

Original Article - Year 2021 - Volume 36 -
Primary augmentation mammoplasty in a plastic surgery residency service
Mastoplastia de aumento primária em serviço de residência médica de cirurgia plástica
ABSTRACT
Introduction: Primary augmentation mammoplasty is one of the main cosmetic surgeries in the plastic surgeon’s routine. The various performance techniques require constant study and extensive training of the specialty’s resident physicians.
Methods: Review medical records of patients who underwent primary augmentation mammoplasty at the Hospital das Clínicas of the Faculdade de Medicina de Botucatu from 2017 to 2020.
Results: 120 surgeries were performed during the period analyzed. There was a predominance of high-projection (75%) and subfascial (67.5%) implants. There were no major complications, with most patients (75%) not having any minor complications (p<0.001).
Conclusion: Augmentation mammoplasty is a safe surgery when performed following proper technical care and under supervision.
Keywords: Mammoplasty; Breast implant; Plastic surgery; breast implants; Internship and residency; Teaching Hospitals.
RESUMO
Introdução: A mastoplastia de aumento primária é uma das principais cirurgias estéticas na rotina do cirurgião plástico. As várias técnicas de realização exigem estudo constante e formação ampla dos médicos residentes da especialidade.
Métodos: Revisão de prontuários das pacientes submetidas a mastoplastias de aumento primária no Hospital das Clínicas da Faculdade de Medicina de Botucatu no período de 2017 a 2020.
Resultados: 120 cirurgias foram realizadas no período analisado. Houve predomínio de implantes de projeção alta (75%) e em plano subfascial (67,5%). Houve ausência de complicações maiores, com grande parte das pacientes (75%) não apresentando nenhuma complicação menor (p<0,001).
Conclusão: A mastoplastia de aumento é uma cirurgia segura quando realizada seguindo os cuidados técnicos adequados e sob supervisão, sendo um procedimento importante na formação do cirurgião plástico.
Palavras-chave: Mamoplastia; Implante mamário; Cirurgia plástica; Implantes de mama; Internato e residência; Hospitais de ensino.
INTRODUCTION
Brazil was the country that performed the most cosmetic surgeries in 2018, with 1,498,327 procedures. Leading the table, augmentation mammoplasty appears responsible for 18.4% of this total, which corresponds to 275,283 surgeries1. The need for learning this area of plastic surgery during residency is evident. Teaching this type of procedure is not limited only to the issue of insertion in the labor market. Still, there is also training in the doctor-patient relationship, evolving the ability of interpersonal communication, which is essential in the practice of the specialty2.
Reparative treatment should still be the main pillar of resident training, especially since it is normative to perform only 15% of cosmetic surgeries during specialist training3. The Unified Health System (SUS) offers several treatments involving plastic surgery, such as oncology, microsurgery, trauma, surgery after massive weight loss, treatment of lipodystrophy secondary to antiretroviral therapy. All these subspecialties are part of the training of plastic surgeons, according to the National Commission for Medical Residency guidelines in 20194.
Augmentation mammoplasty techniques are not limited exclusively to the use of breast implants. Fat grafting has gained ground, with advanced studies regarding its collection, preparation and application, in addition to being able to be performed alone or in association with silicone implants5,6.
The correct indication of techniques and even the types of implants available requires a detailed physical examination, aiming to adapt the prostheses to the anatomical structure and profile of the patients7. It is worth highlighting the importance of clinical evaluation, especially at the furcula-nipple distance between 17 and 21cm and the cutaneous envelope fold greater than 2cm, which may indicate the need for a submuscular plane8.
The literature varies concerning what is considered an adequate increase in breast size, changing between different cultures and times the ideal breast size or shape. We found some attempts on the description of the breast with the best shape and volume, but without a concrete formula7,9. The same can be said about the technique, as different authors have preferences regarding access routes - inframammary, periareolar and transaxillary -, dissection planes - subfascial, “dual plane” (submuscular) subglandular -, and types of silicone - macro and microtextured, among others8,10.
Therefore, the correct indication and knowledge of available arsenals are valuable tools for residents.
This article aims to present a survey of primary augmentation mammoplasty performed by first- and second-year plastic surgery students at the Botucatu Medical School Hospital das Clínicas in the last four years and discuss teaching this type of surgery in the scope of medical residency.
OBJECTIVES
In this article, we aim to present a survey of primary augmentation mastoplasty performed by first and second year plastic surgery students at the Hospital das Clínicas of the Faculty of Medicine of Botucatu in the last four years and discuss the teaching of this type of surgery in the scope of medical residency
METHODS
We reviewed the medical records of patients who underwent primary augmentation mammoplasty by residents of the first and second year of Plastic Surgery at the Hospital das Clínicas, Faculty of Medicine of Botucatu UNESP (HC FMB UNESP) in the last four years - the period from January 2017 to March 2020.
Outpatient routine and surgical schedule
Patients were selected who are followed up at the cosmetic plastic surgery outpatient clinic, entered via Annex I of the Unified Health System with complaints of hypomastia. All undergo screening, excluding cases of BMI greater than 28 or less than 16, in addition to smokers and collagen diseases or comorbidities that make it impossible to perform surgery under general anesthesia. After this phase, patients undergo a consultation called the “New Aesthetics Case,” where they undergo a complete anamnesis and detailed physical examination, followed by surgical planning with at least two different volumes of implants to be selected on the day of the surgery, according to the size of the pocket created and joint decision at the time of markings.
All patients are reassessed the day before or on the procedure when the surgical planning is re-discussed, and the points of reference, breast limits and incision site are marked with a dermographic pen.
After the surgeries, the patients were instructed to wear a surgical bra for at least 30 days without interruption and at least 30 days at night.
Surgical technique
In this topic, there was little variation regarding materials, using lighted retractors of different sizes, shapes and brands, and the suture threads varied between mononylon, Monocryl and polydioxanone, as well as the dressing methods, with micropore, rayon and tape adhesives. There was always a change of gloves during implantation and cleaning of them with 0.9% saline solution before handling the implant. In general, all patients were positioned on tables with dorsiflexion capacity to assess symmetry after implantation of the prostheses.
Inclusion criteria
All adult patients who underwent primary augmentation mammoplasty, strictly for aesthetic indication, performed procedures by a first- or second-year resident as the main surgeon.
Among the selected medical records, some patients underwent other procedures at the same surgical time, such as liposuction, gluteal fat grafting, rhinoplasty, abdominoplasty, papilla reduction and revision of other scars.
Exclusion Criteria
As an exclusion criterion for medical records, we did not include patients with congenital or acquired, post-bariatric thoracic deformities or the need for pexia or any form of skin resection.
Data analysis
Descriptive statistical analysis was performed, with analysis of variance to calculate the mean and standard deviation for the volume, according to the position of the implant; chi-square test to assess complications; and Goodman test to compare the profile of the implant and its position.
TCLE and CEP
Before the surgeries, all patients were submitted to sign an informed consent form, including risks inherent to the anesthetic-surgical procedure and specific to augmentation mammoplasty. The work follows the recommendations of the Research Ethics Committee (CEP) of the HC FMB UNESP, being approved under the opinion number 4,480,923.
RESULTS
Patients
One hundred twenty patients were identified in these four years (January 2017 to July 2020), with ages ranging from 19 to 47 years - a mean of 28.6 years.
The body mass index (BMI) ranged from 16.9 to 26.2 - an average of 21.73, and in 26 patients, it was not possible to calculate BMI retrogradely at the time of surgery.
Seven patients had hypothyroidism, one patient was hypertensive, and the other had congenital adrenal hyperplasia. Still, all maintained adequate clinical control during surgery and had a specialized and regular follow-up of the individual comorbidities.
Implants
| Position x Volume of implant (ml) | Subfascial | “Dual plane” (submuscular) | Subglandular | p1 |
|---|---|---|---|---|
| Average | 333,3 | 308,1 | 325,2 | 0,08 |
| SD | 36,1 | 37,9 | 44,2 |
1 Analysis of variance.
SD: standard deviation.
All surgeries performed were bilateral and had a round base as the implant of choice and shared the same manufacturer - Silimed®. Only one patient received the polyurethane type implant, and all the other prostheses were textured.
The volume of implants ranged from 270 to 445ml, with an average of 327.25ml, as shown in Table 1. The biggest difference between the right and left sides was 85ml, and in 10 cases, implants of different sizes were used.
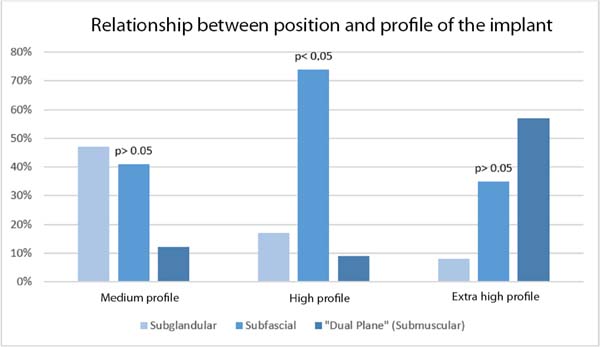
There was a predominance of high-projection implants 75% (90/120), followed by medium implants 14% (17/120) and extra-high 10.8% (13/120). No patients received low-projection implants. Figure 1 shows the distribution of these data and their relationship with the position of the implants using the Goodman test (p=0.03).
Surgical technique
The surgery time ranged from 45 to 330 minutes, with an average time of 116 minutes. Still, these values were affected by the performance of other procedures in the same surgical time. It is not possible to quantify the time spent with liposuction in some cases, for example.
The access route was invariably inframammary in the selected cases, with irregular reports regarding the quality of the scar and the need to revise it intraoperatively due to edge trauma caused by tissue manipulation during implant inclusion.
As for the implant position, 67.5% (81/120) were placed in the subfascial position, and 21.6% (26/120) were implanted in the subglandular position, mainly due to difficulty identifying separating the fascia from the pectoralis major muscle.
All patients who had implants placed with the “dual plane” (submuscular) technique, which corresponded to 10.8% (13/120), left the surgery with a portovac drain, with an average time of 2 to 7 days until removal. Drain use was irregular in the other patients, with use being reported in 15% (18/120) of cases, especially when intraoperative bleeding that was difficult to control was noted. In these cases, the drain remained for 2 to 7 days, respecting the same removal criteria: serous or serohematic appearance and a flow rate of less than 30ml in 24 hours.
Comparisons between the profile and position of the implants are shown in Figure 1.
Complications
Only one patient in the observed interval required surgical re-approach due to unnoticed asymmetry during the intraoperative period, with symmetrization being performed in a second time by the same surgeon nine months after the first surgery, without approaching the capsule or changing implants. Another patient complained of breast ptosis and underwent periareolar mastopexy one year after primary mammoplasty. No other patient required surgical re-approach until the time these results were released (January/2021).
During surgery, there was an external rupture during implantation, requiring exhaustive washing of the skin and cavity, and replacement for an implant of the same size, without other complications during the intra- and postoperative period.
We did not identify major complications, such as cases of infection, seroma or hematoma requiring surgical re-approach, as well as venous thromboembolism or death. The only case of infection appeared on the 8th postoperative day and was treated conservatively, with observation and maintenance of the use of cephalexin for seven days.
Cases of hematoma and seroma, outflow of active secretion of blood or serous fluid for more than seven days, without collections or bulging in the breasts were considered. All spontaneously resolved with conservative treatment.
The six cases of dehiscence were also clinically managed, without re-approach, as they did not exceed a distance greater than 3mm.
The appearance of stretch marks in the breast in patients who underwent subglandular implants was 11.5% (3/26), while in the subfascial plane, it was 3.7% (3/81). This suggests a three times greater risk of streak formation when opting for the subglandular plane than the subfascial plane (p=0.22). Patients undergoing the “dual plane” (submuscular) technique did not present this clinical change.
Hyperesthesia in the nipple-areola complex was a complaint in three patients whose implants were in the subglandular plane, which was more superficial (p<0.05).
75% of operated patients did not present any clinical changes, and five patients were not followed up after the first consultation (p<0.001).
Complications are grouped in Table 2, divided between the different positions of the implants.
Hospital care and outpatient follow-up
The length of stay ranged from 2 to 3 days, and none of the patients required admission to the intensive care unit.
It was impossible to estimate the time taken for the patients to return to their usual activities due to irregular follow-up in the postoperative period and incomplete data in this regard.
So far, the follow-up of patients has ranged from 4 to 41 full months, with an average of 23.34 months.
All patients were questioned during their return to the clinic and considered themselves satisfied with the esthetic result.
DISCUSSION
Residents’ assessment of their education is an important parameter to analyze how their teaching and learning process is going. As reported by a German study, most residents who graduated from plastic surgery services do not feel confident about performing aesthetic procedures at the end of their training11. Many wish to have more cosmetic surgery performed during training. Augmentation mammoplasty is among the most cited by residents, who suggest performing at least 10 of these surgeries during their training. In our study, the average number of procedures per resident was 15, which makes training considered adequate from this perspective.
| Complications | Subglandular | Subfascial | “Dual plane” (submuscular) | Total | p1 |
|---|---|---|---|---|---|
| Seroma | 0 | 3 (3,7%) | 0 | 3 (2,5%) | 0,05 |
| Infection | 0 | 1 (1,2%) | 0 | 1 (0,8%) | 0,37 |
| Stretch marks | 3 (11,5%) | 3 (3,7%) | 0 | 6 (5%) | 0,22 |
| Bruise | 0 | 0 | 1 (4,3%) | 1 (0,8%) | 0,37 |
| Ptosis | 0 | 1 (1,2%) | 0 | 1 (0,8%) | 0,37 |
| Enlarged scar | 0 | 3 (3,7%) | 0 | 3 (2,5%) | 0,05 |
| Asymmetry | 0 | 1 (1,2%) | 1 (4,3%) | 2 (1,6%) | 0,61 |
| Hyperesthesia of CAP | 3 (11,5%) | 0 | 0 | 3 (2,5%) | 0,05 |
| Dehiscence | 1 (3,8%) | 5 (6,1%) | 0 | 6 (5%) | 0,03 |
| Breast tenderness | 1 (3,8%) | 1 (1,2%) | 1 (4,3%) | 3 (2,5%) | 1,00 |
| Without changes | 18 (69,2%) | 61 (75,3%) | 10 (43,4%) | 90 (75%) | <0,001 |
| No follow-up | 1 (3,8%) | 3 (3,7%) | 1 (4,3%) | 5 (4,1%) | 0,45 |
CAP: Areolar-papillary complex;
1 Chi-square test.
The importance of esthetic education during the years of medical residency also involves the preservation of the labor market. The invasion of other medical and non-medical specialties, in addition to legal actions in the legal environment, has to be fought with the knowledge and training of plastic surgeons capable and qualified to enter the labor market2.
The number of surgeries per resident in this article is within the 15% of aesthetic procedures that the National Medical Residency Council matrix recommends for specialist training.
In our sample, 77.5% (93/120) of augmentation mammoplasties occurred in the first half of the second year of residency, and implant surgeries in “dual plane” (submuscular) usually take place within four months of the second-year residence, and after at least ten augmentation mammoplasties in other plans. This can be explained by the need for muscle incision and more careful dissection.
The first- and second-year surgeons are accompanied by at least one other resident of the team as the first assistant, in addition to the presence of staff, usually a teacher or preceptor, who assesses the execution of the steps and guides in the main decision moments. Instrumentation was usually performed by a general surgery resident, or a nursing technician hired for the position. All anesthesia was performed by residents and/or preceptors of the HC FMB UNESP anesthesiology service.
A work by Hidalgo and Sinno, in 201612, pointed out the profile of breast augmentation surgeries in the United States performed by members of the American Society of Plastic Surgeons (ASPS). It showed a preference for round, smooth implants, 42% with 300 to 350cc and 42% above 350cc. Unlike our retrospective analysis, they indicated the subfascial plane as used in only 2.4%, while the inframammary route was also the most applied. Textured implants, which in our study were unanimous, accounted for only 10% of the choices in that article.
An assessment like this one was presented in the Revista Brasileira de Cirurgia Plástica by Charles-de-Sá et al. in 201913. In this study, there was also a preference for round implants over anatomical ones, in addition to a predominance of microtextured ones, followed by polyurethane implants. Skin incision in the inframammary position was also the majority, and the implant position in descending order of frequency was in the subfascial plane, followed by the subglandular and, finally, submuscular (“dual plane”), in proportions of 54, 26 and 14%, which is close to our experience.
In a retrospective study, Alves et al. (2018)14 evaluated as preferential the anatomical type implant as more “natural,” also using the Silimed® brand as a reference in this comparison.
The most frequent complications in our study were surgical wound dehiscence and cutaneous streaks in the breasts, both found in 5% of cases. Although complications can also be associated with the learning curve, some are also found in services with long-term professionals. Basile et al. (2012)15 reported 19 cases of stretch marks in 409 patients - 4.9% - evaluated in the postoperative period of augmentation mammoplasty. The authors mentioned age as a risk factor for this complication, as younger patients are more prone to fiber rupture during skin distension. Tijerina et al. (2010)16 and Brown (2020)17 performed retrospective analyzes of 1,000 and 783 cases of primary augmentation mammoplasty. The main complication found by both was capsular contracture, 0.4% and 6.8%, respectively. In our analysis, this complication was not evidenced; however, one must consider the fact that our observation time, which is a key factor in this complication, was inferior.
When comparing the positions of the implants concerning complications, we noticed that patients who underwent the subfascial technique were those who had fewer postoperative complications. This differs from Brown et al. (2012)18, who reported no significant difference when comparing the subglandular and subfascial positions. However, when in the subfascial position, we present a higher rate of seroma, which differs from the meta-analysis carried out by Li et al. (2019)19, who found no differences in the seroma rate between implants placed in planes above or below the pectoralis muscle.
As described in another large case series20, in which there are very low levels of complications during and after augmentation mammoplasty, we did not obtain any major complications, such as venous thromboembolism.
Another topic to be discussed is the increasing evidence and new research related to anaplastic large cell lymphoma associated with a breast implant (BIA-ALCL). This also interferes in this discussion and may affect shortly much of what is considered about the use of prostheses21,22.
Despite satisfactory postoperative results and a substantial number of procedures, more concrete teaching assessment tools need to be implemented to create replicable training standards for new plastic surgeons. One of these tools present in the current literature is the so-called “entrustable professional activities” (EPA)23,24. In this method, we try to translate the skills of each surgical procedure. In theory, upon reaching pre-determined competencies, the surgeon in training would be really qualified for unsupervised performance25. This mechanism can potentially make training more objective and help organize inputs and resources spent on training the plastic surgeon.
The EPA for augmentation mammaplasty can be later translated into Portuguese and adapted to the reality of every service.
Among the limitations of this study, we must comment on its retrospective character, which was carried out under the analysis of medical records. This impairs the assessment of data such as the quality of healing and patient satisfaction since the evaluators described them in a less objective character.
Mammoplasty is the most common surgery performed by plastic surgeons in their clinical practice, which makes it essential in the technical training of the resident physician in the specialty. Maintaining a routine and a pattern in its performance is important for the specialist’s evolution, both for the refinement of one of his most sought-after surgeries and the development of the skills needed to perform more complex surgeries.
Monitoring the evolution of the school service over time and following the patients who received implants is essential to identify possible complications early and offer patients satisfactory and long-lasting results.
CONCLUSION
Primary augmentation mammoplasty is one of the main procedures in most plastic surgery offices. When performed in a medical residency service, by plastic surgeons in training under adequate supervision can also bring satisfactory results, with low complication rates.
REFERENCES
1. International Survey on Aesthetic/Cosmetic Procedures (ISAPS). ISAPS International Survey on Aesthetic/Cosmetic Procedures [Internet]. West Lebanon: ISAPS; 2018; 1-49. Available from: https://www.isaps.org/wp-content/uploads/2019/12/ISAPS-Global-Survey-Results-2018-new.pdf
2. Rohrich RJ. The importance of cosmetic plastic surgery education: an evolution. Plast Reconstr Surg. 2000 Fev;105(2):741-2.
3. Sociedade Brasileira de Cirurgia Plástica (SBCP). Serviços credenciados da SBCP. São Paulo: SBCP; 2017.
4. Ministério da Saúde (BR). Resolução no 43, de 8 de abril de 2019. Estabelece novo prazo para entrada em vigor da Resolução Normativa nº 39, de 20 de junho de 2018, do Conselho Nacional de Controle de Experimentação Animal, que dispõe sobre restrições ao uso de animais em procedimentos classificados com grau de invasividade 3 e 4. Diário Oficial da União, Brasília (DF), 11 set 2019; Edição: 70; Seção: 1:85.
5. Coleman SR, Saboeiro AP. Primary breast augmentation with fat grafting. Clin Plast Surg. 2015 Jul;42(3):301-6.
6. Kerfant N, Marchac A, Auclair E. Fat grafting in composite breast augmentation with round implants: a new concept for breast reshaping. Aesthet Plast Surg. 2019;550-1.
7. Mallucci P, Branford OA. Concepts in aesthetic breast dimensions: analysis of the ideal breast. J Plast Reconstr Aesthet Surgery. 2012 Jan;65(1):8-16.
8. Tebbetts JB. Dual plane breast augmentation: optimizing implant-soft-tissue relationships in a wide range of breast types. Plast Reconstr Surg. 2006 Dez;118(7 Suppl):81S-98S;discussion:99S-102S.
9. Wan D, Rohrich RJ. Modern primary breast augmentation: best recommendations for best results. Plast Reconstr Surg. 2018 Dez;142(6):933e-46e.
10. Tebbetts JB, Adams WP. Five critical decisions in breast augmentation using five measurements in 5 minutes: the high five decision support process. Plast Reconstr Surg. 2005 Dez;116(7):2005-16.
11. Momeni A, Goerke SM, Bannasch H, Arkudas A, Stark GB. The quality of aesthetic surgery training in plastic surgery residency: a survey among residents in Germany. Ann Plast Surg. 2013 Jun;70(6):704-8.
12. Hidalgo DA, Sinno S. Current trends and controversies in breast augmentation. Plast Reconstr Surg. 2016 Abr;137(4):1142-50.
13. Charles-De-Sá L, Gontijo-De-Amorim NF, Albelaez JP, Leal PR. Profile of breast augmentation surgery in Brazil. Rev Bras Cir Plást [Internet]. 2019; 34(2):174-86. Disponível em: http://www.gnresearch.org/doi/10.5935/2177-1235.2019RBCP0132
14. Alves DG, Santos Junior CAN, Vilca MMR, Arruda SCG, Medeiros MPC, Decusati FL. Análise comparativa entre indicações de implantes anatômicos ou redondos em mamoplastia de aumento. Rev Bras Cir Plást [Internet]. 2018; 33:5-6. Disponível em: http://www.rbcp.org.br/details/2098/analise-comparativa-entre-indicacoes-de-implantes-anatomicos-ou-redondos-em-mamoplastia-de-aumento
15. Basile FV, Basile AV, Basile AR. Striae distensae after breast augmentation. Aesthetic Plast Surg. 2012 Ago;36(4):894-900.
16. Tijerina VNE, Saenz RAE, Garcia-Guerrero J. Experience of 1000 cases on subfascial breast augmentation. Aesthetic Plast Surg. 2010 Fev;34(1):16-22.
17. Brown T. A comprehensive outcome review of subfascial breast augmentation over a 10-year period. Plast Reconstr Surg. 2020 Dez;146(6):1249-57.
18. Brown T. Subfascial breast augmentation: is there any advantage over the submammary plane? Aesthetic Plast Surg. 2012 Jun;36(3):566-9.
19. Li S, Mu D, Liu C, Xin M, Fu S, Xu B, et al. Complications following subpectoral versus prepectoral breast augmentation: a meta-analysis. Aesthetic Plast Surg. 2019 Ago;43(4):890-8.
20. Alderman AK, Collins ED, Streu R, Grotting JC, Sulkin AL, Neligan P, et al. Benchmarking outcomes in plastic surgery: national complication rates for abdominoplasty and breast augmentation. Plast Reconstr Surg. 2009 Dez;124(6):2127-33.
21. Groth A, Graf R. Breast implant-associated anaplastic large cell lymphoma (BIA-ALCL) and the textured breast implant crisis. Aesthetic Plast Surg. 2020 Feb;44(1):1-12.
22. Clemens MW, Jacobsen ED, Horwitz SM. 2019 NCCN consensus guidelines on the diagnosis and treatment of breast implant-associated anaplastic large cell lymphoma (BIA-ALCL). Aesthet Surg J. 2019 Jan;39(Supl 1):S3-13.
23. Cate OT. Nuts and bolts of entrustable professional activities. J Grad Med Educ. 2013 Mar;5(1):157-8.
24. Jones Junior MD, Rosenberg AA, Gilhooly JT, Carraccio CL. Perspective: competencies, outcomes, and controversy--linking professional activities to competencies to improve resident education and practice. Acad Med. 2011 Fev;86(2):161-5.
25. Courteau BC, Knox ADC, Vassiliou MC, Warren RJ, Gilardino MS. The development of assessment tools for plastic surgery competencies. Aesthet Surg J. 2015 Jul;35(5):611-7.
1. Hospital das Clínicas, Faculty of
Medicine of Botucatu, Botucatu, SP, Brazil.
BFMN Analysis and/or data interpretation, Conception and design study, Data Curation, Final manuscript approval, Formal Analysis, Investigation, Methodology, Project Administration, Supervision, Writing - Original Draft Preparation, Writing - Review & Editing.
MSS Analysis and/or data interpretation, Conceptualization, Writing - Original Draft Preparation, Writing - Review & Editing.
Corresponding author: Balduino Ferreira de Menezes Neto, Rua Hortênsia, 291, Apto 802, Jardim Bom Pastor, Botucatu, SP, Brasil, Zip Code 18607-650, E-mail: balduino.neto@unesp.br
Article received: October 18, 2020.
Article accepted: July 14, 2021.
Conflicts of interest: none.
Institution: Hospital das Clínicas da Faculdade de Medicina de Botucatu, Botucatu, SP, Brasil.






 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter