

Case Report - Year 2022 - Volume 37 -
The use of parietotemporal fascia flap in the treatment of recurrent cholesteatoma: clinical case
O uso do retalho de fáscia parietotemporal no tratamento do colesteatoma recidivado: caso clínico
ABSTRACT
Cholesteatoma consists of an inflmmatory process that results in the migration of squamous keratinized epithelium into the middle ear. Although regarded as a histopathologically benign entity it can behave quite aggressively being an important cause of deafness in all countries. Ear discharge, pain, ear drum rupture with extension into the inner ear leading to deafness and vertigo, are the most common clinical manifestations. Treatment consists of surgically excising all the foreign epithelium from the middle ear. Recurrences can be as high as 50% and are a challenge to Ear, Nose and Throat doctors. In this case report we describe a case of an acquired recurrent cholesteatoma in a tertiary hospital in Portugal, treated with radical ablation of middle ear and mastoid cavity by the otolaryngologists. The chosen reconstructive option was obliteration of the dead space using a temporo-parietal fascial flap by the Plastic Surgery Department
Keywords: Cholesteatoma, Middle ear; Surgical flaps; Middle ear, surgery; Mastoidectomy; Reconstructive surgical procedures.
RESUMO
O colesteatoma consiste em um processo inflamatório que resulta na migração do epitélio escamoso queratinizado para o ouvido médio. Embora considerada uma entidade histopatologicamente benigna, pode se comportar de forma bastante agressiva sendo uma importante causa de surdez em todos os países. Descarga, dor, ruptura do tímpano com extensão para o ouvido interno levando à surdez e vertigem, são as manifestações clínicas mais comuns. O tratamento consiste na excisão cirúrgica de todo o epitélio estranho da orelha média. As recorrências podem chegar a 50% e são um desafio para os médicos de ouvido, nariz e garganta. Neste relato de caso descrevemos um caso de colesteatoma recorrente adquirido em um hospital terciário em Portugal, tratado com ablação radical de ouvido médio e cavidade mastóide pelos médicos otorrinolaringologistas. A opção reconstrutiva escolhida foi a obliteração do espaço morto com retalho fascial temporo-parietal pelo Serviço de Cirurgia Plástica.
Palavras-chave: Colesteatoma da orelha média; Retalhos cirúrgicos; Orelha média; cirurgia; Mastoidectomia; Procedimentos cirúrgicos reconstrutivos
INTRODUCTION
Cholesteatoma is a histopathologically benign entity but locally very aggressive, being an important cause of chronic otitis media and deafness.
Congenital or acquired, it consists of a chronic inflammatory process that results in the migration of keratinized epithelium from the tympanic membrane to the middle ear.
The accumulation of keratin plaques is the underlying factor in the etiology of cholesteatoma. The characteristic clinical findings are purulent otorrhea, tympanic perforation extending to the inner ear and erosion of the ossicles with hearing loss or deafness1.
Treatment consists of eradicating all middle ear tissue; however, relapse rates can be high, from 8% to 50%2. Recurrence usually manifests with postoperative otorrhea3.
The mastoidectomy ablation area can be quite extensive and, to avoid complications, its obliteration is important4. Obliteration can be achieved with the use of alloplastic materials or autologous reconstruction. Lipofilling or adipose autograft is the most used method of obliterating the mastoid cavity in the literature5,6.
The temporal fascia flap is an established surgical technique for mastoid reconstruction3. Descriptions of this flap for this purpose can be found in the literature.
In this clinical case, we discussed the surgical approach of a recurrent cholesteatoma, which underwent reconstruction with a temporal fascia flap after radical excision by the Otorhinolaryngology (ENT) service Plastic Surgery.
OBJECTIVE
This work aims to present the temporal fascia flap as a suitable surgical option for the reconstruction of the mastoid cavity.
CASE REPORT
A 50-year-old male Caucasian patient was diagnosed with chronic otitis media cholesteatomatous on the left.
The first manifestation of the disease occurred 4 years earlier, in May 2014, with an episode of left suppurative otitis media, and after several relapses, it progressively evolved into chronic otitis media.
During this period, he continued to be followed up in the ENT service of the Centro Hospitalar e Universitário de Coimbra.
The disease had periods of remission and recurrence, gradually progressing to a lytic lesion of the inner ear with cophosis.
He underwent multiple cycles of empiric and targeted antibiotics, washes and topical corticosteroids. In the laboratory, the only microorganism identified was Pseudomonas aeruginosa.
Imagiologically, maxillofacial computed axial tomography (CAT) described a polypoid lesion extending to the external auditory canal.
Biopsy revealed inflammatory tissue with granulation and excluded a neoplastic lesion.
In December 2016, the patient underwent modified radical mastoidectomy and meatoplasty, and in November 2017, open mastoidectomy with surgical cleaning, mastoid cavity reduction with cartilage, tympanoplasty with perichondrium and fascia, and meatoplasty revision.
In July 2018, after a new recurrence and the cophosis was installed, a mastoidectomy review and dead space obliteration with a temporal fascia flap were proposed.
Anatomical considerations
The parietotemporal fascia is an extension of the superficial muscular aponeurotic system (SMAS) inferiorly and the galea aponeurotic superiorly.
In the temporal fossa, it is found superficial to the deep temporal fascia and the temporal muscle. Above the temporal muscle, the parietotemporal fascia lies immediately above the periosteum.
It is a thin fascia vascularized by the superficial temporal artery (TS).
The TS artery is a branch of the external carotid. It is a small-caliber artery, approximately 1-3 mm in diameter. A vein of a similar caliber usually accompanies it. These vessels run anterior to the pinna, and the pulse can be easily palpated.
Along its course, the TS artery branches supply the parietotemporal fascia, helix, temporal muscle, and scalp.
Pitanguy Line: the frontal branch of the facial nerve runs on an imaginary line 0.5 cm below the tragus and 1.5 cm above the lateral border of the supercilium and is at risk of being severed if the dissection is too deep. This imaginary line is called Pitanguy’s line and is an anatomical reference that must be respected.
The auriculotemporal branch runs posterior to the artery and is a sensory nerve to the scalp. This branch of the maxillary nerve (in turn, one of the branches in the trigeminal cranial nerve - CN V) is often sacrificed in dissection, resulting in an area of hypoesthesia of the scalp.
Surgical technique
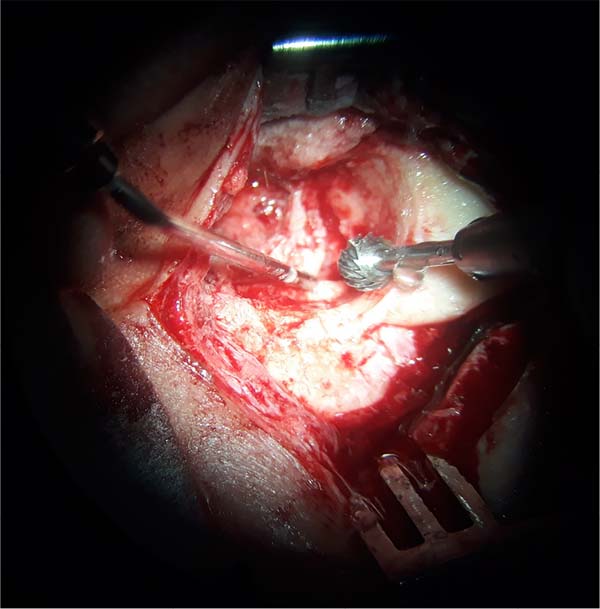
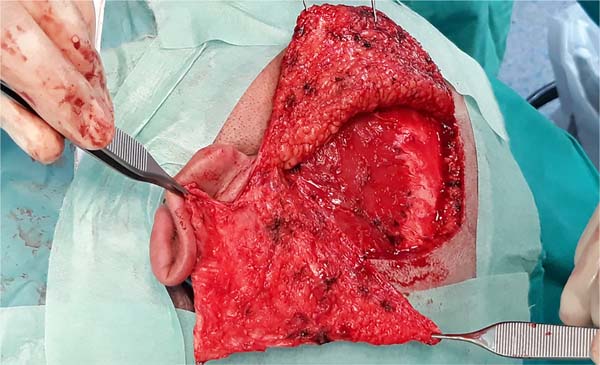
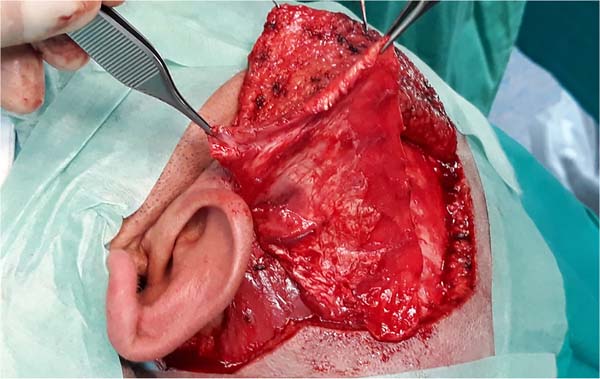
ENT mastoidectomy review (Figures 1, 2 and 3)
Patient undergoing removal of epithelial and mucosal tissue from the petromastoid emptying cavity. The limits were sharpened with a diamond bur, and the tympanic membrane was removed.
Lifting of skin tissue from the external auditory canal (EAC).
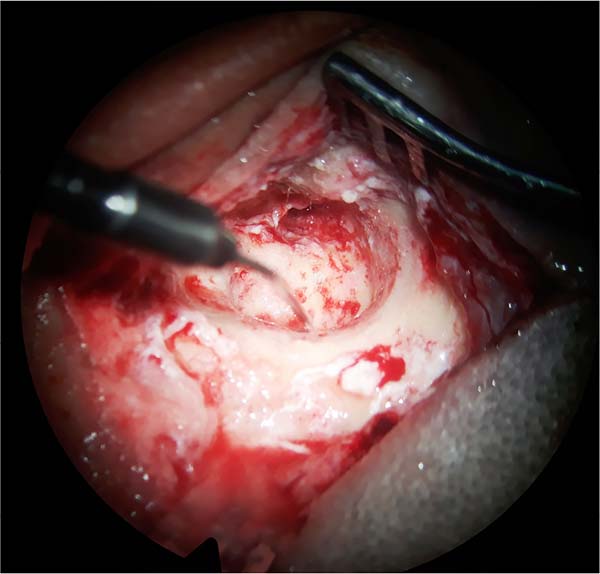
Superficial parietotemporal fascia flap
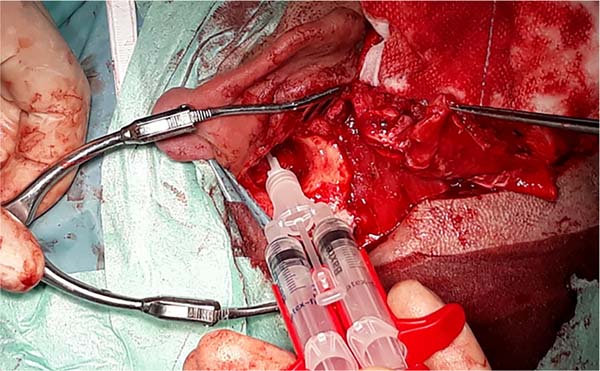
To expose the fascia, make a “V”-shaped skin incision in the pre-auricular region (Figure 4).
The scalp is dissected from the fascia similarly to a rhytidectomy. The intended plane is immediately superficial to the superficial parietotemporal fascia.
In this step, care must be taken not to injure the follicles and cause alopecia.
After exposing the fascia and identifying the vascular pedicle, the flap is delimited by making an incision to the desired plane, which is the posterior leaflet of the deep temporal fascia.
Subsequently, the flap is lifted from distal to proximal, tapering as we approach the vascular pedicle. In this step, care must be taken not to injure the frontal branch of the facial nerve.
The auriculotemporal branch of the maxillary nerve is often sacrificed, resulting in an area of scalp hypoesthesia.
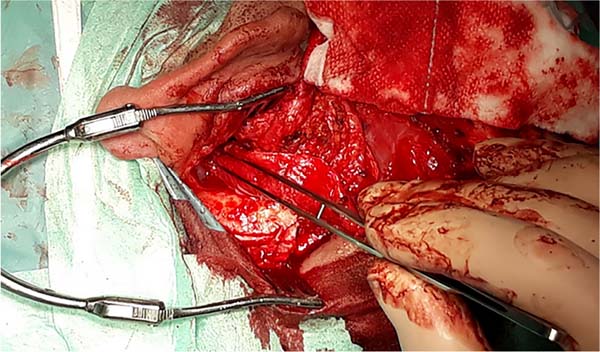
The temporal fascia flap based on the superficial temporal vessels can be visualized (Figures 5 and 6).
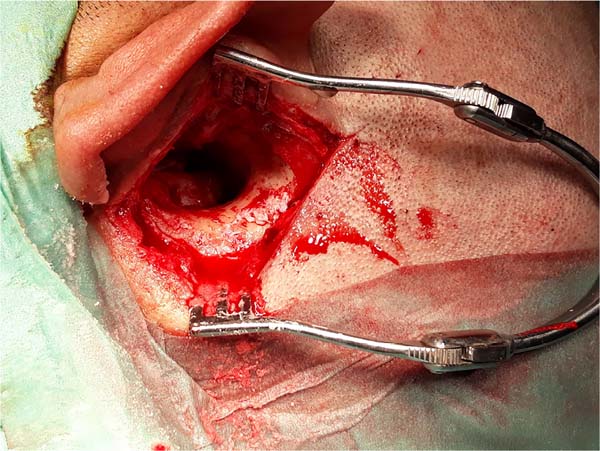
The “Inset” in the cavity obliterates all dead space (Figures 7, 8 and 9). Fibrin glue was used to promote adhesion.
The meatus of the EAC is left to epithelialize by the second intention, applying a dressing with fat gauze.
The suture is performed in layers, and an aspiration drain is left and removed in the immediate postoperative period (Figure 10).
This reconstructive technique presents a good final functional and aesthetic result at 5 months postoperatively, with total epithelialization of the external auditory meatus and no signs of recurrence (Figure 11).
Results
In the clinical case presented, the treatment was effective. Outwardly, only a fully epithelialized meatus of the ear canal can be seen, with no suspicion of cholesteatoma recurrence.
At the time of discharge from the Plastic Surgery consultation, 5 months after reconstruction with a temporal fascia flap (Figure 11), the patient was doing well and had no clinical complaints. He had preserved facial movements, demonstrating the integrity of the facial nerve, namely the frontal branch. There were no further episodes of recurrence such as otorrhea or suspicions of disease progression such as vertigo or headache.
DISCUSSION
The temporal fascia flap is a versatile flap, generally used in head and neck reconstruction7.
It aims to obliterate dead space and increase vascularization of the affected anatomical area, consequently improving the supply of antibiotics. This is the main advantage compared to other non-vascularized reconstructive options, such as adipose autograft or the use of alloplastic material8.
The temporal fascia flap is an effective technique in the plastic surgeon’s arsenal to reconstruct the temporal region with good long-term results9. In this sense, it presents itself as an adequate technique to obtain obliteration of the middle ear and mastoid, especially important in patients with locally advanced disease who require extensive mastoidectomy.
It also has advantages compared to other reconstructive options, namely the temporal myofascial flap. The main disadvantage of this flap is the excessive volume of the flap and less plasticity when compared to the temporal fascia flap.
As it is a fascial flap, the sequelae, such as the aesthetic deformity caused to the donor area, are minimal, and the scar is inconspicuous on the scalp.
The advantage of approaching pathologies in multidisciplinary teams is also highlighted, as is the role of Plastic, Reconstructive and Aesthetic Surgery as a last-line reconstructive surgical specialty in a multipurpose hospital.
CONCLUSION
In the clinical case presented, the treatment choice proved to be effective in achieving the proposed objective of obliterating the mastoid cavity without recurrences and with the least possible morbidity.
This work was also intended to briefly present the surgical technique to make its execution reproducible and simple.
REFERENCES
1. Vartiainen E. Factors associated with recurrence of cholesteatoma. J Laryngol Otol. 1995;109(7):590-2.
2. Rutkowska J, Özgirgin N, Olszewska E. Cholesteatoma Definition and Classification: A Literature Review. J Int Adv Otol. 2017;13(2):266-71.
3. Hung T, Leung N, van Hasselt CA, Liu KC, Tong M Long-term outcome of the Hong Kong vascularized, pedicled temporalis fascia flap in reconstruction of mastoid cavity. Laryngoscope. 2007;17(8):1403-7.
4. Skoulakis C, Koltsidopoulos P, Iyer A, Kontorinis G. Mastoid Obliteration with Synthetic Materials: A Review of the Literature. J Int Adv Otol. 2019;15(3):400-4.
5. Çath T, Çelik C, Olgun L. Subtotal Petrosectomy and Blind Sac Closure of the External Auditory Canal: Single-Center Experience with 44 Cases. Turk Arch Otolaryngol. 2014;52(3):81-6.
6. Pyle GM, Wiet RJ. Petrous Apex Cholesteatoma: Exteriorization vs. Subtotal Petrosectomy with Obliteration. Skull Base Surg. 1991;1(2):97-105.
7. Demirdover C, Sahin B, Vayvada H, Oztan HY. The versatile use of temporoparietal fascial flap. Int J Med Sci. 2011;8(5):362-8.
8. Yung M. The Use of Temporoparietal Fascial Flap to Eliminate Wound Breakdown in Subtotal Petrosectomy for Chronic Discharging Ears. Otol Neurotol. 2016;37(3):248-51.
9. Karimnejad K, Akhter AS, Walen SG, Mikulec AA. The temporoparietal fascia flap for coverage of cochlear reimplantation following extrusion. Int J Pediatr Otorhinolaryngol. 2017;94:64-7.
1. Coimbra Hospital and University Center, Plastic Surgery and Burns, Coimbra, Portugal.
| COLLABORATIONS | |
|---|---|
| JBF | Analysis and/or data interpretation, Conceptualization, Formal Analysis, Investigation, Realization of operations and/or trials, Writing - Original Draft Preparation, Writing - Review & Editing |
| CB | Analysis and/or data interpretation, Investigation |
| RM | Visualization |
| MJFS | Realization of operations and/or trials, Supervision |
Corresponding author: João Baltazar Ferreira, Praceta Professor Mota Pinto, Coimbra, Portugal, Zip Code 3004-561, E-mail: joao_cbf@msn.com
Article received: October 19, 2020.
Article accepted: April 23, 2021.
Conflicts of interest: none.


















 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter