

Articles - Year 1997 - Volume 12 -
The Digital Neurovascular Island Flap Applied In Acute Injuries
Retalho da Artéria Colateral Digital na Urgência
ABSTRACT
The authors present 20 cases of digital neurovascular island flaps applied in acute injuries. Sixty-one patients treated over the last 3 years of severe digital tissue losswere analysed. 70% of cases were sited at the distal phalanx. Eight patients were treated with direct island flaps to restore skin and sensibility of small oblique distal losses. Seven patients presenting more transverse and extensivo lesions needed reverse flow island flaps. Three patients with partial pulp amputation of the thumb were treated with island bipedicled flaps. Finally, in the other two patients with total loss of thumb pulp, heterodigital island flaps with neurotization of the flap were necessary to restore the thumb whole digital pulp. The functional and aesthetic aspects of the reconstructions were analysed and compared with the traditional methods.
Keywords:
RESUMO
Os autores apresentam 20 casos de retalhos da artéria colateral digital utilizados na urgência. Foram analizados 61 pacientes que nos últimos 3 anos sofreram quadro agudo de perda de substância digital. Destes, 70% envolveram a falange distal. Em 8 pacientes foi proposto o retalho em ilha direto para cobrir perdas de substância oblíquas menores. Em 7 pacientes foi utilizado o retalho em ilha de fluxo reverso para restaurar sensibilidade e/ou cobrir perdas mais extensas. Em 3 casos de perda de parte de polpa do polegar foi indicado o retalho em ilha bipediculado. Finalmente, em 2 casos foi utilizado o retalho em ilha heterodigital para reconstruir toda a polpa digital do polegar. Os aspectos funcionais e estéticos da reconstrução foram analisados e comparados com os métodos tradicionais.
Palavras-chave:
Small tissue losses involving the digital distal segment are quite frequent. The covering method must be elected on account of innumerable criteria. All methods, however, must have in common the skin and subcutaneous tissue replacement for a tissue presenting the same characteristics and sensibility. Such an ideal situation is achieved only if the skin adjoining to the defect is used. The defect topography, the affected finger, the associated lesions of the injured finger and of the neighbouring fingers, the post-operative re-education, the functional necessities, the patient's age and sex, all these factors interfere in this therapeutic choice. All covering techniques, from the simple directed healing to the microsurgical transplantation, must be known in detail, aiming at providing the patient with the most adequate answer. The practice of small local flaps, however, requires a deep knowledge of the hand vascularization.
In this work, the utilization of flaps vascularized by the digital colateral artery for covering tissue losses of the long fingers and thumb will be analysed. The use of these flaps was introduced in 1955 by Moberg(5) and made popular by Littler(4) and Tubiana(6). Different island flaps, both homodigital and heterodigital, were described. They are particularly indicated in the digital pulp reconstruction, which requires a consistent, sensible and good looking covering.
There are two types of homodigital island flaps appliable to fingers: 1 - direct island flap, described by Venkataswami and Subramanian in 1980(7) from the initial works by Hueston in 1966(3); 2 - reverse flow island flap, described by Glicenstein(2) and Brunelli(1).
As to the heterodigital flaps, indication is basically restricted to those cases of extensive loss of thumb digital pulp, where the distal phalanx ulnar rim of the annular finger is used as donor site for the cutaneous covermg.
MATERIAL AND METHOD
In 19 patients ofthe total 61 cases of traumatic tissue loss in long fingers and thumb treated between 1991 and 1994 at the Clínica SOS Mão, 20 digital colateral artery flaps were utilized.
Sixty-five per cent of the cases were represented by the digital colateral artery flap of proximal flow On the long fingers, the flap was outlined having as axle one of the palmar neurovascular pedicles. When the case referred to losses of the finger itself, the flap distal limit was the lesion rim itself. In the heterodigital reconstructions (eg. thumb), however, the flap included the whole hemipulp. Depending on the loss extension, it proceeded proximally as far as the median phalanx. The lateral limits were the median line of the volar face and the median-lateral line, laterally.
The dissection was performed under pneumatic tourniquet and the flap was raised from the deep plan always next to the digital channel. A lateral incision connecting the interdigital plicae extremities, as far as the finger base or even more proximally on the palm, permitted to approach the neurovascular pedicle. After releasing the pedicle, the flap was advanced to the distal loss ar transposed to another finger by means of tunnelization, when the case required it.
The donor site was covered with a total skin graft and the finger was kept under slight flexion to prevent tensioning the pedicle.
On the thumb, the flap was utilized from both neurovascular pedicles (O'Brien), permitting the total advancement of the volar skin to the distal loss site (Fig. 1). The marking was performed in quadrilateral form, having as proximal limit the median portion of the proximal phalanx and as lateral limit the median-lateral lines of either side. The pedicle was accessed by means of an ample detachment of the proximal skin, permitting the release and advance of the flap under no tension (Fig. 2). The donor site was treated likewise, and the whole finger was kept under slight IF flexion. The fmal result was always satisfactory (Fig. 3).
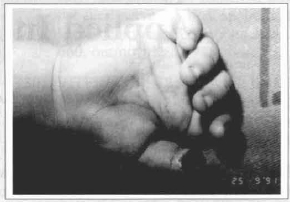
Fig. 1 - Partial tissue loss of a right thumb pulp in a 4-year-old ehild.
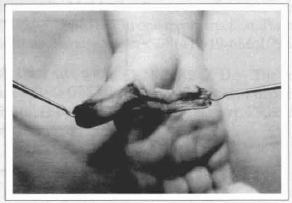
Fig. 2 - The bipedicled homodigital flap is disseeted to permit the advancement to the loss site.

Fig. 3 - The result of 6 post-operative months shows adequate acommodation of the flap skin and graft at the donor site.
The digital colateral artery flap of reverse flow was marked on the proximal phalanx of the finger to be reconstructed (Fig. 4). Its limits were the median and lateral axle of the finger and the flexion plicae proximally and distally. When the flap was indicated for covering but did not require sensibility, it was transposed only with the vascular pedicle (Fig. 5). In such a case, care was taken to keep the greatest possible amount of adipose tissue around the pedicle to prevent venous suffering problems. The losses treated with this kind of non-resensibilizable flap were generally sited on the dorsum of the median and distal phalanx (Fig. 6). As to the larger losses ofthe distal phalanx (Fig. 7), the flap was transposed with the colateral nerve to be resensibilized from the contralateral nerve. The flap was initially approached and the neurovascular pedicle was proximally identified, with the care of preserving the dorsal branch of the colateral nerve which originates next to the digital-palmar plica; the nerve was then dissected palmward 1 cm from the flap rim and sectioned. Then a median-lateral incision as far as the tissue loss site permitted the pedicle disection, which did not go beyond the digital plica of the IFD (Fig. 8).
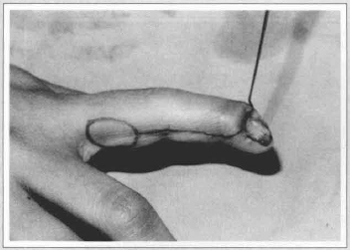
Fig. 4 - Marking of the reverse flow island flap at the ulnar rim of the proximal phalanx to cover dorsal osseous exposure of the distal phalanx. The pedicle is accessed by means of a median-lateral incision from the donor site as far as the cutaneous loss site.
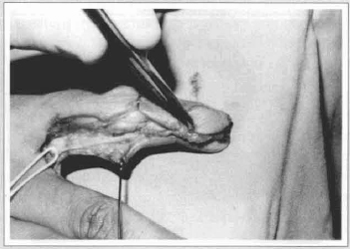
Fig. 5 - After dissection of the vascular pedicle without the nerve, the flap is transposed to the receptor bed. Observe that the pedicle dissection must not go beyond the distal third of the median phalanx to prevent sacrificing the last transverse branch which communicates with the contralateral pedicle.
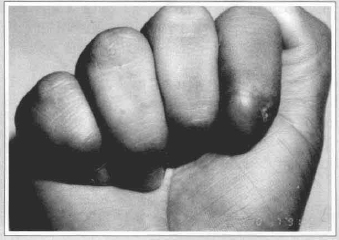
Fig. 6 - Result after 3 post-operative months, with good aesthetie aspect of the reconstructed area.
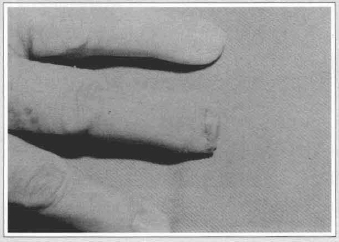
Fig. 7 - Transverse amputation at the level of the median third of the distal phalanx with loss of a considerable portion of the ungual bed.
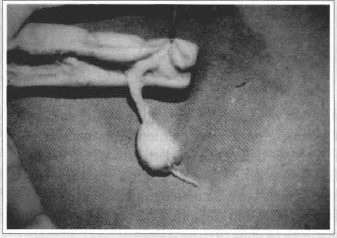
Fig. 8 - Reverse flow island flap dissected along with the colateral nerve. Observe that the proximal stump was sectioned at 1 cm from the flap rim, to permit the neurorrhaphy with the contralateral nerve.
The flap was then transposed to the tissue loss site, with care being taken only to prevent torsioning and tensioning the pedicle. After suture of the flap and donor site of access to the vessels, the colateral nerve previously dissected was finally sutured with the proximal stump of the flap nerve (Fig. 9). The donar site was grafted with total skin.
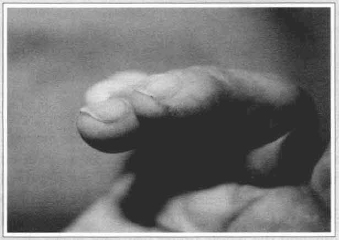
Fig. 9 - Result after one post-operative year, showing the ungual bed recovering with the filling of the fingertip with the flap. The flap was satisfactorily resensibilized.
RESULTS
The traumatic tissue losses of long fingers and thumb treated with digital colateral artery flaps represented only 30% of the total 61 patients assisted over the last three years.
The most common causes of the accidents were domestic (40.9%), work (22.95%), street and road (11.5%) and sport (6.54%). The most affected fingers were the forefinger (33.84%), the middlefinger (24.61%), the annular (21.53%), the minimus (10.76%) and the thumb (9.23%). The right hand, being the dominant one in the majority of the population, was involved in 57.37% of the cases, compared to 42.63% of occurrences on the left hand. In 73.35% of the cases there was no association with other lesions, but only the tissue loss itself, while in the remaining 26.7% the lesion was associated with fracture (13.3%), devascularization (5%), sinews and nerves section (3.3%) and other occurrences (3.3%).
The dimensions varied depending on the loss extension and the patient's age, but they generally did not go beyond one third of the finger total length in the unipedicled flaps and 50% of the volar surface in the bipedicled ones (O'Brien).
Complications represented up to 15% of the cases (3 cases); in 10% there was total loss of the flap and, in the remaining 5%, partial loss. In those cases, the lesion extension was probably inadequately evaluated, and the vascular pedicle might have been already affected. All of those cases occurred in the reverse flow flap.
DISCUSSION
Innumerable techniques of digital tissue loss covering have been described and are successfully utilized nowadays. The indication of more complex surgical procedures is dominam when there is osseous exposure. The osseous covering provided by direct suture or cutaneous grafting produces unsatisfactory results and the cutaneous flap is preferable. When there is minimal osseous exposure, the covering with local advance flaps is possible (Hueston 1966, Tranquilli-Leali 1935 and Tubiana 1986), but the larger the cutaneous loss area, the more complex the procedure. Until recently the most extensive cutaneous losses were covered with flaps distant from the temporary pedicle (cross-finger or thenal flap). This resulted in fingers with good aspect but with no sensibility, aesthetic sequela of the donor site and risk of articular rigidity due to the extensive immobilization period (generally three weeks). Nowadays the indications for this kind of flap became less common due to the development of island flaps, a technique which permits reconstruction in a single surgical time. The choice is essentially made between two types of island flap. The choice between the two techniques depends on the patient's clinic status and the surgeon's experience. As a general rule, the transverse or slightly oblique amputations are better treated with advance local flaps. The oblique amputations, where the amputation line ends at the median portion of the distal phalanx are preferably treated with direct island flaps. In all remaining cases, the reverse flow flap must be indicated.
The problems which affect this kind of flap are basicaliy the rectratile median-lateral scar with [?] IFP [?] flexion, which may be corrected with z-plasty and physiotherapy; the flap hyperesthesia, which tends to decrease on the first months, and the cutaneous anesthesia at the proximal areas which are always denervated with the pedicle dissection.
However, the advantages are evident as compared with other alternatives. This flap provides a covering in a single surgical time, with good quality and sensibility, permitting the maximum preservation of the finger length.
In reverse flow flaps, the neurorrhaphy of one of the colateral nerves with the contralateral nerve is possible, thus preventing one of the greatest problems with the amputation stumps, which are the neuromas. In addition, it permits the transposition of a large skin segment with reinnervation possibility.
REFERENCES
1. BRUNELLI, F. 1987 - Lambeau en ilôt digital inversé. Pages at GEM winter meeting, Paris.
2. GLICENSTEIN, J. 1988 - Table ronde: Les lambeaux en ilôts en chirurgie de la main. Annales de Chirurgie de La Main 7: 119-121.
3. HUESTON, J. T. 1966 - Local flap repairs in the finger tip injuries. Plastic and Reconstructive Surgery 37: 349-350.
4. LITTLER, J. W 1956 - Neurovascular pedicle transfer of tissue in reconstructive surgery of the hand. Journal of Bone and Joint Surgery 38A: 917.
5. MOBERG, E. 1964 - Aspects of sensation in the reconstructive surgery of the upper extremity. Journal of Bone and Joint Surgery 46: 817-825.
6. TUBIANA, R.; DUPARC, J. 1959 - Operation palliative pour paralysis sensitive à la main. Memoires de l'Academie des Chirurgiens. 85: 66-670.
7. VENKATASWAMI, R.; SUBRAMANIAN, N. 1980 - Oblique triangular flap: a new method of repair for oblique amputations of the fingertip and thumb. Plastic and Reconstructive Surgery 66: 296-300.
I - Staff Member, Microsurgery Division - HTO - MS - Rio de Janeiro
Staff Member, Clínica SOS Mão - Rio de Janeiro
Titular Member, SBCP
II - Chief, Microsurgery Division - HTO - MS - Rio de Janeiro
Staff Member, Clínica SOS Mão - Rio de Janeiro
Titular Member, SBCP
Clínica SOS Mão
Rua São João Batista, 80 - Botafogo
22270-030 - Rio de Janeiro - RJ - Brazil
Phone/Fax: +55 21 266-6004


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter