

Review Article - Year 2022 - Volume 37 -
Complex dorsal dislocation of the metacarpophalangeal joint of the long fingers: case report and literature review
Luxação dorsal complexa da articulação metacarpofalangeana dos dedos longos: relato de caso e revisão da literatura
ABSTRACT
Dorsal dislocations of the metacarpophalangeal joint of the fingers are rare injuries that are seen more frequently in young patients secondary to trauma due to forced hyperextension of the finger on the extending hand. They are classified as simple when closed reduction is possible, or complex when reduction by closed methods is not possible given the interposition of peri-articular structures. It is important to distinguish between a simple and complex dislocation because their approach and treatment differ. The objective of this study is to update the clinical approach and the different surgical techniques used in the treatment of complex dislocations. We conducted a bibliographic review on metacarpophalangeal dorsal dislocation of the long fingers, excluding those of the thumb, including the Medline (PubMed interface), SciELO and academic google databases. All the articles reviewed conclude that attempts at closed reduction in these types of injuries are often unsuccessful and often lead to additional complications. Open surgical reduction is the method of choice, allowing joint anatomical recovery with the lowest risk of complications. Postoperative immobilization using a dorsal locking splint is recommended for two weeks followed by rehabilitation by occupational therapy, expecting a normal range of motion at six weeks. The low frequency added to the ignorance of the emergency physician when performing the reduction maneuver can often lead to transform a simple dislocation into a complex one, making it irreducible and injuring adjacent structures, which is why we believe it is essential to know the management of this injury.
Keywords: Metacarpophalangeal joint; Joint dislocations; Open fracture reduction; Palmar plate; Closed fracture reduction.
RESUMO
As luxações dorsais da articulação metacarpofalangeana dos dedos são lesões raras, vistas com mais frequência em pacientes jovens, secundárias a trauma por hiperextensão forçada do dedo na mão que estende. São classificadas como simples, quando a redução fechada é possível; ou complexas, quando a redução por métodos fechados não é possível devido à interposição de estruturas periarticulares. É importante distinguir entre uma luxação simples e uma complexa porque sua abordagem e tratamento são diferentes. O objetivo deste estudo é atualizar a abordagem clínica e as diferentes técnicas cirúrgicas utilizadas no tratamento das luxações complexas. Foi realizada uma revisão bibliográfica sobre a luxação dorsal metacarpofalangeana dos dedos longos, excluindo os do polegar, incluindo o Medline (interface PubMed), SciELO e bancos de dados acadêmicos do Google. Todos os artigos revisados concluem que as tentativas de redução incruenta nesses tipos de lesões costumam ser malsucedidas e levar a complicações adicionais. A redução cirúrgica aberta é o método de escolha, permitindo a recuperação anatômica articular com o menor risco de complicações. A imobilização pós-operatória com uma tala de travamento dorsal é recomendada por duas semanas, seguida por reabilitação por terapia ocupacional, esperando-se uma amplitude de movimento normal em seis semanas. A baixa frequência somada ao desconhecimento do médico emergencista ao realizar a manobra de redução pode, muitas vezes, levar à transformação de um simples deslocamento em complexo, tornando-o irredutível e lesionando estruturas adjacentes, por isso, acreditamos ser fundamental conhecer o manejo desta lesão.
Palavras-chave: Articulação metacarpofalângica; Luxações articulares; Redução aberta; Placa palmar; Redução fechada.
INTRODUCTION
Trauma injuries to the hand are a frequent reason for emergency room visits. Dislocations of the metacarpophalangeal joint (MCP) of the long fingers are rare and serious injuries, given the connective tissue support present around this joint and its basal position in the hand1,2. Joint stability is enhanced by bilateral attachments of the deep, transverse metacarpal ligaments, which unite and stabilize the palmar plate. This intimate relationship provides stability but is also responsible for the irreducibility of the lesion. The index and little fingers do not have this bilateral support and, therefore, are more prone to injuries3.
Dislocations are classified as simple when closed reduction is possible, with the volar plate remaining fixed to the proximal phalanx in these cases and the finger being highly hyperextended in the resting position (60 to 90º); or complex when reduction by closed methods is not possible due to the interposition of periarticular structures, and its clinical presentation is even rarer4. Most authors agree that the volar plate is the reason for the impossibility of closed reduction of these lesions5,6.
Clinically, they present with the metacarpophalangeal joint slightly hyperextended (30-40º) and the interphalangeal joints slightly flexed, adding to palpation of the metacarpal head (MTP) at the volar level and decreased range of motion of the MCP.
It is important to distinguish between a simple and a complex dislocation because their approach and treatment are different.
Simple dislocations (or subluxations) can be treated non-surgically by closed reduction, while attempts at a closed reduction in complex dislocations are often unsuccessful and often lead to additional complications. Open surgical reduction is the method of choice in these injuries, allowing joint anatomical recovery with the lowest risk of complications.
Adequate treatment and knowledge of hand injuries are extremely important, conditioning the patient’s functional prognosis and limiting the impact and health costs of a long absence from work. It is essential to determine the best treatment to achieve full hand functionality recovery and return to work as soon as possible, emphasizing that this type of injury occurs, in its vast majority, in the working population.
OBJECTIVE
The present study aims to update the clinical and therapeutic approach, analyzing the advantages and disadvantages of the different surgical techniques used in treating complex dislocations based on a clinical case operated by the author.
METHODS
A narrative review of the literature on dorsal metacarpophalangeal dislocation of the long fingers of the hand was performed. The search was performed in Medline (Pubmed interface), SciELO and Google Scholar databases. The keywords were used: “metacarpophalangeal joint,” “dislocation,” “open reduction,” and “volar plate.”
Abstracts of articles from the first search were analyzed by the authors, selecting publications that met the following inclusion criteria: clinical trials, case series, case reports and literature reviews that included patients diagnosed with dorsal metacarpophalangeal dislocation of long fingers, articles published in English, Spanish and Portuguese and no restrictions were established regarding the time of publication.
Exclusion criteria were: metacarpophalangeal dislocation of the first finger and publications without an identifiable scientific article format.
A clinical case operated by the author is presented, which was evaluated in the emergency department of the Hospital de Clínicas de Montevideo - Uruguay, from June to December 2020.
This work is carried out following the guidelines of the Ethics Committee of Hospital de Clínicas, approval number 32. The images of patients in this publication have informed consent.
CLINICAL CASE
Female patient, 52 years old, right-handed, presented a fall from her height on her left hand in extension. She consulted the emergency room 12 hours after the trauma.
The energetic hyperextension determined a complex dorsal dislocation of the metacarpophalangeal joint of the second finger of the left hand, presenting in the emergency with a pathological attitude, with the MCP joint in 30º of extension and the interphalangeal joints slightly flexed, with the impossibility of joint mobilization of the second ray (Figure 1).
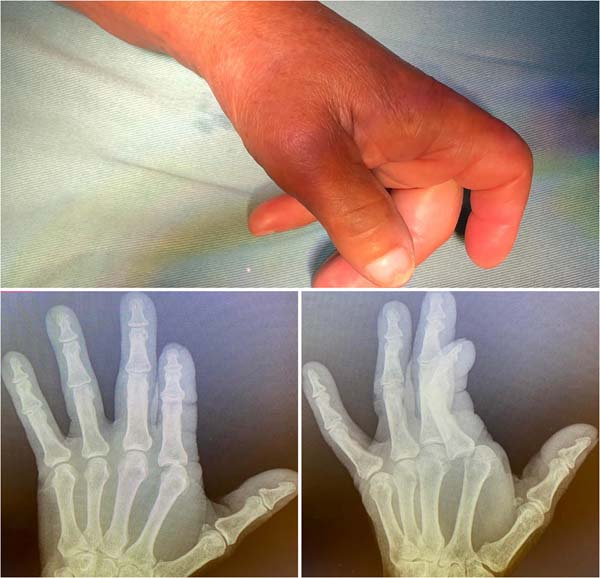
Hand radiographs confirmed the dislocation described without showing the presence of an interposed sesamoid (Figure 2).

A closed reduction attempt was made under a regional wrist block without therapeutic success, so open reduction was coordinated in the operating room under general anesthesia.
It was performed in a closed field with a pneumatic cuff, volar approach through sinusoidal insertion centered on the head of the second metacarpal. The characteristic findings of these lesions were identified: disinserted proximal volar plate, interposed and blocking the joint, radial collateral nerve in close relationship with the metacarpal head, which was identified and protected during surgery, and displacement of the flexor to ulnar and lumbrical towards the radial, producing a loop around the head of the second MTP. Longitudinal sectioning of the A1 pulley and volar plate was performed to restore normal joint anatomy. Figure 3 shows the normal attitude of the hand after reduction. There were no intra or postoperative complications.
Immobilization was performed with a locked dorsal brachydigital splint for two weeks, followed by rehabilitation by occupational therapy consisting of passive and active range of motion exercises and complementary therapies to control edema and optimize the healing process. The patient had a good evolution, recovering to the full range of motion at eight weeks.
DISCUSSION
The pathogenesis and anatomy of these lesions were initially reported by Kaplan7 in 1957, who described that the various structures involved contribute to the irreducibility of dislocation by closed methods. In 1876, Farabeuf described its management and treatment based on the description of MCP dislocations of the thumb8.
Dorsal metacarpophalangeal dislocations of the long fingers usually occur in patients with a history of trauma from a fall with an outstretched hand with the finger in hyperextension. They can occur in all MCP joints, being more frequent in the external fingers2,4 due to their greater vulnerability to trauma and the lack of stabilization by the adjacent deep, transverse metacarpal ligaments. Most of the reports found in the literature are from the index finger; among these, less than 10% are open9.
Dislocations are classified as simple when closed reduction is possible; in these cases, the volar plate remains fixed in the proximal phalanx, and the finger is highly hyperextended in the resting position (60 to 90º); or complex when reduction by closed methods is not possible, due to the interposition of periarticular structures, and its clinical presentation is less frequent2,4.
It is important to distinguish between a simple and a complex dislocation because their approach and treatment are different. Simple dislocations (or subluxations) can be treated non-surgically by closed reduction. The maneuver is performed by gently flexing the wrist to relax the flexor tendons and then applying gradual dorsal-to-volar pressure on the dorsal base of the proximal phalanx, flexing the MCP10 joint. Longitudinal traction instead of force applied based on the first phalanx can transform a simple displacement into a complex one, making it irreducible and injuring adjacent structures, which can lead to degenerative arthritis, with a decrease in the final range of motion8,10-12.
Complex dislocations are those cases in which the volar plate detaches from its junction with the metacarpal and is interposed between the proximal phalanx and this phalanx2,4,13. It has been reported that the metacarpal head can become trapped between adjacent tendon structures. In the case of the index finger, the flexors move ulnarly, and the lumbricals move radially; in the fifth finger, the abductor tendon and the flexor brevis of the fifth finger move ulnarly and the lumbricals move radially2,4. The swimming ligament can move dorsally, and the superficial transverse metacarpal ligament proximally7.
Clinically, they present with the metacarpophalangeal joint slightly hyperextended (30-40º) and the interphalangeal joints slightly flexed secondary to the dorsal displacement of the proximal phalanx, palpation of the MTP head at the volar level and decreased range of motion of the MCP11. It can also be accompanied by a slight deviation in the anteroposterior plane, in the case of the index finger, towards the ulnar14. The wrinkling of the palmar skin on the metacarpal head is recognized as a pathognomonic sign, which can also associate skin wounds with exposure to the metacarpal head5.
At the time of trauma, the hyperextension force determines the rupture of the weakest membranous portion of the palmar plate at its insertion into the metacarpal, which determines its displacement to be stuck in the joint2.
Regarding the paraclinical, frontal, lateral and oblique radiographs should be requested.
An anteroposterior radiograph usually shows an increase in joint space and a displacement of the base of the phalanx in an ulnar direction. The presence of an interposed sesamoid within the joint, usually moving distally and ulnarly from the joint, is a characteristic finding in the diagnosis of volar plate entrapment and seals the closed irreducibility of these lesions.
Generally, they are better visualized in the oblique approach8,11,14,15. In these cases, Kaplan defined the treatment as “triple release,” adding the extraction of the volar plate from the joint with the sesamoid. These bones are present in approximately 70% of the population; they appear to cover the MTP head at 12 years of age. Generally, they are single on the second and third MTP and can be bent on the first, fourth and fifth rays14.
In the lateral approach to radiography, the base of the proximal phalanx is dorsal to the metacarpal head and may or may not associate osteochondral fractures in the dorsal head of the same.
Complex dislocations require surgical treatment through an approach that can be volar, dorsal, lateral or combined16.
The need for surgical reduction is due to the region’s anatomy, which contributes to its complexity and difficulty.
Kaplan described the structures responsible for the irreducible nature of the dislocation, such as the superficial and deep, transverse metacarpal ligaments, the swimming ligament, the flexor and the lumbrical tendons3,7.
The deep, transverse metacarpal ligament plays a key role in MCP joint stability. They are closely linked to the volar plate, and together they constitute the most relevant structures in irreducibility8,15,17. This ligament, which is tense on the dorsum of the dislocated metacarpal head, acts as a mechanical block, holding the joint in place and making it impossible to reduce. Gerrand & Shearer15, in their review of the case, proposed a reduction to release the remaining union of the volar plate with the transverse metacarpal ligament, preserving its distal insertion in the neck of the proximal phalanx.
As a characteristic finding, the metacarpal head is trapped between adjacent structures: flexors and lumbricals, and the volar plate detach from its proximal insertion in the neck of the MTP. It is systematically displaced to be searched in the dorsal joint space in the MTP head, which acts as a mechanical obstruction in closed reduction2,14.
The closed reduction maneuver in these cases employing traction is usually insufficient and generates a loop for the metacarpal head, producing more trauma to the adjacent tissues. Some authors recommend, even after the diagnosis of dislocation, avoiding closed maneuvers and opting for open reduction as the first treatment option5,14,15.
In their systematic review, Diaz Abele et al.1 recommended reducing closed reduction attempts in the preoperative period and performing open reduction with minimal delay. Previous attempts at reduction are potentially traumatic and can lead to further damage to the joint surfaces and even the creation of a cord around the metacarpal head due to excessive traction. Surgery usually requires a volar plate cut, and the authors recommend repair with figure-eight stitches and subsequent immobilization with a dorsal block splint for two weeks, followed by rehabilitation by the occupational therapy team.
Open reduction is performed in a surgical center under regional or general anesthesia, with a bloodless field, under a pneumatic cuff that allows for a correct balance of the lesion and the correct identification of injured structures. Currently, the safety of using local anesthesia with epinephrine in hand surgery is well known, which provides anesthesia and a bloodless field through vasoconstriction, eliminating the need for a pneumatic tourniquet and general anesthesia18.
There are controversies regarding the most appropriate surgical approach for reduction. In his initial description, Kaplan defends the volar approach, like other authors2,5,9,15. This approach allows direct access to the lesion and subsequent anatomical restoration of the joint, possibly repairing the volar plate. This may be related to a lower risk of late instability2.
It is performed through a zigzag or sinusoidal skin incision, which allows distal and proximal extension over the MCP joint11,15. Care must be taken with the radial collateral nerve and artery in injuries to the second and third fingers and with the ulnar collateral nerve and artery in injuries to the fourth and fifth fingers2,15. Neurovascular damage can be avoided by careful dissection and more atraumatic tissue management.
For reduction, some authors3 refer to the need to section the remaining union of the deep, transverse ligament attached to the palmar plate and incise the superficial and transverse swimming ligaments.
Releasing the A1 pulley decreases the tension of the loop around the metacarpal. The proximal phalanx and volar plate can usually be repositioned into their anatomical positions by relieving tension on the tendon.
If necessary, the palmar plate5,7 can also be released and minimal traction applied to the flexor tendons to perform the reduction maneuver by moving the MTP head dorsally and making a slight flexion of the joint from ulnar to radial, flexing the phalanx proximal.
Some authors1,2,14,15 repair the palmar plate with figure-eight stitches with non-absorbable sutures after the maneuver, and others do not, justifying that the periarticular structures limit the risk of posterior instability6.
In their review, Diaz Abele et al.1 reported better results when repairing it, having the greatest active metacarpophalangeal range of motion in these cases. In cases where bone fixation of the palmar plate was performed, a worse result was obtained regarding the joint range of motion in the postoperative period. Gerrand & Shearer15, in their review of the case, performed the suture of the volar plate to the periosteum of the metacarpal in the proximal direction.
The authors who defend the dorsal approach17,19,20 among its advantages highlight the good exposure of the volar plate and the low risk of injury to the digital nerves. This approach is also useful in those dislocations associated with osteochondral fractures of the metacarpal head that may require fixation or excision of the fragment depending on its size. The main disadvantage is that the volar plate, which is split longitudinally for reduction, cannot be repaired by this approach.
O’Neill et al.21, in their case report published in 2021, used a dorsal approach, obtaining good results with an early functional return one month after the injury, despite the delay in definitive treatment. A centralized incision is made over the joint, and the extensor tendon and joint capsule must be sectioned longitudinally. The volar plate that appears immediately interposed is also sectioned longitudinally to subsequently perform reduction by flexing the wrist and finger.
Barry et al.17, in their study combining their clinical experience with the dissection of anatomical samples from cadaver hands, compared the volar and dorsal approaches. In cadaveric dissection, the vulnerability of the radial neurovascular bundle concerning the metacarpal head of the second toe is highlighted. The advantage of the dorsal approach is highlighted, as it is simpler and has no risk of injuring vital structures, with the advantage of being able to address any osteochondral fracture associated with the head of the MTP. There was no apparent difference in stability after reduction by either approach. They also emphasize that in all dissections, reduction necessarily required partial or total release of the deep, transverse ligament, while sectioning of the superficial and swimming transverse ligaments was only necessary for better exposure. The volar approach allowed for anatomic restoration of the joint and access to volar plate repair; this author did not find studies that evaluated its relationship with long-term instability. Barry et al.17 recommend a volar approach for more experienced hand surgeons and a dorsal approach for those starting surgery.
Pereira et al.22 reported a case of dislocation of the MCP of the index finger in which an open reduction was performed via a lateral approach, finding the interposition of the volar plate and an osteochondral fragment that blocked the reduction.
A straight longitudinal incision was made on the lateral aspect of the MCP joint; the joint capsule was sectioned longitudinally above the collateral ligament, and the volar neurovascular bundle and the dorsal nerve branches were identified and protected. This approach gained access to the dorsal and volar structures, and the intervening volar plate was reduced and reinserted with a 4.0 Vycril suture. An osteochondral fragment was identified and fixed with a 1.7mm screw.
Regarding complications, one of the most encountered early is loss of joint amplitude, which is more frequently manifested in lesions with a delayed surgical resolution, severe joint infections associated with exposed dislocations, and damage to the digital collateral nerve2. Among the late complications, osteoarthrosis of the joint and osteonecrosis have been described, also associated with repeated failed attempts at closed reduction, open dislocations and prolonged immobilization.
Postoperative immobilization is a controversial issue. Rubin et al.13, in their case series, performed immediately protected mobilization and used immobilization in one patient for three days.
In their systematic review, Diaz Abele et al.1 suggest immobilization with a locked dorsal splint for two weeks followed by rehabilitation by occupational therapy, which consists of passive and active range-of-motion exercises, and complementary therapies to control edema and optimize the healing process23.
McLaughlin10, in his work, reports a less satisfactory range of motion in complex dislocations immobilized for more than two weeks.
Durakbasa & Guneri2, on the other hand, performed immobilizations in their series of seven cases for an average of three weeks, with a mean follow-up of 91 months, reporting excellent functional results in all their patients, standing out as important data in the result that five of them correspond to the pediatric age. Recovery with a normal range of motion is generally expected within 6 weeks.
CONCLUSIONS
Complex dislocations of the metacarpophalangeal joint are rare lesions diagnosed by clinical findings with a slightly hyperextended metacarpophalangeal joint, mild ulnar deviation of the involved finger, volar palpation of the MCP head, and the presence of dimples in the palmar skin.
Attempts at closed reduction of complex dislocations are often unsuccessful, and repeated attempts often lead to additional complications. Open surgical reduction is the method of choice for treating these injuries, allowing the joint anatomy to recover with the lowest risk of complications.
Even after diagnosing complex dislocation, it is recommended to avoid closed maneuvers and opt for open reduction as the first treatment option.
There are several approaches described. The volar approach allows direct access to the lesion and anatomical restoration of the joint with the possibility of repairing the volar plate, which may be related to a lower risk of late instability. The dorsal approach also offers good exposure to the lesion, with a lower risk of injury to the digital nerves, and also provides good access in cases that associate MCP osteochondral fractures.
Immobilization with a dorsal locking splint for two weeks is recommended, followed by rehabilitation and therapy to control edema and optimize the healing process.
As emergency physicians evaluate these patients, knowledge of this injury, proper diagnosis and prompt referral to hand surgeons for surgical treatment are essential and determine the functional prognosis of these injuries.
REFERENCES
1. Diaz Abele J, Thibaudeau S, Luc M. Open metacarpophalangeal dislocations: literature review and case report. Hand (N Y). 2015;10(2):333-7. DOI: 10.1007/s11552-014-9646-6
2. Durakbasa O, Guneri B. The volar surgical approach in complex dorsal metacarpophalangeal dislocations. Injury. 2009;40(6):657-9. DOI: 10.1016/j.injury.2008.10.027
3. Nussbaum R, Sadler AH. An isolated, closed, complex dislocation of the metacarpophalangeal joint of the long finger: a unique case. J Hand Surg Am. 1986;11(4):558-61. DOI: 10.1016/S0363-5023(86)80198-8
4. Stiles BM, Drake DB, Gear AJ, Watkins FH, Edlich RF. Metacarpophalangeal joint dislocation: indications for open surgical reduction. J Emerg Med. 1997;15(5):669-71.
5. Mudgal CS, Mudgal S. Volar open reduction of complex metacarpophalangeal dislocation of the index finger: a pictorial essay. Tech Hand Up Extrem Surg. 2006;10(1):31-6. DOI: 10.1097/00130911-200603000-00006
6. Wright CS. Compound dislocations of four metacarpophalangeal joints. J Hand Surg Br. 1985;10(2):233-5. DOI: 10.1016/0266-7681(85)90025-7
7. Kaplan EB. Dorsal dislocation of the metacarpophalangeal joint of the index finger. J Bone Joint Surg Am. 1957;39-A(5):1081-6.
8. Green DP, Terry GC. Complex dislocation of the metacarpophalangeal joint. Correlative pathological anatomy. J Bone Joint Surg Am. 1973;55(7):1480-6.
9. Imbriglia JE, Sciulli R. Open complex metacarpophalangeal joint dislocation. Two cases: index finger and long finger. J Hand Surg Am. 1979;4(1):72-5. DOI: 10.1016/S0363-5023(79)80108-2
10. McLaughlin HL. Complex “locked” dislocation of the metacarpophalangeal joints. J Trauma. 1965;5(6):683-8.
11. Elghoul N, Bouya A, Jalal Y, Zaddoug O, Benchakroun M, Jaafar A. Complex metacarpophalangeal joint dislocation of the litter finger: A sesamoid bone seen within joint. What does it mean? Trauma Case Rep. 2019;23:100225. DOI: 10.1016/j.tcr.2019.100225
12. An MT, Kelley JP, Fahrenkopf MP, Kelpin JP, Adams NS, Do V. Complex Metacarpophalangeal Dislocation. Eplasty. 2020;20:ic3.
13. Rubin G, Orbach H, Rinott M, Rozen N. Complex Dorsal Metacarpophalangeal Dislocation: Long-Term Follow-Up. J Hand Surg Am. 2016;41(8):e229-33. DOI: 10.1016/j.jhsa.2016.05.010
14. Silberman WW. Clear view of the index sesamoid: a sign of irreducible metacarpophalangeal joint dislocation. JACEP. 1979;8(9):371-3. DOI: 10.1016/S0361-1124(79)80262-2
15. Gerrand CH, Shearer H. Complex dislocation of the metacarpophalangeal joint of the index finger with sesamoid entrapment. Injury. 1995;26(8):574-5. DOI: 10.1016/0020-1383(95)98148-C
16. Becton JL, Christian JD Jr, Goodwin HN, Jackson JG 3rd. A simplified technique for treating the complex dislocation of the index metacarpophalangeal joint. J Bone Joint Surg Am. 1975;57(5):698-700.
17. Barry K, McGee H, Curtin J. Complex dislocation of the metacarpo-phalangeal joint of the index finger: a comparison of the surgical approaches. J Hand Surg Br. 1988;13(4):466-8. DOI: 10.1016/0266-7681(88)90182-9
18. Lalonde DH, Martin A. Epinephrine in local anesthesia in finger and hand surgery: the case for wide-awake anesthesia. J Am Acad Orthop Surg. 2013;21(8):443-7.
19. Bohart PG, Gelberman RH, Vandell RF, Salamon PB. Complex dislocations of the metacarpophalangeal joint. Clin Orthop Relat Res. 1982;(164):208-10.
20. Yadav SK, Nayak B, Mittal S. New approach to second metacarpophalangeal joint dislocation management: the SKY needling technique. Eur J Orthop Surg Traumatol. 2021;31(1):189-92. DOI: 10.1007/s00590-020-02728-w
21. O’Neill ES, Qin MM, Chen KJ, Hansdorfer MA, Doscher ME. Dislocation of the metacarpophalangeal joint of the index finger requiring open reduction due to the presence of an intra-articular sesamoid bone. SAGE Open Med Case Rep. 2021;9:2050313X211021180. DOI: 10.1177/2050313X211021180
22. Pereira JM, Quesado M, Silva M, Carvalho JDD, Nogueira H, Alves J. The Lateral Approach in the Surgical Treatment of a Complex Dorsal Metacarpophalangeal Joint Dislocation of the Index Finger. Case Rep Orthop. 2019;2019:1063829. DOI: 10.1155/2019/1063829
23. Afifi AM, Medoro A, Salas C, Taha MR, Cheema T. A cadaver model that investigates irreducible metacarpophalangeal joint dislocation. J Hand Surg Am. 2009;34(8):1506-11. DOI: 10.1016/j.jhsa.2009.06.001
1. Hospital de Clínicas Dr. Manuel Quintela, Cátedra de Cirugía Plástica, Reparadora
y Estética, Montevidéu, Uruguai
Corresponding author: Victoria Hernández Sosa Mac Eachen, 1302, Montevidéu, Uruguai. Zip code: 11300, E-mail: victoria.hernandezsosa@gmail.com
Article received: October 22, 2021.
Article accepted: April 7, 2022.
Conflicts of interest: none.







 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter