

Original Article - Year 2022 - Volume 37 -
Gluteoplasty with fat grafting: experience in 137 patients
Gluteoplastia com enxerto de gordura: experiência em 137 pacientes
ABSTRACT
Introduction: The concept of female aesthetics has been changing, strongly influenced by cultural and regional patterns. Buttocks and breasts are the main regions emphasized, especially in Latin America. Then, gluteal fat grafting becomes increasingly important. In this article, we aim to study the results of this procedure and its complications, suggest a classification of the shape of the buttocks and standardize areas to be treated with fat grafting.
Methods: This is a prospective study realized from January 2018 to February 2020, and there was a follow-up of the patients for 6 months of postoperative. The surgical technique was tumescent to get fat, and decantation was the method to prepare the graft, which was injected through the intergluteal and subgluteal folds.
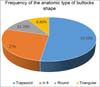
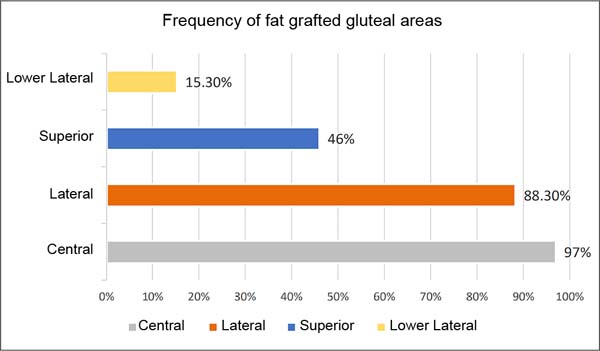
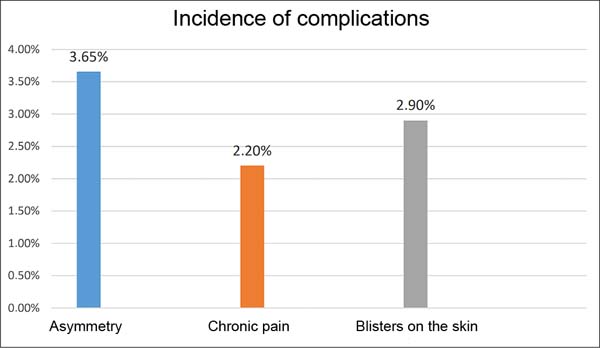
Results: Of 146 patients, nine were excluded, remaining 137, of which 132 were women, and four were men. The mean age of patients was 34.1 years, and the mean body mass index was 27.2Kg/m2. The predominant gluteal shape was the trapezoid (52.5%), and the average volume of fat injected into the buttocks was 510.8ml on the right side and 580.5ml on the left, with the central and lateral gluteal areas being the most grafted. As for complications, asymmetry occurred in 3.65% of patients, skin blister in 2.9% and chronic pain in 2.2% of them.
Conclusion: It is a safe procedure with a low incidence of complication when the fat grafting respects the subcutaneous plane, and this procedure has high patient satisfaction.
Keywords: Lipectomy; Buttocks; Esthetics; Reconstructive surgical procedures; Subcutaneous fat.
RESUMO
Introdução: O conceito da estética feminina vem apresentando mudanças, com forte influência dos padrões culturais e regionais. Glúteos e mamas são as principais regiões enfatizadas, principalmente na América Latina. Diante disto, a lipoenxertia glútea adquire uma importância crescente. Neste trabalho, objetivamos estudar os resultados deste procedimento e suas complicações, sugerir uma classificação do formato dos glúteos e padronização de áreas a serem tratadas com a lipoenxertia.
Métodos: Trata-se de um estudo prospectivo, realizado de janeiro de 2018 a fevereiro de 2020, com seguimento pós-operatório mínimo de 6 meses. Foi utilizada a técnica tumescente para obtenção da gordura, tratada por decantação, e injetada com seringa e cânula via sulco interglúteo e sulco subglúteo.
Resultados: Dos 146 pacientes, nove foram excluídos, restando 137, sendo 132 mulheres e cinco homens. A idade média dos pacientes foi de 34,1 anos e o índice de massa corporal médio foi de 27,2Kg/m2. O formato de glúteo predominante foi o trapezoide (52,5%) e o volume médio de gordura injetado nos glúteos foi de 510,8ml no lado direito e 580,5ml no esquerdo, sendo as áreas central e lateral do glúteo as mais enxertadas. Quanto às complicações, a assimetria ocorreu em 3,65% dos pacientes, bolhas na pele em 2,9% e dor crônica em 2,2% deles.
Conclusão: É um procedimento seguro com baixa incidência de complicações, quando é respeitada a restrição ao subcutâneo como plano de lipoenxertia, e de alta satisfação para os pacientes. A classificação e padronização sugeridas podem auxiliar a aprendizagem do procedimento.
Palavras-chave: Lipectomia; Nádegas; Estética; Procedimentos cirúrgicos reconstrutivos; Gordura subcutânea
INTRODUCTION
Bone structure and the genetic tendency of adipose tissue deposition will define body shape characteristics, with those with wider hips and greater deposition of fat in the gluteal-trochanteric region being more cinched.
Aesthetic patterns of female body contour tend to vary over time, following cultural trends and regional factors, which can be corroborated through sculptures, paintings, magazines, and social media 1. The waist/hip ratio measurement of close to 0.7 has been considered good for the female body shape.
Nowadays, the buttocks and breasts are the main prominent regions, especially in Latin America, where there is a strong media appeal for the ideal gluteal, which explains the increase in the search for gluteoplasty procedures in Brazil in recent years1,2. According to statistics from The International Society of Plastic Surgery (ISAPS), in 2013, just under 10,000 gluteoplasty procedures with fat grafting were performed per year3. This procedure has increased over the years, and in 2018 it reached close to 25,000 procedures per year4.
The desire for a body contour with a small waist, contrasting with the more voluminous gluteal region, has made many women seek this type of beauty standard5 . Liposuction is essential to reduce the waist and still provides the fat to model the buttocks. Gluteal fat grafting consists of aspirating fat from different body regions and inserting it into the buttocks. It is a procedure that uses an autologous, safe biological product with predictable results6.
Compared to other procedures to add volume to the buttocks, such as silicone implants and injection of permanent alloplastic materials, such as polymethylmethacrylate, fat grafting has a lower incidence of complications7,8. Nevertheless, gluteal fat grafting can also present serious complications in the attempt to inject large volumes due to the possibility of causing fat embolism and even death9,10. To avoid them, The Aesthetic Surgery Education and Research Foundation (ASERF) emphasizes some precautions that must be respected, such as: avoiding injecting fat into the muscle; using more caliber cannulas when injecting, such as the 4mm with only one hole; direct the cannula to the most superficial tissues and inject the fat with the cannula in motion11.
Following these guidelines, gluteal fat grafting becomes an important procedure in the treatment of body contouring, with a low incidence of complications, as evidenced in a meta-analysis study carried out in 2016 by Alexandra Condé-Green and collaborators, comprising 4,105 patients from 19 articles selected, which found an incidence of 6.7% of minor complications and 0.32% of major complications12.
Surgery composed of gluteal augmentation, using fat grafting and silicone gluteal implants, as proposed by Aslani & Del Vecchio13, is an option that can improve gluteoplasty results and reduce complications, but studies are still lacking better conclusions.
OBJECTIVE
This article has the general objective of evaluating the results of gluteal fat grafting and specific objectives of determining the incidence of complications, the average volume of fat grafted on each gluteal, the anatomical pattern of the glutes, creating a classification to facilitate the teaching and learning of which areas to be grafted according to the anatomy of each buttock and the degree of patient satisfaction.
METHODS
This is a prospective study carried out from January 2018 to February 2020, with a minimum follow-up of 6 months postoperatively. The patients underwent surgery from January 2018 to August 2019, and the evaluations took place from July 2018 to February 2020. The variables evaluated were age, sex, anatomical classification of the buttocks, gluteal areas fat grafted, volumes of fat used, patient satisfaction and complications.
Inclusion criteria for the study were patients aged between 18 and 60 years, undergoing liposuction and fat grafting in the buttocks.
Exclusion criteria for the study were patients who refused to participate in the study and patients who could not be followed up to the sixth month.
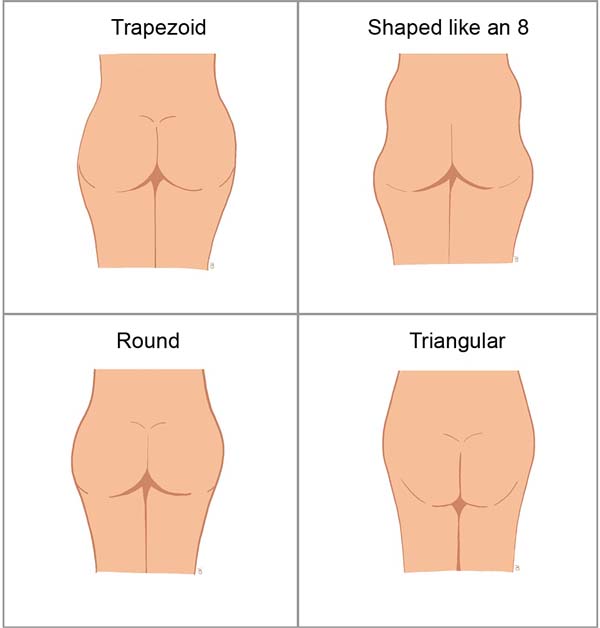
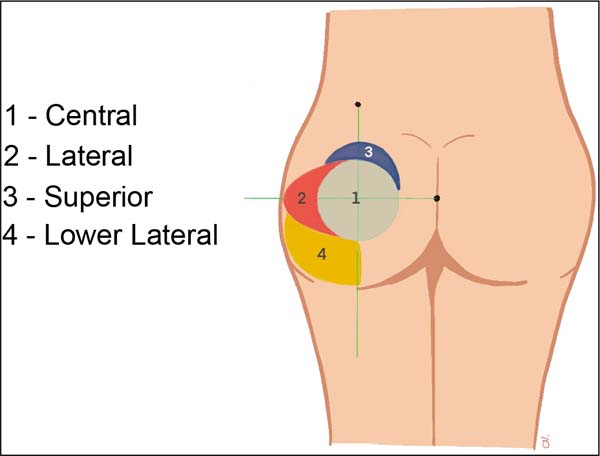
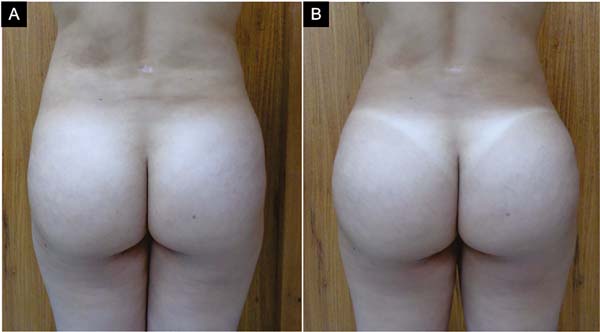
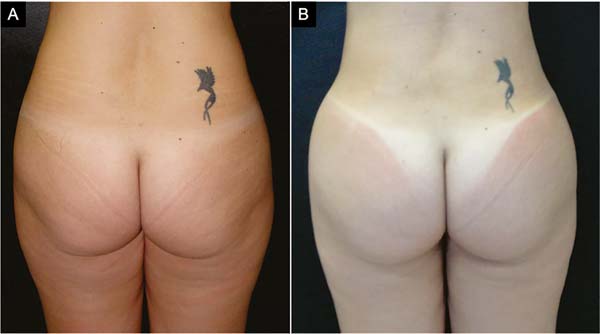
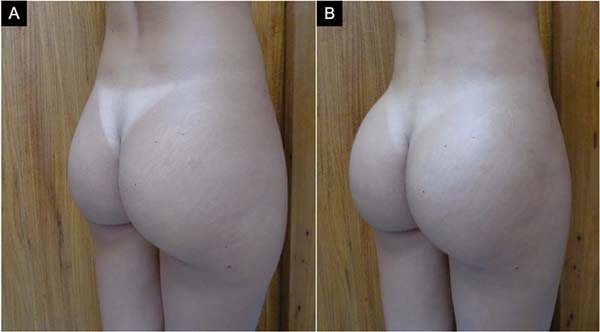
The region’s planning to be fat grafted was programmed according to the anatomical type of the patient’s buttocks (Chart 1 and Figures 1 to 7), with liposuction always being performed on the flanks. Other areas were liposuctioned as needed. The division of the gluteal areas to receive the graft was made according to Figure 2 and mentioned in Chart 1.
| Buttock shape type | Anatomical feature of the gluteus in the posterior view of the body silhouette | Areas to be fat grafted |
| Trapezoid | Two prominent points in the lateral projection, one in the upper portion and one in the lower portion of the gluteus, without depression in the middle. | Area 1- central Area 2- side Area 3- upper |
| Shaped like an 8 | Two prominent points in the lateral projection, one in the upper portion and one in the lower portion of the gluteus, with depression in the middle. | Area 1- central Area 2- side |
| Round | Only a prominent point in the lateral projection is in the middle of the gluteus. | Area 1- central Area 3- superior |
| Triangular | Only a prominent point in the lateral projection is in the upper portion of the gluteus. | Area 4- inferolateral |
The surgeries were performed in a private hospital on patients of the first author. The research was approved by the Research Ethics Committee, with a certificate of presentation of ethical appreciation number 48417821.6.0000.0018 and opinion number 4,877,284. Three patients did not accept participating in the study, and 146 accepted and signed the Free and Informed Consent Form.
The tumescent technique was used to obtain the fat, infiltrating the area liposuctioned with saline solution with adrenaline 1:500,000, with a 60ml syringe and a 3mm Klein cannula. Aspiration was performed with an Allcap® lipoaspirator, the pressure of -600mmHg, an intermediate sterilized bottle to collect the fat, and cannulas with three aligned holes, 3.5 and 4.0mm in diameter.
Fat preparation was performed by decanting in 60ml syringes for 10 minutes (Figure 8). We do not wash or strain the fat.
The fat injection was via the intergluteal sulcus and subgluteal sulcus using a 4mm cannula with three aligned holes and a 60ml syringe in retroinjection, with the cannula in motion, injecting 15 to 20ml per pass of the cannula, in the subcutaneous plane, starting through the deepest part and then injecting more superficially, trying to make a fan distribution (Figure 9). In the end, a massage was performed to model and regularize the skin surface.
In the postoperative care, antimicrobial prophylaxis was performed with cefazolin, 01g every 8 hours, for 24 hours and azithromycin, 500mg a day, for 5 days. In procedures with fat grafting not associated with other surgeries, patients were instructed to remain in the prone position (preferred) for 15 days. In liposculpture combined with abdominoplasties, mammaplasties and/or nose, the patients were instructed to lie supine in the postoperative period. In the first two weeks, massage or lymphatic drainage was not performed in the fat grafted regions.
After the sixth postoperative month, the result evaluation was performed following the 5-point Likert scale (1=poor, 2=fair, 3=good, 4=very good and 5=excellent).
RESULTS
A total of 146 patients participated in the study, but it was not possible to follow up until the sixth month in nine cases, and they were excluded. Of the 137 patients in the final sample group, 132 were women and 5 men. They were aged between 18 and 54 years (mean 34.1 years), and the patients’ body mass index (BMI) ranged from 22.6 to 29.8 kg/m2 (average 27.2Kg/m2);
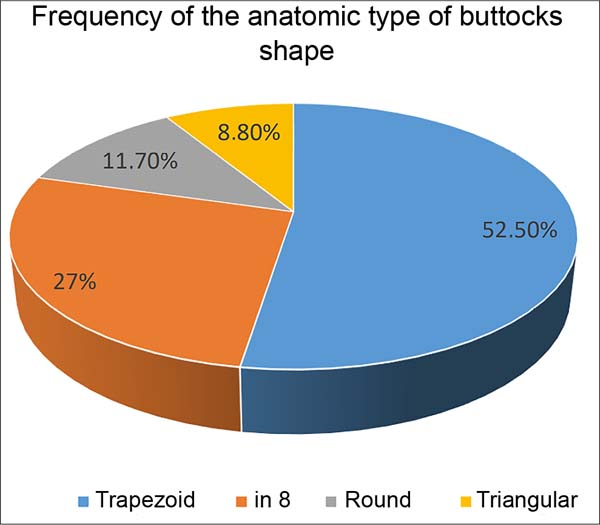
The predominant anatomical pattern was trapezoid (52.5%), followed by figure-8 (27%), round (11.7%) and triangular (8.8%) (Figure 10).
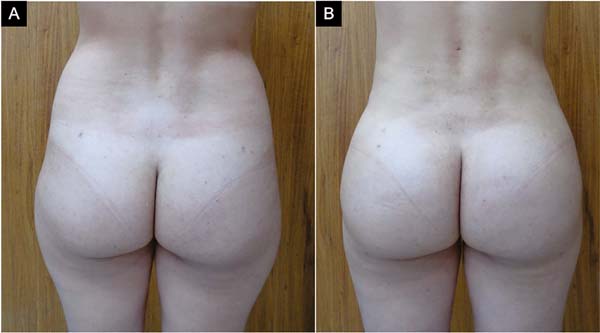
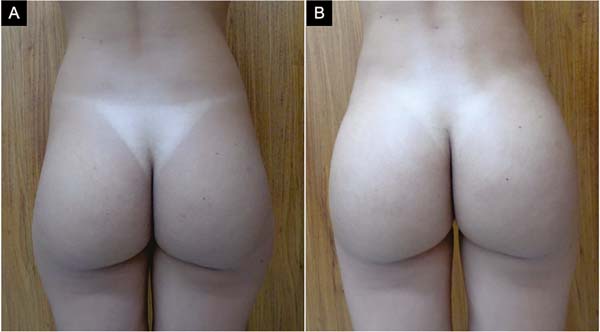
The volume of fat injected into the buttocks ranged from 240ml to 1000ml per buttock, with averages of 510.8ml in the right buttock and 580.5ml in the left buttock. Only 30.65% of the patients had symmetrical buttocks in the preoperative period.
As for the donor areas (in some cases, there was more than one donor area), the waist (flanks and lumbar region) was used in all 137 patients (100%), the side of the thighs (culottes) was included in 108 cases (78, 8%) and the inner thighs in 95 of them (69.3%).
The fat grafted areas (in most cases, more than one area was grafted) were: 1- central, in 133 patients (97%); 2- lateral, in 121 of the cases (88.3%); 3- superior, in 63 patients (46%); and 4- inferolateral, in 21 cases (15.3%) (Figure 11).
We had 12 (8.75%) minor complications (Figure 12) and no major complications. No fat necrosis, seroma, infection, or fat embolism was observed.
The evaluation of satisfaction obtained by patients was described as excellent in 56.2% and very good in 40.9% of cases (Figure 13).
DISCUSSION
The first gluteoplasty procedure was published in 1969 by Bartels, in which the author used breast implants in the gluteus for reconstruction14. With the advancement of liposuction, a new alternative to gluteoplasty emerged, fat grafting15,16.
Gluteoplasty surgeries have become more frequent over the years due to the demand for patients who want to increase the gluteal region, thus obtaining a better body contour12,17. Therefore, gluteal fat grafting has become an increasingly important procedure due to its great demand and good results without using alloplastic materials12,18.
In the present study, the mean age was 34.1 years, and 96.35% of the patients were female, following a similar pattern in other studies2,6,19. The predominant buttock shape was the trapezoid, followed by the figure 8.
The volume of fat injected in most patients was different in each buttock, with the left one receiving more volume, 580.5 ml on average, compared to the average volume grafted on the right side, which was 510.8 ml. In the studies studied, there were no differences in fat injections between the sides of the buttocks, and the fat grafted volumes were like the study by Rosique et al.19, who injected an average of 505 ml in each buttock, as well as in work by Cansancao et al.,6 in which the average volume injected on each side was 521.1 ml.
However, a survey carried out by the same author with 853 Brazilian plastic surgeons showed that 75.65% of them usually inject between 200-399 ml per side, and only 16.71% of them used values of 400-599 ml18.
Infiltration of the donor region using saline with adrenaline, as performed in our study, is the most used according to the review by Condé-Green et al.12, followed by Klein and Ringer lactate solutions with adrenaline. The present study obtained fat with 3.5- and 4.0-mm cannulas through liposuction devices12. The research by Cansancao et al. with Brazilian plastic surgeons had similar results, showing a preference for using liposuction devices and a 4 mm cannula18.
Fat preparation is debatable in the literature, with several techniques reported15,20,21. In this study, we prepared the fat using the decanting technique, which is the most used in several scientific articles, including research with plastic surgeons in Brazil, with fat washing being the second most used technique18. In the review by Condé-Green et al.,12, the decantation was also the most used, followed by centrifugation in second place.
The donor regions of the patients in our study were varied. There was a need for more than one donor area in several patients, and the waist and the lateral region of the thighs were the most used, in agreement with the literature19,22.
Regarding the fat injection planes, we exclusively used the subcutaneous plane, which, after the task force carried out by the Aesthetic Surgery Education and Research Foundation, has been the most used because it is the safest6,11,18.
Fat grafting was performed using 60ml syringes and 4mm cannulas, with three holes aligned at the tip. According to Condé-Green et al.12, only 15% used 4mm cannula, 54.5% of these procedures were performed with 60ml syringes, and only three articles reported the use of cannula with three holes; these data partially agree with our work. We inject 15 to 20 ml of fat for each cannula pass, agreeing with six articles analyzed by Condé-Green et al.12, who reported the injection varying between 0.3 and 20 ml for each cannula passage.
The most grafted areas were: area 1, central, in 97%, is the main one for global gluteal augmentation and to give more projection (Figure 7); area 2, lateral, in 88.3%, serves for modeling, filling the depression at Mendieta’s point C22; area 3, superior, in 46%, serves to stretch the short glutes and when you want a more accentuated curve between the back and the gluteus (Figure 7); area 4, inferolateral, in 15.3%, it is not very common to be grafted, and its use usually occurs in the triangular glutes, to improve their shape, although, in these cases, the expansion capacity of area 4 is more limited, causing a correction, sometimes smaller than desired (Figure 6).
In the present study, only mild complications were observed, such as asymmetry, which affected five patients (3.65%), chronic pain (more than 30 days) in three cases (2.2%) and superficial epidermolysis blisters in four cases. (2.9%). We did not detect any seroma collection, unlike what we found in the articles by Condé-Green et al. and Rosique et al. Its occurrence ranged from 2.4 to 4.7% and is one of the most reported complications in the literature12,19. We emphasize that fat grafting was performed only in the subcutaneous plane, and there were no serious complications such as fat embolism and death. According to the researched literature, these serious complications were more frequent when the graft was performed in the muscular plane9,12. Therefore, we emphasize the importance of the fat graft being placed only in the subcutaneous plane.
In the cases of asymmetries, we emphasize that they already existed in the preoperative period and were not completely corrected with fat grafting. However, they obtained significant improvement. There was no need for additional surgery since the patients were satisfied with the result. In cases of blister formation, these were treated by placing a semipermeable transparent adhesive film dressing (Tegaderm®), which was only removed after absorbing the liquid from the blister. Initially, these areas evolved with dyschromia but responded satisfactorily to the treatment prescribed by the dermatologist. The two cases of chronic pain improved with physical therapy (mobilization and carboxytherapy) and resolved within 4 months.
Regarding patient satisfaction, 97.1% of the result was considered excellent or very good, like the work by Rosique et al.19, whose excellent or very good result was observed in 97% of the cases, as well as in the survey carried out by Condé-Green et al.12, in which, in the studies in which this was evaluated, most of the results were also considered excellent or good.
CONCLUSION
Gluteoplasty with fat grafting is a procedure that provides good results, considered “excellent” or “very good” in 97.1% of cases, with a low incidence of complications, with 8.75% of minor complications, and is more sought after by women in their 30s. at 40 years old. The trapezoid shape of the gluteus is the most frequent anatomical pattern, corresponding to 52.5%, and the central and lateral areas are the most fat grafted, 97% and 88.3%, respectively. The average volume of fat placed in each buttock is between 500 and 600ml, with 580.5ml on the left side and 510.8ml on the right. A classification of the buttocks and standardization of graft areas were defined to help teach this procedure.
REFERENCES
1. de la Peña JA, Rubio OV, Cano JP, Cedillo MC, Garcés MT. History of gluteal augmentation. Clin Plast Surg. 2006;33(3):307-19. PMID: 16818090 DOI: https://doi.org/10.1016/j.cps.2006.04.003
2. Lima DA, Minakami DA, Pereira LC, Grando MC, Cruz RS, Braga AR, et al. Gluteoplastia de aumento: a importância do ensino na formação atual do residente frente à demanda crescente. Rev Bras Cir Plást. 2011;26(1):127-33. DOI: https://doi.org/10.1590/S1983-51752011000100023
3. American Society of Plastic Surgeons. [Internet]. 2013 plastic surgery statistics report. [acesso 2021 Mar 25]. Disponível em: https://www.plasticsurgery.org/documents/News/Statistics/2013/plastic-surgery-statistics-full-report-2013.pdf
4. American Society of Plastic Surgeons. [Internet]. 2018 plastic surgery statistics report. [acesso 2021 Mar 25]. Disponível em: https://www.plasticsurgery.org/documents/News/Statistics/2018/plastic-surgery-statistics-full-report-2018.pdf
5. Singh D. Universal allure of the hourglass figure: an evolutionary theory of female physical attractiveness. Clin Plast Surg. 2006;33(3):359-70. DOI: https://doi.org/10.1016/j.cps.2006.05.007
6. Cansancao AL, Condé-Green A, David JA, Vidigal RA. Subcutaneous-Only Gluteal Fat Grafting: A Prospective Study of the Long-Term Results with Ultrasound Analysis. Plast Reconstr Surg. 2019;143(2):447-51. DOI: https://doi.org/10.1097/prs.0000000000005203
7. Mofid MM, Gonzalez R, de la Peña JA, Mendieta CG, Senderoff DM, Jorjani S. Buttock augmentation with silicone implants: a multicenter survey review of 2226 patients. Plast Reconstr Surg. 2013;131(4):897-901. DOI: 10.1097/PRS.0b013e3182818ec0
8. Kurimori KT, Mendes M, Milcheski DA, Monteiro Junior AA, Gemperli R. Complicação grave do uso irregular do PMMA: relato de caso e a situação brasileira atual. Rev Bras Cir Plást. 2019;34(1):156-62. DOI: 10.5935/2177-1235.2019RBCP0025
9. Cárdenas-Camarena L, Bayter JE, Aguirre-Serrano H, CuencaPardo J. Deaths Caused by Gluteal Lipoinjection: What Are We Doing Wrong? Plast Reconstr Surg. 2015;136(1):58-66. DOI: https://doi.org/10.1097/prs.0000000000001364
10. Toledo LS. Gluteal augmentation with fat grafting: the Brazilian buttock technique: 30 years’ experience. Clin Plast Surg. 2015;42(2):253-61. DOI: https://doi.org/10.1016/j.cps.2014.12.004
11. Mofid MM, Teitelbaum S, Suissa D, Ramirez-Montañana A, Astarita DC, Mendieta C, et al. Report on Mortality from Gluteal Fat Grafting: Recommendations from the ASERF Task Force. Aesthet Surg J. 2017;37(7):796-806. DOI: https://doi.org/10.1093/asj/sjx004
12. Condé-Green A, Kotamarti V, Nini KT, Wey PD, Ahuja NK, Granick MS, et al. Fat Grafting for Gluteal Augmentation: A Systematic Review of the Literature and Meta- Analysis. Plast Reconstr Surg. 2016;138(3):437e-46e. DOI: https://doi.org/10.1097/prs.0000000000002435
13. Aslani A, Del Vecchio DA. Composite Buttock Augmentation: The Next Frontier in Gluteal Aesthetic Surgery. Plast Reconstr Surg. 2019;144(6):1312-21. DOI: 10.1097/PRS.0000000000006244
14. Bartels RJ, O’Malley JE, Douglas WM, Wilson RG. An unusual use of the Cronin breast prosthesis. Plast Reconstr Surg. 1969;44(5):500. PMID: 5345491 DOI: https://doi.org/10.1097/00006534-196944050-00023
15. Oliveira Neto FV. Enxerto de gordura humana em ratos: estudo comparativo de diferentes preparos da gordura. Rev Bras Cir Plást. 2011;26(3 Supl.1):5.
16. Illouz YG. Body contouring by lipolysis: a 5-year experience with over 3000 cases. Plast Reconstr Surg. 1983;72(5):591-7. DOI: https://doi.org/10.1097/00006534-198311000-00001
17. Rodrigues Neto JN, Guimarães GS, Benedik Neto A, Cammarota MC, Daher JC. Prótese glútea: o uso da lipoaspiração na melhora dos resultados. Rev Bras Cir Plást. 2010;25(2):344-8.
18. Cansancao AL, Condé-Green A, Rosique RG, Rosique MJ, Cervantes A. “Brazilian Butt Lift” Performed by Board-Certified Brazilian Plastic Surgeons: Reports of an Expert Opinion Survey. Plast Reconstr Surg. 2019;144(3):601-9. PMID: 31461012 DOI: https://doi.org/10.1097/PRS.0000000000006020
19. Rosique RG, Rosique MJF, De Moraes C. Gluteoplasty with autologous fat tissue: experience with 106 consecutive cases. Plast Reconstr Surg. 2015;135(5):1381-9. DOI: https://doi.org/10.1097/prs.0000000000001167
20. Coleman SR. Structural fat grafting: more than a permanent filler. Plast Reconstr Surg. 2006;118(3 Suppl):108S-20S. DOI: 10.1097/01.prs.0000234610.81672.e7
21. Roberts TL 3rd, Toledo LS, Badin AZ. Augmentation of the buttocks by micro fat grafting. Aesthet Surg J. 2001;21(4):311-9. DOI: https://doi.org/10.1067/maj.2001.117926
22. Mendieta C, Stuzin JM. Gluteal Augmentation and Enhancement of the Female Silhouette: Analysis and Technique. Plast Reconstr Surg. 2018;141(2):306-11. DOI: 10.1097/PRS.0000000000004094
1. Universidade Federal do Pará, Belém, PA, Brazil
2. Hospital Amazônia, Belém, PA, Brazil
3. Spani Vendramin Clinic, Plastic Surgery, Belém, PA, Brazil
FSV Analysis and/or interpretation of data, Statistical analysis, Final approval of the manuscript, Data Collection, Conception and design of the study, Project Management, Methodology, Conducting operations and/or experiments, Writing - Preparation of the original, Writing - Review and Editing.
DASS Analysis and/or interpretation of data, Writing - Review and Editing.
MDSD Analysis and/or interpretation of data, Statistical analysis, Data collection, Writing - Preparation of the original.
LDC Statistical analysis, Data collection, Writing - Preparation of the original.
Corresponding author: Fabiel Spani Vendramin Rua Municipalidade, no 985, sala 2112, Umarizal, Belém, PA, Brazil, Zip Code: 66050-350, E-mail: drfabiel@gmail.com
Article received: April 12, 2021.
Article accepted: October 15, 2021.
Conflicts of interest: none.


















 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter