis was been performed with a bipolar cauterizing and a continuous aspiration drain has been set in place along the pathway of T10 and under the flap. The defect on the donating area at level of the umbilical scar has been repaired by approximation and primary suture. Margins of the latissimus dorsi muscle were sutured using Vicryl 2-0 and 'U' stitches. The donating and receptor areas were closed with Nylon 4-0 suture. The continuous aspiration drain was withdrawn on the 5th day.
At immediate and delayed post-operatory period the flap presented very good perfusion, with immediate re-perfusion after compression, with no changes in color (cyanosis or pallor). Patient presented sensitivity to touch and pain soon after surgery, locating the stimulus in the periumbilical region (Photos 5 to 9). After two weeks, the flap did not present any changes in perfusion, with a 100% vitality (Photo 10).

Photo 5. Pre-operatory
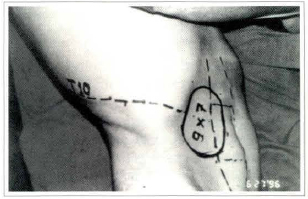
Photo 6. Flap drawing. Pre-operatory
Photo 7. Intra-operatory Isolated flap

Photo 8. Intra-operatory. Donating area.
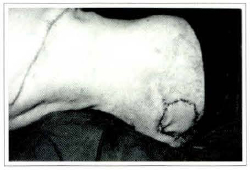
Photo 9. Immediate post-operatory.
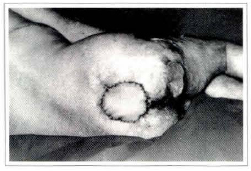
Photo 10. Five days post-operatory.
DISCUSSION
The PIF utilized for the management of pressure ulcers has proven itself quite risk free from the blood nutrition point of view. This is because the intercostal artery is segmental, that is, a primary branch of the aorta with high flow pressure. Besides various cutaneous branches it anastomoses with the deep vessels of the epigastrium to the rectus abdominis muscle that holds muscle cutaneous perforans in the periumbilical region. Furthermore, each intercostal space on each side is a source for a flap.
Innervation of the flap has also proven to be highly constant. The nerve, the artery and the vein are alwavs joined and present along the whole path of the intercostal space.
Dibbel(4), in 1974, was the first one to use the posterior intercostal flap in a clinical case, having performed the surgery in four steps. First he identified the pedicle and incised the flap in its upper and lower portions. At the second step he incised all the flap. On the third one, he elevated the flap with the pedicle and sutured it on the donating region. In the last stage, he once more elevated the flap, revived the margins of the ulcer and, by means of a subcutaneous tunnel, took it to its recipient bed.
Dibbel questioned whether the flap could reach regions such as the sacrococcigeal and trochanteric ones. Daniel and collaborators(2,3,7), in 1980, undertook an anatomical study between T7 and T12 and reported the results in clinical cases submitted to surgery. In some cases, surgery was performed in two stages and in others in one stage. They further reported reconstruction of the contralateral thoracic wall, e1evating the rib together with the flap; free transfer of flap for treatment of pressure ulcer in paraplegic with grafting of the sural nerve (previous biopsy of the sural nerve was performed).
Shively and collaborators(11) in 1981, described an increase of the sensitivity area beyond the flap area, which had not been observed by Dibbel.
Little and collaborators(8), in 1981, proposed a modification of the flap e1evation technique, designating it as upper quadrant flap. They elevated all the intercostal space, including the parietal pleura, the rib's periosteum, the abdominal transversus muscle and the posterior sheath of the rectus abdominis muscle. Furthermore, they performed resection of a segment of rib of the corresponding space. The elevated skin on the flap might be extended to the contralateral region and to the lower abdomen. With these modifications, Little and collaborators reported reduction of the surgical time and transfer of larger cutaneous areas.
In 1982, Raynaud(10), published the utilization of the posterior intercostal flap for a case of lumbar radio-necrosis.
Bardran and collaborators(1) in 1984, performed an anatomical study stressing the anatomy of the lateral cutaneous branch and its utilization as a free flap. (The lateral cutaneous branch originates in the posterior axillar line with a cutaneous territory irrigated like the main pedicle). They reported the utilization of a free, innervated flap, with a pedicle into this branch for correction of post-burn cervical retraction, lesion of the palm and back of the hand and impairment of the calcaneous.
In 1994, Gao(5) reported the use of a flap with pedicle in the lateral cutaneous branch for two stages repair of a hand burn. In the first stage, he elevated the flap and sutured it to the back of the hand. In the second stage, he cut off the pedicle.
All authors reported the finding of the flap's sensitivity to touch, to pain and to temperature in different degrees. Complications reported by various authors, include total and partial necrosis, hematomas, pneumothorax, hyperesthesia and bone growth along the pedicle's pathway.
In our study, we showed that the pedicle in T11 was sufficiently long to reach the sacral region as well as the ischium and trochanter regions, except in the case of longilineal individuals, with a rather acute infrasternal angle.
Although Daniel and Kerrigan noticed a large cutaneous area irrigated by the lateral cutaneous branch and its bifurcation before the sheath of the rectus abdominis muscle, we include the latter in the flaps described in clinical cases, considering the periumbilical perforans, keeping in mind a greater circulatory safety.
As such, we believe, that the elevation of the flap in one stage is fairly secure and enabled us to transfer an island of skin to more distal regions, expanding its rotation arch.
In the case submitted to surgery, we found the customary thoracic drainage unnecessary, as dissection of the pedicle should not go beyond the parietal pleura.
CONCLUSIONS
The posterior intercostal flap is a muscle cutaneous flap different from the customary ones because of a series of muscles constituting its pedicle.
It exhibits important characteristics such as:
- Long, thin and pliant pedicle;
- Large rotation arch;
- Large skin surface area to be transferred;
- It is innervated;
- 1t has various potential pedicles.
Its disadvantage is the requirements of a more complex surgical procedure. In the pressure ulcers of paraplegic individuals, the posterior intercostal flap, has over other options the advantage of solving the basic cause - which would be the lack of sensitivity in these regions - and constitutes the first choice for patients in good clinical conditions and with sensitivity in the region of the donating area.
It is, futhermore, very useful in patients with multiple surgeries and large sized ulcers.
BIBLIOGRAPHY
1. BADRAN, H. A.; EL-HELALY, M. S. - Safe I: The Lateral Intercostal Neurovascular Free Flap. Plast. Reconstr. Surg., 73:1,1984.
2. DANIEL, R. K.; KERRIGAN, C. L.; GARD, D. A. - The Great Potencial of the Intercostal Flap for Torso Reconstruction. Plast. Reconstr. Surg., 61:653,1978.
3. DANIEL, R. K.; TERZIS, J. K.; CONNINGHAM, D. M. - Sensory Skin Flaps for Coverage of Pressure Sores in Paraplegics Patients: A Preliminary Report. Plast. Reconstr. Surg., 58:317,1976.
4. DIBBELL, D. G. - Use of a Long Island Flap to Bring Sensation to the Sacral Area in Young Paraplegics. Plast. Reconstr. Surg., 54:220, 1974.
5. GAO, J. H. et col- Usefulnes of Narrow Pedicled Intercostal Cutaneous Perforator Flap for Coverage of the Burned Hand. Burns 20, 1, 1994.
6. KERRIGAN, C. L.; DANIEL, R. K. - The Intercostal Flap: An Anatomical and Hemodynamic Approach. Ann. Plast. Surg., 2:411, 1979.
7. LITTLE, J. W.; FONTANA, D. J.; McCULLOCH, D. T. - The Upper-Quadrant Flap. Plast. Reconstr. Surg.,68:2, 1981.
8. Nomina Anatomica-quinta edição: Editora MEDSI, 1987.
9. RAYNAUD, J. P.; GARY-BOBO, A. - Urilizacion du Lambeau en Îlot Intercostal: A Propros d' un cas de Vaste Radionécrose Lombaire. Ann. Chir. Plast., 27:3, 1982.
10. SHIVELY, R. E.; SCHAFER, M. E.; KERNAHAN, D. A. - The Spread of Sensibility into Previously Anesthetic Skin Following Intercostal Flap Transfer in a Paraplegic. Ann. Plast. Surg., 5:5, 1980.
I - Titular Member of the Brazilian Society of Plastic Surgery, Assistent Phisician of the Instituto de Cirurgia Plástica Santa Cruz - SP.
II - Associated Member of Brazilian Society of Plastic Surgery, Fellow of the Instituto de Cirurgia Plástica Santa Cruz - SP.
III - Associated Member of Brazilian Society of Plastic Surgery.
IV - Third Year Resident Phisician in Plastic Surgery at Instituto de Cirurgia Plástica Santa Cruz - SP.
V - Titular Member of the Brazilian Society of Plastic Surgery, Director of the Instituto de Cirurgia Plástica Santa Cruz - SP.
Work performed at Instituto de Cirurgia Plástica Santa Cruz (SP) and Serviço de Verificação de Óbito da Capital (SP).
Address for Correspondence:
Jason C. A. Figueiredo, MD
Instituto de Cirurgia Plástica Santa Cruz
Rua Santa Cruz, 398
04122-000 - São Paulo - SP - Brazil


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter