

Case Report - Year 2022 - Volume 37 -
Forearm reconstruction with acellular dermal matrix after giant plexiform neurofibroma excision: case reports
Reconstrução do antebraço com matriz dérmica acelular após excisão de neurofibroma plexiforme gigante: relato de casos
ABSTRACT
Introduction: Giant plexiform neurinoma is a neuroectoderm and inherited disease. It is an uncommon skin tumor associated with NF1, characterized as a benign peripheral nerve sheath tumor surrounding multiple nervous fascicles. The goals of forearm coverage reconstruction are to protect the structures running to the wrist and hand and prevent scarring that leads to movement loss. Both forearm and hand play functional and social roles. Successful management of complex wounds is necessary for the overall functional rehabilitation of these patients.
Case Report: A 31-year-old woman presented at the plastic surgery division with a giant plexiform neurofibroma in the right forearm. After careful resection, all anterior forearm tendons were exposed. The defect was covered with graftable Pelnac T (thickness of 3mm and sizing 12 X 24cm2), fixed with 4-0 monocryl sutures. After 10 days, the acellular dermal matrix silicone layer was removed, and a split-thickness skin meshed graft was placed. On day 7, the acellular dermal matrix showed good signs of intake. On day 17, we observed a 95% graft survival. At the 3-month follow-up, reconstruction was stable without contouring defects, the hand had full range of motion, and the patient had no problems in daily activities.
Conclusions: Acellular dermal matrix appears to be a useful option in covering complex defects in the forearm, allowing for less morbidity and rapid functional recovery
Keywords: Neurofibroma; Neurofibroma, plexiform; Forearm; Forearm injuries; Surgical wound; Wound healing; Tendon injuries; Acellular dermal matrix.
RESUMO
Introdução: O neurinoma plexiforme gigante é um neuroectoderma e uma doença hereditária. É um tumor cutâneo incomum associado à NF1, caracterizado como um tumor benigno da bainha do nervo periférico envolvendo múltiplos fascículos nervosos. Os objetivos da reconstrução da cobertura do antebraço são proteger as estruturas que vão até o punho e a mão e evitar cicatrizes que levem à perda de movimento. Tanto o antebraço quanto a mão desempenham papéis funcionais e sociais. O manejo bem-sucedido de feridas complexas é necessário para a reabilitação funcional geral desses pacientes.
Relato do Caso: Paciente do sexo feminino, 31 anos, apresentou-se na divisão de cirurgia plástica com neurofibroma plexiforme gigante no antebraço direito. Após ressecção cuidadosa, todos os tendões anteriores do antebraço foram expostos. O defeito foi coberto com Pelnac T enxertável (espessura de 3mm e tamanho 12 X 24cm2), fixados com pontos monocryl 4-0. Após 10 dias, a matriz dérmica acelular foi removida e um enxerto de malha de pele de espessura parcial foi colocado. No dia 7, a matriz dérmica acelular apresentou bons sinais de ingestão. No dia 17, observamos uma sobrevida do enxerto de 95%. No seguimento de 3 meses, a reconstrução estava estável, sem defeitos de contorno, a mão apresentava amplitude de movimento completa e o paciente não apresentava problemas nas atividades diárias.
Conclusões: A matriz dérmica acelular parece ser uma opção útil na cobertura de defeitos complexos no antebraço, permitindo menor morbidade e rápida recuperação funcional.
Palavras-chave: Neurofibroma; Neurofibroma plexiforme; Antebraço; Lesões no antebraço; Ferida cirúrgica; Cicatrização de feridas; Lesões tendíneas; Matriz dérmica acelular
INTRODUCTION
Plexiform neurofibroma is a benign peripheral nerve sheath tumor surrounding multiple nervous fascicles. It usually is present at birth and often becomes physically apparent within the first 2-5 years of life, generating morbidity and cosmetic problems. Despite being considered an uncommon skin tumor, the plexiform neurofibroma is the most often congenital tumor associated with NF1 and has a 2%-5% chance of transformation to malignant peripheral nerve sheath tumors in this setting1-3.
Forearm and hand damage impairs its functional and social role. Successful management of complex wounds is necessary for the overall rehabilitation of these patients4,5. The goals of forearm coverage reconstruction are to protect the structures running to the wrist and hand and prevent scarring that leads to movement loss. Therefore, it promotes patients’ functional mobility of the whole limb and lets them return to work and resume their life6.
The lack of muscular layers on the arm’s anterior surface makes coverage of tendons challenging and may require pedicle or free flaps for treatment. Each technique’s advantages and disadvantages in the management of complex wounds must be taken into account before deciding the treatment option. These variables include bulkiness, donor site morbidity, patient discomfort for a long time and unfavorable cosmetic and functional results5,6.
The introduction of advanced wound care technologies, including negative pressure wound therapy (NPWT) and bioengineered tissues such as acellular dermal matrices (ADMs), has reduced the need for complex surgical procedures with the right indication7-10.
The Pelnac™ (Gunze Co., Ltd., Kyoto, Japan) is an ADM with a bilayer dermal substitute, which consists of the underlying atelocollagen matrix layer acting as a scaffold for dermal regeneration the overlying semipermeable silicone layer acting as a temporary epidermis11.
The application of Pelnac™ for the treatment of forearm injuries involving tendons has not been extensively studied, though the ongoing literature suggests it is a powerful tool for treating such cases11.
OBJECTIVE
We present our experience using ADM for coverage of a large forearm defect. We discuss its advantages and possible drawbacks.
CASE REPORT
The patient signed an informed consent form, and the research followed the Helsinki principles.
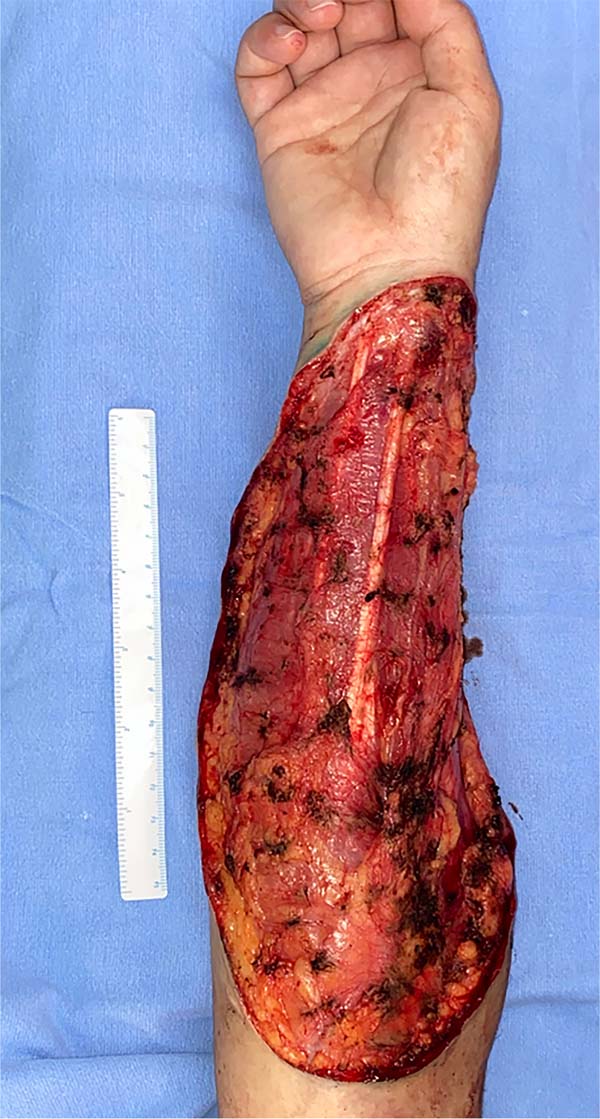
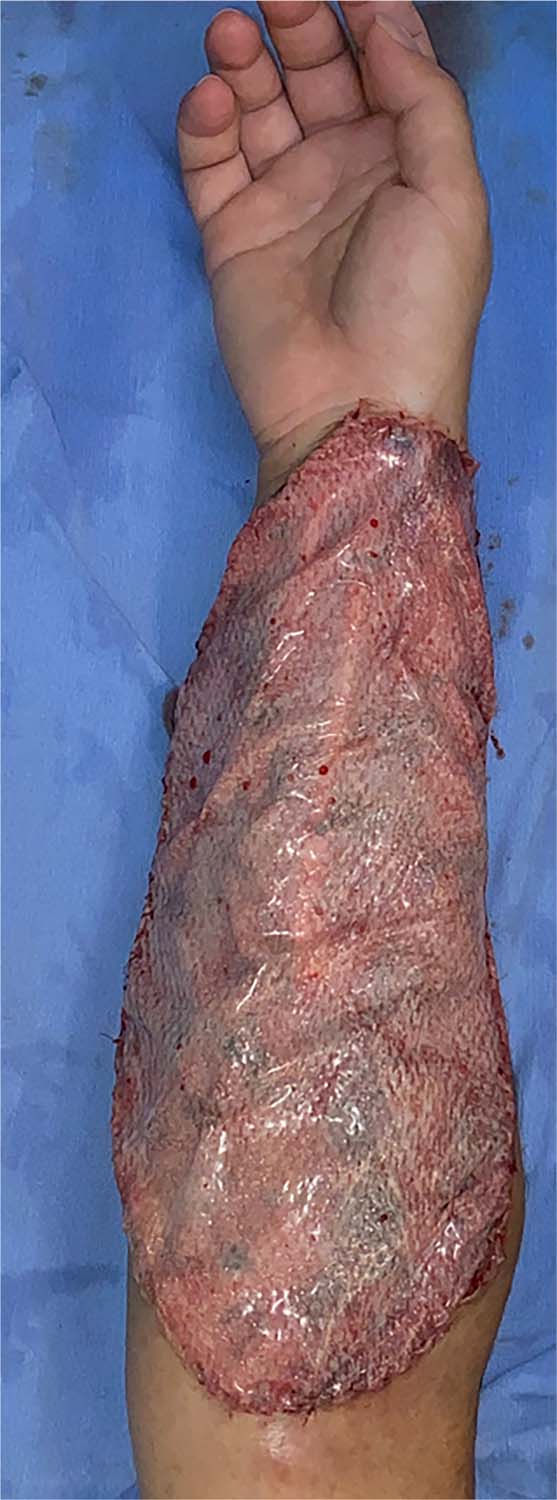
A 31-year-old woman presented to the plastic surgery division with a giant plexiform neurofibroma on the right forearm (Figure 1). She had a past medical history for tetralogy of Fallot, corrected surgically, and neurofibromatosis. The forearm tendons were exposed after careful resection (Figure 2), the forearm tendons were exposed (Figure 3). The defect was then covered with graftable Pelnac™ with 3mm thickness and 12 X 24cm2, fixed with 4-0 monocryl sutures. Small punctures were made into the overlying silicon layer to facilitate effusion drainage (Figure 4). Dressings were made with Jelonet™ and occlusive bandages. Changing was made every 48 hours. After 10 days, the ADM silicone layer was removed, and a fenestrated autologous thin split-thickness skin graft (STSG) was harvested from the thigh region and then placed on the ADM sutured with 4-0 monocryl. The same previously described dressings were made and kept for 7 days.
On day 7, the ADM showed good signs of engraftment (Figure 5). On day 17, we observed a 95% graft take; some debris was removed without any signs of hematoma, seroma, or infection. Intense physical therapy and abundant local hydration were started and performed for 3 months.
At the 3-month follow-up, the reconstruction was stable without contouring defects. The Vancouver Scar Scale score was 3, the hand had a full range of motion, and the patient had no problems in her daily activities (Figure 6).
DISCUSSION
Giant plexiform neurinoma is a benign disease, but it may compromise large areas. Before its excision, reconstruction concerns and options should be considered to avoid transoperative pitfalls.
Most peripheral neurofibromas are solitary lesions. The presence of large, plexiform or multiple neurofibromas is rare, with a limited number of reported cases of lesions with such dimensions and localization. The management of patients with plexiform neurofibroma is not well defined; it is traditionally focused on relieving the symptoms1. Surgical excision of the lesions is the only therapy available to this date. However, the results can be poor, and the procedures can be complicated due to several variables such as size, localization, vascular and neural involvement, the microscopic extension of the tumor and the high rate of tumor re-growth3,12.
Traditionally, flap reconstruction has been the primary treatment option for extensive tendon exposure on the forearm. Nevertheless, it has a variable success rate in some studies regarding flap viability and donor site morbidity. Furthermore, flaps may be limited by the magnitude of the defect and restricted donor sites, especially in patients with significant comorbidities.
ADM has become a popular alternative method in recent years and was reported to provide favorable outcomes in various causes11,13-15. ADM combined with STGS has resulted in encouraging outcomes in treating wounds in terms of scar quality, aesthetic appearance, functional recovery and donor site morbidity16. Pelnac™ is a type of ADM that allows dermis-like tissue growth into a matrix layer and vascularization over areas of exposed tendons, providing a powerful alternative for the reconstruction of these defects.
Compared to the traditional autologous skin flap transplantation, Pelnac™ combined with autologous split-thickness skin grafting more likely resulted in a favorable clinical outcome in treating hand complex wounds in terms of scar quality (VSS), aesthetic appearance, functional recovery and donor site morbidity17. Comparing ADMs in mice, despite some differences in the granulation tissue thickness, inflammatory response, and blood vessel density, is similar in wounds treated with Pelnac and other ADMs. This data suggests that dermal substitutes have a similarly favorable biological behavior and could be successfully implanted18.
A clean wound is mandatory for a successful procedure. Any devitalized tissue would potentially cause infection and failure of the wound repair. Small stabs into the overlying silicon layer to facilitate drainage of effusion, as performed in this case, are described in the ongoing literature to diminish the infection risk. In cases with suspected contaminated wounds, NPWT can be utilized to allow ADM to integrate11.
On every dressing change, the transparent silicone layer allows adequate monitoring of vascularization status and development of potential complications such as infection, hematoma, or seroma.
The main disadvantage of ADMs, such as the Pelnac™, is the high cost, risk of infection, and the need for at least two procedures in most of the ADMs available (although it could be done at once with second-generation matrices)16. Techniques should always be compared scientifically to help aid medical decision19.
CONCLUSION
ADM appears to be a useful option in covering complex defects in the forearm, allowing for less morbidity and rapid functional recovery.
REFERENCES
1. Rallis E, Ragiadakou D. Giant plexiform neurofibroma in a patient with neurofibromatosis type I. Dermatol Online J. 2009;15(5):7.
2. Ross AL, Panthaki Z, Levi AD. Surgical management of a giant plexiform neurofibroma of the lower extremity. World Neurosurg. 2011;75(5-6):754-7.
3. Oruç M, Gürsoy K, Yıldız K, Süngü N, Koçer U. Giant plexiform neurofibroma of the upper limb and anterior chest wall: case report and review of the literature. Eur J Plast Surg. 2015;38(4):323-6.
4. Cho EH, Shammas RL, Carney MJ, Weissler JM, Bauder AR, Glener AD, et al. Muscle versus fasciocutaneous free flaps in lower extremity traumatic reconstruction: a multicenter outcomes analysis. Plast Reconstr Surg. 2018;141(1):191-9.
5. Nelson JA, Fischer JP, Brazio PS, Kovach SJ, Rosson GD, Rad AN. A review of propeller flaps for distal lower extremity soft tissue reconstruction: is flap loss too high? Microsurgery. 2013;33(7):578-86.
6. Browne EZ, Pederson WC. Skin grafts and skin flaps. In: Green DP, Hotchkiss RN, Pederson WC, Wolfe SW, eds. Green’s Operative Hand Surgery. 5th ed. Philadelphia: Elsevier/Churchill Livingstone; 2005. p. 1629-48.
7. Llanos S, Danilla S, Barraza C, Armijo E, Piñeros JL, Quintas M, et al. Effectiveness of negative pressure closure in the integration of split thickness skin grafts: a randomized, double-masked, controlled trial. Ann Surg. 2006;244(5):700-5. DOI: 10.1097/01.sla.0000217745.56657.e5
8. Yonehiro L, Burleson G, Sauer V. Use of a new acellular dermal matrix for treatment of non- healing wounds in the lower extremities of patients with diabetes. Wounds. 2013;25:340-4.
9. Winters CL, Brigido SA, Liden BA, Simmons M, Hartman JF, Wright ML. A multicenter study involving the use of a human acellular dermal regenerative tissue matrix for the treatment of diabetic lower extremity wounds. Adv Skin Wound Care. 2008;21(8):375-81.
10. Randall KL, Booth BA, Miller AJ, Russell CB, Laughlin RT. Use of an acellular regenerative tissue matrix in combination with vacuum-assisted closure therapy for treatment of a diabetic foot wound. J Foot Ankle Surg. 2008;47(5):430-3.
11. Lv Z, Yu L, Wang Q, Jia R, Ding W, Shen Y. The use of dermal regeneration template for treatment of complex wound with bone/tendon exposed at the forearm and hand, a prospective cohort study. Medicine (Baltimore). 2019;98(44):e17726.
12. Liu S, Zhou X, Song A, Huo Z, Wang Y, Liu Y. Giant plexiform neurofibroma of thigh in a young woman. Postgrad Med J. 2019;95(1126):459-60.
13. Haslik W, Kamolz LP, Manna F, Hladik M, Rath T, Frey M. Management of full-thickness skin defects in the hand and wrist region: first long-term experiences with the dermal matrix Matriderm. J Plast Reconstr Aesthet Surg. 2010;63(2):360-4.
14. Gan M, Suzuki S, Moriue T, Igawa HH. Combined treatment using artificial dermis and basic fibroblast growth factor (bFGF) for intractable fingertip ulcers caused by atypical burn injuries. Burns 2005;31(4):514-7.
15. Chen X, Chen H, Zhang G. Management of wounds with exposed bone structures using an artificial dermis and skin grafting technique. Clin Plast Surg. 2012;39(1):69-75.
16. Melandri D, Marongiu F, Carboni A, Rubino C, Razzano S, Purpura V, et al. A New Human- Derived Acellular Dermal Matrix for 1-Stage Coverage of Exposed Tendons in the Foot. Int J Low Extrem Wounds. 2020;19(1):78-85.
17. Wei B, Feng YG, Zhang X. The effectiveness of artificial dermis for repairment of full-thickness defect of the hand. Chin J Hand Surg. 2016;32:145-6.
18. Wosgrau AC, Jeremias TS, Leonardi DF, Pereima MJ, Di Giunta G, Trentin AG. Comparative experimental study of wound healing in mice: Pelnac versus Integra. PLoS One. 2015;10(3):e0120322. DOI: 10.1371/journal.pone.0120322
19. Zanin EM, Maximiliano J, Oliveira ACP, Arpini NE, Duarte DW, Portinho CP, et al. Otoplasty: Rasps or Puncture Needles? A Clinical Trial. Aesthetic Plast Surg. 2021;45(2):521-7.
1. Hospital de Clínicas de Porto Alegre, Department of Plastic Surgery, Porto Alegre,
RS, Brazil.
2. Universidade de Passo Fundo, Faculdade de Medicina, Passo Fundo, RS, Brazil.
| COLLABORATIONS | |
|---|---|
| EMZ | Analysis and/or data interpretation, Conception and design study, Conceptualization, Data Curation, Final manuscript approval, Formal Analysis, Funding Acquisition, Investigation, Methodology, Project Administration, Realization of operations and/or trials, Resources, Software, Supervision, Validation, Visualization, Writing - Original Draft Preparation, Writing - Review & Editing |
| DWD | Analysis and/or data interpretation, Conception and design study, Conceptualization, Data Curation, Final manuscript approval, Formal Analysis, Funding Acquisition, Investigation, Methodology, Project Administration, Realization of operations and/or trials, Resources, Software, Supervision, Validation, Visualization, Writing - Original Draft Preparation, Writing - Review & Editing |
| CPP | Analysis and/or data interpretation, Conception and design study, Conceptualization, Data Curation, Final manuscript approval, Formal Analysis, Funding Acquisition, Investigation, Methodology, Project Administration, Realization of operations and/or trials, Resources, Software, Supervision, Validation, Visualization, Writing - Original Draft Preparation, Writing - Review & Editing |
| NEA | Writing - Original Draft Preparation, Writing - Review & Editing |
| MJZ | Analysis and/or data interpretation, Conception and design study, Conceptualization, Data Curation, Final manuscript approval, Formal Analysis, Funding Acquisition, Investigation, Methodology, Project Administration, Realization of operations and/or trials, Resources, Software, Supervision, Validation, Visualization, Writing - Original Draft Preparation, Writing - Review & Editing |
| JM | Analysis and/or data interpretation, Conception and design study, Conceptualization, Data Curation, Final manuscript approval, Formal Analysis, Funding Acquisition, Investigation, Methodology, Project Administration, Realization of operations and/or trials, Resources, Software, Supervision, Validation, Visualization, Writing - Original Draft Preparation, Writing - Review & Editing |
| ACPO | Analysis and/or data interpretation, Conception and design study, Conceptualization, Data Curation, Final manuscript approval, Formal Analysis, Funding Acquisition, Investigation, Methodology, Project Administration, Realization of operations and/or trials, Resources, Software, Supervision, Validation, Visualization, Writing - Original Draft Preparation, Writing - Review & Editing |
| MVMC | Analysis and/or data interpretation, Conception and design study, Conceptualization, Data Curation, Final manuscript approval, Formal Analysis, Funding Acquisition, Investigation, Methodology, Project Administration, Realization of operations and/or trials, Resources, Software, Supervision, Validation, Visualization, Writing - Original Draft Preparation, Writing - Review & Editing |
Corresponding author: Eduardo Madalosso Zanin, Rua Ramiro Barcelos, 2350, Porto Alegre, RS, Brazil, Zip Code 90035-007, E-mail: eduardo.zanin@gmail.com
Article received: August 23, 2020.
Article accepted: April 23, 2021.
Conflitos de interesse: não há.














 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter