

Special Article - Year 2022 - Volume 37 -
Legal therapeutic forms for litigation between doctors and patients
Formas terapêuticas jurídicas para o litígio entre médicos e pacientes
ABSTRACT
Highly empowered by knowledge and available information, patients are no longer a passive part of the patient-physician relationship but become more challenging and argumentative about their diagnoses and prescribed therapies. Part of the issues, especially regarding medical complications, may weaken this relationship, a phenomenon that has been described to enhance judiciary litigation against physicians worldwide. With this trajectory, there was a distance in this medical relationship. In this perspective, a wedge has been placed within the patient-physician relationship, delineating on one side a general public more suspicious of the services provided, and on the other side, a more worn-out doctor, with a defensive stance, hyper-specialized and consequently more technical and formalistic than humane and empathic. The reinforcement of medical information and communication between the parts strongly signal what is considered legal prophylaxis in medical services. Even so, complications do occur, and different attitudes do exist in the face of what may have happened. When this happens, one can count on a large legal system called "multi-doors," able to accommodate the necessary contingency, depending on the diagnosis in the relations between the parts, for a legal therapy appropriate to each particular situation. Such "legal therapy" can occur by self-composition, as are the established methods of Mediation and Conciliation, no longer foreign to the health area, or by heterocompositive methods, among which are the already well-known methods of judicial adjudication and Arbitration.
Keywords: Health; Heath/legislation & jurisprudence; Physician-patient relations; Jurisprudence, medical; Arbitration.
RESUMO
Com a maior possibilidade de conhecimento e acesso a informações, o paciente deixa de ser uma parte passiva no relacionamento médico-paciente, sendo a cada dia mais contestador e argumentativo a respeito de seus diagnósticos e terapêuticas instituídas. Parte destes questionamentos, principalmente no que diz respeito a intercorrências médicas, acaba por desgastar esta relação, fenômeno que tem sido descrito como um potencializador na judicialização dos conflitos médicos no mundo. Com esta trajetória, assistiu-se de perto a um afastamento nessa relação médico-paciente, não apenas com um público geral mais desconfiado das prestações de serviços, mas também um médico mais desgastado, com posturas defensivas, hiperespecializado e, consequentemente, mais técnico e formalista do que humano e empático. O reforço na informação médica e na comunicação entre as partes é um sinalizador forte no que se pensa de uma profilaxia jurídica nas prestações de serviços médicos. Ainda assim, intercorrências ocorrem, e posturas diversas existem frente ao ocorrido. Quando isso ocorre, temos hoje a possibilidade de contar com um grande sistema jurídico dito "multiportas", capacitado a abrigar a contingência necessária, a depender do diagnóstico nas relações entre as partes, para uma terapia jurídica adequada a cada situação em particular. Tal "terapêutica jurídica" pode dar-se por autocomposição, como os consagrados métodos de mediação ou conciliação, já não estranhos à área da saúde, ou por métodos heterocompositivos, e, entres estes, a já conhecida tutela Estatal e a Arbitragem, por autonomia da vontade das partes desde que o direito a ser discutido seja disponível.
Palavras-chave: Saúde; Saúde/legislação & jurisprudência; Relações médico-paciente; Jurisprudência médica; Arbitragem.
INTRODUCTION
Controversies of all kinds are submitted to the State Courts, which, overcrowded with cases, overwhelm judges and civil servants, resulting in an extension of time for the analysis and resolution of disputes, which ends up wearing out all the parties involved. Therefore, it is a fact that the so-called alternative methods of conflict resolution, which are the “extrajudicial” ones, such as Mediation and Arbitration, have gained increasing notoriety in Brazil since they were timidly put on the agenda in the mid-1980s.
The issue of civil liability is one of the most complex and extensive in modern Law, and medical malpractice is one of the most serious injuries to the legal good of the human person. Celso Barros Coelho defines that treating them together, establishing interconnections, is a difficult task, as it leads the scholar to investigations in different fields: where the Law operates and where the doctor works1. The physician is liable for subjective liability (guilt) for any material, moral and/or aesthetic damage caused to the patient.
THE DOCTOR AND HIS OBLIGATIONS
Medicine assumes a commitment of means and not of end or guarantee. That is, in civil liability for the provision of medical services, it is understood as an adverse result when the doctor has applied all viable resources and still does not obtain the intended performance or even differentiate it from an unpredictable accident (fortuitous event). At this point, the first obstacle to the term “medical error” used in the media is found, frightening the general public with false judgments of those who go looking for a good and achieve a bad thing. Sometimes, discerning among such events requires refined and technical attention.
Thus, it is worth clarifying the reiterated term “medical error.” Medical error is a media designation of the damage caused to the patient through the action or inaction of the professional service provider without the intention of committing it. There are three possibilities for such an error: imprudence, malpractice and negligence2. In the Doctrine of Law, it is known that these three pieces are bases for the configuration of guilt stricto sensu when talking about Civil Liability1,2. Negligence is said to be omissive, while imprudence and malpractice, commissive.
There is a judicial, and consequently public, understanding that some medical areas are premised on the delivery of results, with an obligation of the end (or guarantee), as is the case of plastic surgery. The issue of obligations in medical and dental services is controversial. According to Marta Maffeis Moreira, it is necessary to understand the contract established between the health professional and the patient, that is, what was the contract of locatio conductio3.
The knowledge of a procedure classified as having only an aesthetic character brings with it the bond of an obligation of result, based on the Consumer Law Code of 19904.
Guzman Mejia5 claims that an effective legal system can hold the physician’s service accountable, provided that it understands the proposed medical therapy and the reasons for such a proposition. In other words, in the specific case of certain practices, how to determine, eliminating the superficiality of the term “aesthetic,” the obligation of the doctor who proposes a procedure, evaluating not only the procedure itself, but also understanding what it proposes to treat.
THE PROSECUTED DOCTOR
From the moment of its citation, and here we speak exclusively of an indemnity process for damage, therefore of Civil jurisdiction, until the final res judicata of the applicable last resort, the physician finds himself in the worst scenario he could have in his doctor-patient relationship and often with the profession.
Regardless of whether guilt exists, doctors are negatively affected. Perhaps, at a time when they have to face human fallibility. And, although not present, the accusation of having failed affects not only their self-image but also their social image6,7.
Medical students and physicians are more likely to have anxiety, depression and suicidal ideation than their peers in the general population. The medical culture perpetuates these problems, being true “barriers” to possible treatments. Some authors have examined myths and symbols that form the basis of medical culture and medical self-image, the latter based on a decontextualized medical mythology, such as the myth of Asclepius8, resulting in an unbalanced, dehumanized sense of professional identity characterized by unattainable expectations. It is a construct of the “medical persona,” which is often sick, stressed, or even toxic9.
The prevalence of burnout in the medical population is significant, especially when considering not only the effects on physicians as individuals but social effects at the time the population that depends on these services and medicine itself as an institution suffer10. There is a high prevalence among these physicians of abuse of alcohol or other legal and illegal drugs, problems in personal relationships, anxiety and depression11,12.
Today, it is known that one of the predictive factors for such a diagnosis in a medical professional is the knowledge that this professional is experiencing legal problems with his patients13. It can also be said that stressed, depressed and sleep-deprived physicians are more exposed to making a mistake in their service delivery, a situation that can perpetuate or exacerbate the burnout diagnosis14,15,16.
A study conducted in the 1980s in Chicago matched a random sample of members of the Chicago Medical Society on the impact of medical malpractice litigation (or the mere prosecution of this event) on physicians’ personal and professional lives. They were divided into two groups: one of the doctors with disagreements that have not been judicialized and the other already litigating in the Judiciary.
The difference in the severity of depressive symptoms present in the second group of physicians was significant, with an “unwillingness” to attend to certain types of patients, such as those related to aesthetic procedures or those with a high-demand profile and who led their doubts to a guarantee of results; other data from this group of doctors, who already had the judicialization of a disagreement in their lives, were their desire for early retirement and the discouragement of their children entering medical schools17. These are situations, concludes the author, that undoubtedly affect the doctor’s professional path, as well as the lives of their families, patients, and the entire provision of medical services18.
US data bring to the years 2007/2008 the impressive proportion of 42% of physicians in the country being legally sued for bad professional practice, without analyzing the merits of the request19, with a higher rate of involvement among surgical specialties and gynecology and obstetrics.
Data from US liability insurers shows that most claims of medical malpractice, malpractice or recklessness are unsubstantiated, with nearly two-thirds of claims being dismissed, withdrawn or dismissed. Of the 10% of claims that progress through the procedural rite until their final decision, almost 90% have their decisions in favor of the doctor20. However, during all the procedural stages, adding to uncertainties and financial expenses, the doctor’s psychosocial involvement is exactly the same as the doctor convicted21.
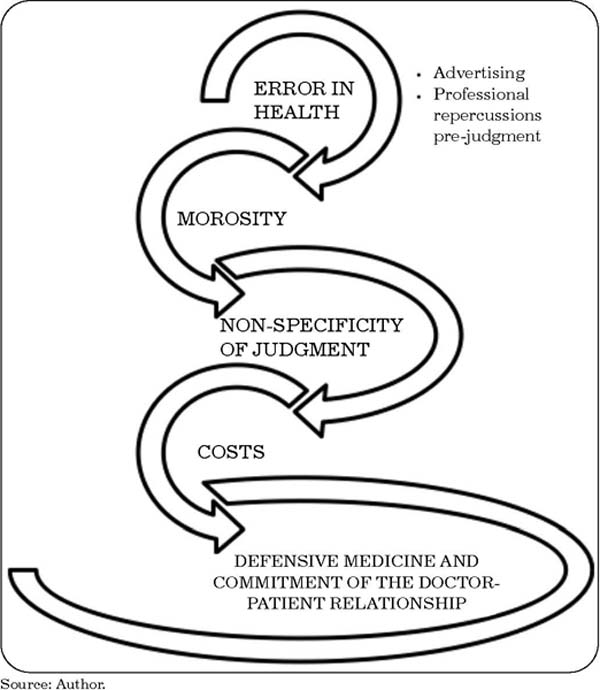
It is true that, specifically for the Brazilian doctor, since a set of rules and regulations valid in the national constituency are being evaluated, there are points that are worth the discussion about “what weighs most in the disputes referred to State protection,” generating this positive feedback for their burnout (Figure 1). Some of these points are listed below from the evident point of view of the physician.
DEFENSIVE MEDICINE AND DOCTOR-PATIENT DISTANCING
Considering the overview of the doctor in the Judiciary, let us take as a step the understanding of some psychosocial consequences adopted by the category and by the insurance industry with coverage in civil liability that surrounds it in the last decades to try to circumvent such judicial events, in the sense of minimizing harm to the medical professional. Would this statement be true?
Despite the great criticism of civil liability insurance coverage or even the suitability of some insurers, perhaps the focus here is on pointing out what this shield, what this supposed protection has contributed to the doctor, the patient and their relationships.
Believing that insurance is a guarantee of repairing the damage committed is to abstract from reality all the humanistic possibilities involved in a medical act. Shielding the professional’s assets is one of the most obvious reasons for contracting civil liability insurance, given the content explained in the downstream item “procedural costs.”
In the legal field, prophylaxis is understood to be what is clearest, for the Law, in the relationship with the patient: the positivization of contracts, not only for the provision of medical services but also the lack of knowledge and understanding of everything that has been said and explained about the diagnosis and recommended treatment plan. The latter is understood to be free and informed consent terms, notifying the patient’s information and the doctor’s safety who, in good faith, provided clarification to what was then understood by the Consumer Code to the hyposufficient party.
The extreme specialization of doctors, technology, and technical and human apparatuses surrounding them contribute to this distance. National and international studies point to the current demand for reversing the deterioration of this relationship22. The authors open similar questions, including the need for government programs and incentives from undergraduate medical education to take care of this distance inherent to our time to medical retraining programs so that professionals do not depend on personal experiences. This must be a social demand.
The physician’s behavioral change is not so recent. Conducted in 2015, a survey of breast pathologists found that more than 80% of them requested testing in response to fears of malpractice, recommended additional surgical sampling or requested more opinions. These defensive practices were attributed as having important implications for health costs and patient safety23.
Another recent national study on the subject concluded that always in the light of ethics, the consequences of defensive medicine and its knowledge on the part of patients tend to make the doctor-patient relationship even more difficult due to the reduction in patient trust concerning the professional. Extending deadlines for diagnosing the health problem to seek a cure and punishing the patient who depends on the Unified Health System substantially increases the cost in public and private spheres. The same study also concludes that the lack of incentives for mediation and conciliation in the hospital area also favors defensive medicine since the doctor would feel more protected if each institution had an internal segment to take care of relationships with patients, something that is not observed worldwide. Of the group investigated, the majority resort to defensive medicine to protect themselves from lawsuits for professional misconduct24,
ANALYSIS FACTORS FOR INDICATION OF LEGAL THERAPY
Publicity
National legal regulations excelled in the Principle of Publicity, which makes all procedural acts public, available for access and consultation, both for the parties and any interested person. However, it is not a full rule since it is established in our Federal Constitution, in its Article 5°, item LX, the possibility of restricting the publicity of procedural acts when the defense of privacy or social interest so required.
The publicity of judicial acts is a fundamental right, which aims to allow the control of public opinion on the services of justice, observing the power that was invested in the judge who, in his function, represents the State. Therefore, there is an intimate relationship between the Principles of publicity and the motivation of judicial decisions, as publicity participates in effectively controlling these decisions. That is, it is a true instrument of effectiveness in guaranteeing the motivation of court decisions25.
The expression “secrecy of justice” is notoriously inappropriate, as it is not a matter of secrecy since the trial does not take place behind closed doors. Rather, care is taken to protect the litigants’ privacy or prevent publicity from causing great inconvenience or social commotion. However, the parties and their attorneys have access to the records, including obtaining certificates. In this sense, when dealing with the matter, the Constitution used a more appropriate expression, namely: restricted publicity26, which occurs in judicial proceedings related to family law and childhood and youth law.
Even though its publicity is restricted, the judicial process guarantees the non-circulation of the case’s contents and its procedural steps; it does not preserve the name of the parties involved in a dispute. And it is at this moment that the doctor, with his name exposed, even though, exceptionally, he has guaranteed secrecy of justice due to confidential data from the medical record, is adrift of public opinion27.
In social networks, what was supposed to be an event becomes a court of Exception, temporarily formed to judge a specific case (or some cases) after the crime has been committed. As a classic example, the Nuremberg Tribunal created by the Allies to try the Nazis for war crimes28.
The danger of this exposure on social networks is the channeling of public opinion, invariably partial in its judgments, even because it is pre-directed according to decisions adopted by this same media court in similar cases.
Slowness
The growing call for judicial protection, with a continuous distribution of facts, added to the state infrastructure deficit to house these actions, and the still low number of magistrates to meet all demands in the national territory attest to the amorousness in the processing of judicial processes, for so long, object of discussion in the doctrine, since it generates legal and social insecurity, with feelings of helplessness and discredit on the part of the jurisdictional parties29.
In her master’s thesis, Simone Oliveira, when understanding the temporal bases of the process, exposes the following question: “In the observance and application of the principle of the reasonable duration of the process, we cannot avoid the following question: reasonable time of the process would be the one foreseen in procedural legislation, or would it be the time needed to resolve the dispute according to its complexity?”29.
In the vast majority of cases, the evidentiary phase of a process involving a medical case depends on specialized expertise that supports the court in conducting the dispute on reasonable terms. At this procedural moment, even though there are rules and determinations of the court related to time, it comes up against insurmountable administrative issues.
As already explained, the need for expert evidence is almost certain in disputes between doctors and patients. The court, based on which party requests this expertise, or even understanding that it is part of the criterion for reversing the burden of proof to the medical party, or even understanding the possible gratuitousness of justice demanded by the patient, decides whether the medical expert summoned and duly registered as an assistant to justice, a professional you trust will be required, or the regional state agency responsible for carrying out medical examinations will be asked to be available to attend to the specific case.
The Institute of Social Medicine and Criminology of São Paulo (IMESC), an autarchy linked to the Secretary of Justice and Citizenship of the Government of the State of São Paulo since 1970, today considered the largest center for Forensic Medicine and Genetic Link Investigation of Latin America, handles demands, through expert appointments with an approximate wait of 8 months for the on-site expert examination, and an average time of delivery of the expert report in another 4 months from the physical examination.
In addition to a structural reform on the part of the State, to ease the stiffening caused by the excess of procedural demands, it is necessary to implement self-compositional means of conflict resolution, such as mediation or conciliation; or even the optimization of part of this high demand through other heterocompositional possibilities, such as the validation of arbitration chambers for the resolution of disputes whose objects are of available rights, a subject to be dealt with in a later chapter.
Specificity of the relationship
From the doctor-patient relationship, which is so specific, litigation could not be expected that would not include all the unique understandings of this bond. From this, the need for specific knowledge of the judge is faced. Therefore, once again, the peculiarity of the relationship and the conflict demand a technical solution that, in the Judiciary, would probably be relegated to expertise and that could better be dealt with, from this point of view, in the arbitration scope or by any autocompositional method.
The judge, a word originated from the Latin iudex, is the one who judges, who says the Law, exercising jurisdiction, being, therefore, an authority invested with power to, saying the Law, resolve the conflicts of interest submitted to it30. However, this judge, endowed with a strong legal basis, is not fully qualified to develop opinions on specific matters related to other professions. And it is in this gap in technical training that an arbitrator or mediator, with a full understanding of the matter, in the case under discussion, medicine, would stand out from the State judge, even if he does not perform the expert function completely differently.
The motivation of the sentence is what makes the judicial decision democratic (the judge is not elected, but, by imposing that he decides based on the established laws and demonstrates having done so, the Judiciary becomes part of a democratic system and non-aristocratic - which is what would only follow from the nomination by competition, among the best). The reasoning of the report and the explicit demonstration that the scientific method was strictly followed is the guarantee that the document is not a mere opinion, prejudice or concept compromised by the ideology, ignorance, or interest of the expert31.
Costs
As a rule, for filing any lawsuit, it is necessary to advance procedural costs by the plaintiff, which are not related to the fees owed to the lawyer for the provision of services. In reality, they are amounts paid directly to the State through cost guides issued by the collection systems, which vary among the entities of the Federation. Some situations alter this circuit of procedural costs, which is the allowance for these if free judicial assistance is granted, at least while the beneficiary party does not have the financial conditions. This happens a lot with the “patient” part here in Brazil.
Obviously, the costs with the legal team are taken into account, not only to whom the party hired, but also, at the time of judgment or final decision, the fees of the attorneys of the opposing party.
However, lately judged, the high indemnity values bring the medical causes to the category of the highest costs observed in the Judiciary. This involves, in most cases, the sum of the material damages caused and moral damages, and in some situations, overlapping the aesthetic damages.
FORMS OF RESOLUTION OF CONFLICTS OUTSIDE THE STATE GUARDIANSHIP
Justiça Multiportas (Multi-Door Justice) is the expression of a new architecture for the protection of rights, composing together with the State protection alternative possibilities of access, several doors, and several justices for a single purpose: the resolution of the conflict. Evidently, the great “atrium” of the Judiciary represents the security of the structure designed for the fundamental rights of individuals and groups, basing the security that the investment in any other dispute resolution system will be valid as long as it is also at the same time, constitutionally appropriate32.
This new adequacy of justice meets the available and unavailable legal situations, individual and collective, between public and private parties, being a distinctive point in the history of accessibility to rights and justice.
Justiça Multiportas is shown in the Civil Code and Process (CPC) by entities known as mediation, conciliation and Arbitration, registered in several passages, with the clear intention of encouraging a new dimension for all those involved with the protection of rights, including the legal operators themselves, from whom cooperation is required, as in the mandatory conciliation and mediation hearing, provided for in Art. 334 of the new regulation32.
The appropriate work method for resolving conflicts must be distinguished from judicial litigation. In the State tutelage, the parties are essential characters, in theory, but, in practice, they do not perform such an effective function except in searching for the merits of the issue in the judicial demand. These act through their lawyers, who invest in technical discourse, and the magistrate, in a retrospective look at the dispute, grant the decision.
MEDIATION AND CONCILIATION
In autocompositional methods, on the other hand, the parties are the effective protagonists of the procedure. The objective, especially of mediation33, gives interested parties the ability to identify the core of disputes and, supposedly, to implement a dialogue. In this vein, we speak of a prospective vision, when in order that skills developed in the course of the proper procedure those parties not only resolve the conflict but are also able to avoid new lawsuits, we look to the future. Of the various guiding principles of our legislation, those of autonomy of will and confidentiality, currently supported by the CPC in its § 3 of Art. 165, flowing on the mediator’s duty to help “the interested parties to understand the issues and interests in conflict so that they can, for the restoration of communication, identify, for themselves, consensual solutions that generate benefits mutual”34.
Conciliation and mediation are two distinct self-composition methods, as the new process code itself indicates:
Art. 165. (...) § 2 “The conciliator, who will act preferably in cases where there is no previous relationship between the parties, may suggest solutions to the dispute, being prohibited the use of any type of constraint or intimidation so that the parties reconcile.”
Art. 165. (...) § 3 “The mediator, who will preferably act in cases where there is a previous relationship between the parties, will help interested parties to understand the issues and interested parties in conflict, so that they can, by reestablishing the communication, identify, by themselves, consensual solutions that generate mutual benefits.”
In mediation or judicial conciliation, the parties must be accompanied by lawyers or public defenders, as provided in § 9 of Art. 334 of CPC/15 and art. 26 of the Mediation Law, except in cases where the lawyer is dismissed, as in the scope of Law 9,099/95.
However, when the procedure is extrajudicial self-composition, the presence of a legal professional is not essential. However, it is worth noting that this professional follow-up is always good manners, as the parties will issue wills and enter into commitments with legal consequences.
In the US states where such possibilities are effective in mediation and arbitration cases, the Courts understand that based on “consent, not coercion” and that “the interpretation of private contracts is normally a matter of State law” causes these Courts not to meet to review them35.
ARBITRATION
The idea that the arbitration process is nothing more than an alternative dispute settlement mechanism has long been overcome. It is an alternative because it still timidly, even today, helps in a limited way the state jurisdictional action. Although born conventionally, it develops concretely in terms of the general theory of the process. It acts and takes place in a procedural environment. But that, in most cases, departs from the state model because it contains instruments that act in a typical way, although with the same stabilization of decisions and the respective pacification of conflicts. And in some situations, more efficiently than in the state sphere. There is greater procedural flexibility compared to the state process. It is said, therefore, that the arbitration process achieves levels of procedural adaptability in degrees very high36.
The autonomy of the will as a presupposition and principle of the arbitration process is a key element of the method: the autonomy of the will, instrumentalized by the arbitration agreement, whether through an arbitration clause or arbitration commitment37.
The agreement of an arbitration clause, due to the autonomy of the will between the parties, is a prerequisite for the arbitration process to exist. Fazzalari sees the convention as a harmful matter, as it has to be appreciated before the merits, subject to the analysis of this38. In contrast, the arbitration commitment takes place during the arbitration process simply because the autonomy of the will is a principle of the arbitration process.
Another element is the need to arbitrate only available rights. Unavailable is the right that is not justly enjoyed, which is inalienable or inalienable. Unavailable are the rights that the person cannot give up, such as the right to life, liberty, health and dignity. A person cannot sell an organ of his body, even though it belongs to him39.
As a matter of principle, health is not very appreciable pecuniarily. Therefore, it is not a heritage asset, as it is not established available. From this perspective, at first, it would be said that there is no arbitrability for its defense, which is not at all the truth.
Although the health path is a non-patrimonial good, the defense of the right to this can contain, first, patrimonial rights and health only appear as a scenario, a background of the conflict. In this way, the right to health is sometimes directly defended. In other cases, defending health implies indirect defense, specifically when the main relationship is economical, obligatory and contractual40. Health is a non-patrimonial and unavailable asset. However, contractual relationships between doctors and patients, health plans and beneficiaries, hospitals and users, among others, establish consideration for the health service, and this contractual-obligatory relationship translates into pecuniary terms41.
It is worth mentioning that there is a hypothesis of the existence of a conflict of an available property nature instituted in Arbitration, and during the process, a controversy of unavailable right arises. Nothing prevents the suspension of proceedings and the referral of the case to the Judiciary so that only after a judicial decision on the non-patrimonial matter is returned to Arbitration, as provided for in Article 25 of Law 9,306/96;
“If in the course of the Arbitration, a dispute about unavailable rights arises, and it is verified that the judgment will depend on its existence or not, the arbitrator or the arbitral tribunal will refer the parties to the competent authority of the Judiciary Power, suspending the arbitration procedure. Sole paragraph. Once the preliminary question has been resolved, and the sentence or judgment has been added to the case file, the Arbitration will proceed as normal.”
SUCH LEGAL THERAPEUTIC FORMS IN HEALTH
The term ADR, for Alternative Dispute Resolution, is commonly used in some countries such as the United States of America (USA) to designate a variety of dispute resolution mechanisms, enabling the fulfillment of a wide variety of social, commercial, legal and political parties, as presented in the comparison between the forms of ADR (mediation and arbitration) and the judicial procedure, as shown in the following table, available at Ribeiro42 (Table 1).
| Objectives of those involved | ADR Mechanism | Procedure | |
|---|---|---|---|
| Mediation | Arbitration | Judicial | |
| Minimize costs | 3 | 1 | 0 |
| Solve quickly | 3 | 1 | 0 |
| Keep privacy | 3 | 3 | 0 |
| Maintain relationships | 3 | 1 | 0 |
| Get neutral opinion | 0 | 3 | 3 |
Caption: 3: highly possible to reach the objective: 2: possible to reach the objective: 1: unlikely to reach the objective: 0: highly unlikely to reach the objective.
Source: Ribeiro WC. Mediation as a means of conflict resolution in the health area. Rev Dir Sanit. 2018;18(3):62-76.42
It is of social interest to create a culture in which not only the individual doctor but a health system does not practice “defensive medicine,” a clear occurrence due to the previously exposed whole, but promotes improvements in their individual and systemic care. For such effectiveness, the system must promote a culture of open and efficient communication between physicians and patients, even after a negative result, regardless of guilt43.
The Lexington, Kentucky, Veterans Affairs (VA) Medical Center was one of the pioneers in this area. In 1987, the Lexington VA implemented a Resolution and Communication Program, which provided full disclosure of the occurrence that resulted in harm, as well as an expression of condolence on behalf of the institution and its clinical staff. Under this system, patients and their families are invited to bring in lawyers to discuss compensation offers at the beginning of the process, which is a milestone for mediation in the North American healthcare sector44.
The mediation process can play a vital role in difficult communications after an adverse medical event. The communication used by the team to calm the emotions of patients and their relatives, the recognition of feelings, active listening and the expression of empathy are important skills to deal with the emotional burden of the injured party. Effective communication after adverse events has been proven to reduce the number of lawsuits against the physicians involved in the case45.
In 2017, a study was published in the Journal of the American Medical Association involving the experiences of a group of 30 patients with the Communication and Resolutions Program in Hospitals in Boston, Massachusetts and California, 18 of whom had a good experience with this communication channel and hospital conflict resolution45.
Non-violent communication, since it represents a strategic means of mediation and its execution, guarantees the re-establishment of social relations based on the process that will search for exchange between the parties to result in consensus46.
Perhaps the two biggest obstacles to mediating medical disputes come from the main players: doctors and lawyers. North American studies on medical mediation show that most mediations take place without the presence of the doctor for many reasons: (i) they do not want to face their patients face to face; (ii) they are very busy in their practices; (iii) they just want to leave it to their insurers to make the deal.
On the other hand, defense attorneys tell doctors not to attend mediation for fear that doctors might be too outspoken and vulnerable to compromise in mediation or fail, and the patient proceeds with litigation. In addition to discouraging doctors from attending mediation, some lawyers do not advocate it for clear economic interests47. A US study showed that a lawyer spent an average of 3.5 hours preparing for mediation and more than 36 hours preparing for a trial48.
The advantages of using Arbitration as a jurisdictional method for doctor-patient disputes are recognized worldwide and a North American practice that has been defended for decades49. Authors highlight the indisputable quality of the decisions made by technical arbitrators in the matter due to the speed of resolution and also, as a consequence, the reduction of procedural expenses50.
In March 2011, the Malpractice-related Damage Relief and Medical Dispute Resolution Act was passed by the National Assembly of South Korea, taking effect one year after its enactment. This Law supports a fair, quick and inexpensive solution to medical disputes, focusing on alternative dispute resolution in malpractice cases, detaching them, if so decided by the parties, from the civil courts51.
Such advantages of precision and efficiency in decisions must work to the benefit of both plaintiffs and defendants.
FINAL CONSIDERATIONS
The many advantages assumed by resolving disputes via Arbitration are still not convincing to the physician, such as the speed of decisions, lower costs and the greater and all-important confidentiality when it comes to medical malpractice claims. First, because the results of related litigation are, in the state jurisdiction, generally very positive for doctors. Of course, physicians understandably refuse to accept a different resolution system when they are not convinced that the results will be equally favorable, much less even better.
Physicians nowadays, and depending on the medical specialty, it becomes an intangible truth; they are usually patrimonially shielded and protected from the costs and expenses of such litigation by Civil Liability insurance. Thus, arguments about reduced arbitration costs are unpersuasive for clinicians.
Third, while disputes can be resolved more quickly with Arbitration than through State relief, other commonly reported advantages of Arbitration - such as the ability to select their decision-maker and the availability of neutrals with specific experience and privacy - may appear illusory for the doctor52.
Just as the legal prophylaxis of this professional relationship must be improved, legal therapy must extend to other possibilities of resolution. It is like in Medicine: if several antibiotics can effectively treat the same disease, you cannot say which is the best course of action for that case. Perhaps here is a comparison with the best experience of that professional for that event.
The best therapy is a sum of the appropriate therapeutic application, for that specific case, according to the experience of the professional able to treat it.
Once these barriers are overcome, self-compositional methods such as Mediation and Conciliation, as well as heterocompositive Arbitration, constitute effective means for the relationship of contractual conflicts between doctors and patients, resolving in a faster, less costly way, and perhaps, why not risk this characteristic, more assertively, given the specificity of the mediators/ arbitrators chosen in the issues involved in each specific case.
IMPRESSIONS AND PERSPECTIVES
The doctor-patient relationship has changed. The proposal to rescue the old formula of this relationship is perhaps wrong. Society dynamically evolves in all its understandings, just as it does in Law, long discussed by Hans Kelsen in his classic Pure Theory of Law. On the other hand, medicine has changed. We evolved with technological, digital devices that allow faster communication at a distance and with the possibility of much more accurate diagnoses. However, as it narrows diagnostic possibilities, all this evolution brings a less passive, more proactive patient and a doctor constrained by conditions that can compromise him: Am I doing the right thing? Am I doing everything I can for local conditions? Am I interpreting correctly? Is this report correct?
Perhaps, given the irrefutable speed and direction in medical technology, the great “secret” lies in communication. However, it is worth remembering that we are talking about and pointing to a modern relationship, informal and formal communication, humanized communication and based on legal prophylaxis, respectively.
Empathy, putting yourself in the patient’s and family’s shoes, treating them with information with respect and consideration, as with any loved one, helps a lot in understanding, not only in the way of following up the patient who has suffered an intercurrence, but it is fundamental in cases where discord is already established on the part of the patient, being a basic principle of Mediation.
Self-compositional methods have been present in the medical profession for years, even proposed by the Regional Councils of Medicine, with some ease, but there is still much to be stimulated in these methods. Perhaps the greatest barrier is the culture of immediate judicialization on the part of the patient, stimulated by a contentious legal class, without the attempt of medical re-approach before a formalized litigation.
Arbitration and its established laws fit perfectly into contractual disputes between physician and patient, as seen. However, the consumerist code limits the method, and the hyposufficient pole must be very aware and in agreement, showing itself to decide to opt for the proposed judicial route. The marketing of this method becomes rigorously necessary for a broad social understanding of its structure and its full validity and effectiveness.
REFERENCES
1. Tartuce F. Manual de Direito Civil. 8ª ed. Rio de Janeiro: Forense; 2018. 538 p.
2. Lima A. Culpa e risco. 2ª ed. São Paulo: Revista dos Tribunais; 1999.
3. Moreira MRM. Contribuição ao estudo da responsabilidade civil do médico à luz do direito romano. São Paulo: Quartier Latin; 2016. 181 p.
4. Brasil. Senado Federal. Lei No. 8.078, de 11 de setembro de 1990. Código de Defesa do Consumidor. Dispõe sobre a proteção do consumidor e dá outras providências. Brasília: Senado Federal; 1990.
5. Guzman Mejia JI. Ante la mala praxis quirúrgica, ¿trascendencia ética o legal? Cir Gen. 2018;40(1):46-53.
6. Wu AW. Medical error: the second victim. West J Med. 2000;172(6):358-9. PMID: 10854367 DOI: https://doi.org/10.1136/ewjm.172.6.358
7. Crigger NJ. Always having to say you’re sorry: an ethical response to making mistakes in professional practice. Nurs Ethics. 2004;11(6):568-76. PMID: 15597937 DOI: https://doi.org/10.1191/0969733004ne739oa
8. King KC, Hoffman JR. Myths and medicine. West J Med. 2000;172(3):208. PMID: 10734817 DOI: https://doi.org/10.1136/ewjm.172.3.208
9. Thomas JC. Re -visioning medicine. J Med Humanit. 2014;35(4):405-22. PMID: 25294627 DOI: https://doi.org/10.1007/s10912-014-9304-6
10. Williams D, Tricomi G, Gupta J, Janise A. Efficacy of burnout interventions in the medical education pipeline. Acad Psychiatry. 2015;39(1):47-54. PMID: 25034955 DOI: https://doi.org/10.1007/s40596-014-0197-5
11. Myers M F. The well-being of physician relationships. West J Med. 2001;174(1):30-3. PMID: 11154663 DOI: https://doi.org/10.1136/ewjm.174.1.30
12. Oreskovich MR, Shanafelt T, Dyrbye LN, Tan L, Sotile W, Satele D, et al. The prevalence of substance use disorders in American physicians. Am J Addict. 2015;24(1):30-8. PMID: 25823633 DOI: https://doi.org/10.1111/ajad.12173
13. Hawton K, Clements A, Sakarovitch C, Simkin S, Deeks JJ. Suicide in doctors: a study of risk according to gender, seniority and specialty in medical practitioners in England and Wales, 1979-1995. J Epidemiol Community Health. 2001;55(5):296-300. PMID: 11297646 DOI: https://doi.org/10.1136/jech.55.5.296
14. Chen KY, Yang CM, Lien CH, Chiou HY, Lin MR, Chang HR, et al. Burnout, job satisfaction, and medical malpractice among physicians. Int J Med Sci. 2013;10(11):1471-8. PMID: 24046520 DOI: https://doi.org/10.7150/ijms.6743
15. West C P, Huschka MM, Novotny PJ, Sloan JA, Kolars JC, Habermann TM, et al. Association of perceived medical errors with resident distress and empathy: a prospective longitudinal study. JAMA. 2006;296(9):1071-8. PMID: 16954486 DOI: https://doi.org/10.1001/jama.296.9.1071
16. Pereira-Lima K, Mata DA, Loureiro SR, Crippa JA, Bolsoni LM, Sen S. Association Between Physician Depressive Symptoms and Medical Errors: A Systematic Review and Meta-analysis. JAMA Netw Open. 2019;2(11):e1916097. PMID: 31774520 DOI: https://doi.org/10.1001/jamanetworkopen.2019.16097
17. Deshpande S P, Deshpande SS. Career satisfaction of surgical specialties. Ann Surg. 2011;253(5):1011-6. PMID: 21451395
18. Charles SC, Wilbert JR, Franke KJ. Sued and nonsued physicians’ self-reported reactions to malpractice litigation. Am J Psychiatry. 1985;142(4):437-40. PMID: 3976916 DOI: https://doi.org/10.1176/ajp.142.4.437
19. Kane C. Policy Research Perspectives: Medical Liability Claim Frequency: A 2007-2008 Snapshot of Physicians. Chicago: American Medical Association; 2010.
20. Mello MM, Chandra A, Gawande AA, Studdert DM. National costs of the medical liability system. Health Aff (Millwood). 2010;29(9):1569-77. PMID: 20820010 DOI: https://doi.org/10.1377/hlthaff.2009.0807
21. Balch CM, Oreskovich MR, Dyrbye LN, Colaiano JM, Satele DV, Sloan JA, et al Personal consequences of malpractice lawsuits on American surgeons. J Am Coll Surg. 2011;213(5):657-67. PMID: 21890381 DOI: https://doi.org/10.1016/j.jamcollsurg.2011.08.005
22. Blasco PG. O humanismo médico: em busca de uma humanização sustentável da Medicina. Rev Bras Med. 2014;68(1 n.esp):4-12.
23. Reisch LM, Carney PA, Oster N V, Weaver DL, Nelson HD, Frederick PD, et al. Medical malpractice concerns and defensive medicine: a nationwide survey of breast pathologists. Am J Clin Pathol. 2015;144(6):916-22. PMID: 26572999 DOI: https://doi.org/10.1309/AJCP80LYIMOOUJIF
24. Vale HM, Miyazaki MCOS. Medicina defensiva: uma prática em defesa de quem? Rev Bioét (Impr.). 2019;27(4):747-55.
25. Toaldo AM, Rodrigues O. A publicidade dos atos processuais: uma questão principiológica. Rio Grande: Âmbito Jurídico; 2012.
26. Wambier LR, Almeida FRC, Talamini E. Curso Avançado de Processo Civil: Teoria Geral do Processo e Processo de Conhecimento. São Paulo; Revista dos Tribunais; 2007.
27. Terra C F, Sousa GMSF. Opinião Pública em tempos de mídias sociais: midiatização, comunicação desintermediada e Memes. In: XIII Congresso Brasileiro Científico de Comunicação Organizacional e de Relações Públicas. São Paulo; 2019.
28. Nunes R. Um Tribunal de Exceção chamado Redes Sociais. Jusbrasil; 2017. Disponível em: https://rodrigonunez.jusbrasil.com.br/artigos/417624066/um-tribunal-de-excecao-chamado-redes-sociais
29. Oliveira S P. Razoável duração do processo e morosidade judicial: a jurimetria como subsídio para o gerenciamento de processos judiciais [Dissertação de mestrado]. São Paulo: Universidade Nove de Julho - UNINOVE; 2016.
30. Manzi JE. O juiz e o perito: paralelos e intersecções. Rio Grande: Âmbito Jurídico; 2013.
31. Manzi JE. Senso crítico, senso comum, argumentação jurídica e decisões judiciais. Rev Jus Navigandi. 2012;3151. Disponível em: https://jus.com.br/artigos/21097
32. Cabral Z Jr, Cabral TNX, coords. Justiça Multiportas: Mediação, conciliação, arbitragem e outros meios de solução adequada para conflitos. In: Didier F Jr. Grandes Temas do NCPC. 1ª ed. Salvador: Juspodivm; 2017.
33. Mazzei R, Merçon-Vargas S. Comentários aos artigos 165-175. In: Novo Código de Processo Civil anotado e comparado. In: Figueiredo SDC, ed. São Paulo: Saraiva; 2015. p. 203-15.
34. Brasil. Senado Federal. Art. 156 - Código de processo civil. Brasília: Secretaria de Editoração e Publicações; 2015.
35. Ginsburg J. Federal Arbitration Act — DirecTV, Inc. v. Imburgia. Harvard Law Rev. 2016;130:457-66.
36. Parente EA. Processo arbitral e sistema [Tese de doutorado]. São Paulo: Faculdade de Direito da Universidade de São Paulo; 2009.
37. Guerrero L F. Convenção de arbitragem e processo arbitral. São Paulo: Atlas; 2009. p. 5-11.
38. Briguglio A, Fazzalari E, Marengo R. La nuova disciplina dell’arbitrato: commentario. Milano: Giuffrè; 1994.
39. Brasil. Câmara dos Deputados. Direitos Indisponíveis. Brasília: Câmara dos Deputados; 2008.
40. Botteon LC. Arbitragem e Direito à Saúde: Possibilidade e eficácia de uso do método arbitral para garantir o direito constitucional à saúde; 2013. Disponível em: http://www.publicadireito.com.br/artigos/?cod=c20bb2d9a50d5ac1
41. Lucas RWC. Câmara arbitral de fisioterapia; 2015. Disponível em: https://jus.com.br/artigos/43702/camara-arbitral-de-fisioterapia
42. Ribeiro WC. A Mediação como meio de resolução de conflitos na área de saúde. Rev Dir Sanit. 2018;18(3):62-76. DOI: https://doi.org/10.11606/issn.2316-9044.v18i3p62-76
43. Kass JS, Rose RV. Medical Malpractice Reform--Historical Approaches, Alternative Models, and Communication and Resolution Programs. AMA J Ethics. 2016;18(3):299-310. PMID: 27003002 DOI: https://doi.org/10.1001/journalofethics.2016.18.3.pfor6-1603
44. Kraman SS, Hamm G. Risk management: extreme honesty may be the best policy. Ann Intern Med. 1999;131(12):963-7. PMID: 10610649 DOI: https://doi.org/10.7326/0003-4819-131-12-199912210-00010
45. Moore J, Bismark M, Mello MM. Patients’ Experiences With Communication-and-Resolution Programs After Medical Injury. JAMA Intern Med. 2017;177(11):1595-603. PMID: 29052704 DOI: https://doi.org/10.1001/jamainternmed.2017.4002
46. Lima BG, Campos F, Lopes C P. Mediação e conciliação de conflitos na área da saúde. Unisanta Law Soc Sci. 2018;7(3):523-33.
47. Amirthalingam K. Medical dispute resolution, patient safety and the doctor-patient relationship. Singapore Med J. 2017;58(12):681-4. PMID: 28741011 DOI: https://doi.org/10.11622/smedj.2017073
48. Szmaria SJ, Johnson AM, Mulligan M. Alternative dispute resolution in medical malpractice: A survey of emerging trends and practices. Confl Resolution Quart. 2008;25(1):71-96. DOI: https://doi.org/10.1002/crq.224
49. Metzloff TB. The Unrealized Potential of Malpractice Arbitration. Wake Forest Law Rev. 1996;31:203-30.
50. DeVille KA. The jury is out: pre-dispute binding arbitration agreements for medical malpractice claims: law, ethics, and prudence. J Leg Med. 2007;28(3):333-95. PMID: 17885905 DOI: https://doi.org/10.1080/01947640701554492
51. Du-Hie H. Breakthrough in medical dispute resolution. The Korea Times. 2011 Apr 6. Disponível em: http://www.koreatimes.co.kr/www/news/opinon/2011/04/137_84613.html
52. Larson D. Medical Malpractice Arbitration: Not Business As Usual. Arbitration Law Rev. 2016;8.
1. Departamento de Clínica Médica, Faculdade de Medicina, Universidade de São Paulo,
São Paulo, SP, Brazil.
2. Departamento de Direito Processual, Faculdade de Direito do Largo São Francisco,
Universidade de São Paulo, São Paulo, SP, Brazil.
Corresponding author: Mario Jorge Warde-Filho Rua Senador Cesar Lacerda Vergueiro, 418/41, Sumarezinho, São Paulo, SP, Brazil Zip Code: 05435-010 E-mail: mario.mwpericias@gmail.com
Article received: March 31, 2021.
Article accepted: December 13, 2021.
Conflicts of interest: none.
Institution: Universidade de São Paulo, Faculdade de Medicina, Hospital das Clínicas, São Paulo, SP, Brazil.





 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter