

Review Article - Year 2022 - Volume 37 -
Adjuvant-induced autoimmune syndrome triggered by silicone breast implants: systematic review
Síndrome autoimune induzida por adjuvantes desencadeada por implantes mamários de silicone: revisão sistemática
ABSTRACT
Adjuvant-induced autoimmune syndrome (ASIA) and its diagnostic criteria were described by Shoenfeld in 2011, relating symptoms of autoimmunity to adjuvants, such as silicone, present in breast implants. This systematic review aimed to gather data from the literature on symptomatology, incidence and proposed treatments for ASIA caused by silicone breast implants (SBI). Searches were carried out in PubMed, LILACS, Embase and Cochrane databases, using the descriptors "Autoimmune Syndrome Induced by Adjuvants," "Breast implant," and "Silicone Implant Incompatibility Syndrome." The search strategy generated 95 articles, of which 20 were included in the review. The authors suggest three main theories to explain the development of the syndrome: genetic predisposition, silicone bleeding and the formation of a periprosthetic capsule. The most frequently described clinical manifestations include chronic fatigue, arthralgia, myalgia, and cognitive and sleep disorders. There is no consensus on laboratory findings and associated risk factors; recent studies propose expanding the diagnostic criteria initially described. Adequate treatment remains controversial, ranging from medications to prosthesis explantation. Although the reviewed articles suggest the existence of ASIA related to SBI, its precise pathophysiology is unknown, the symptoms reported are nonspecific, and the time between exposure and the onset of manifestations is uncertain. This systematic review concludes that, to date, there is not enough scientific evidence to establish the causality of the development of adjuvant-induced autoimmune syndrome resulting from silicone breast implants.
Keywords: Breast implants; Silicone elastomers; Adjuvants, immunologic; Autoimmunity; Systematic Review.
RESUMO
A síndrome autoimune induzida por adjuvantes (ASIA) e seus critérios diagnósticos foram descritos por Shoenfeld em 2011, relacionando sintomas de autoimunidade a adjuvantes, como o silicone, presente em próteses mamárias. Essa revisão sistemática objetivou reunir dados da literatura sobre a sintomatologia, a incidência e os tratamentos propostos para ASIA causada por implantes mamários de silicone (IMS). Foram realizadas pesquisas nas bases de dados PubMed, LILACS, Embase e Cochrane, utilizando os descritores "Autoimmune Syndrome Induced by Adjuvants", "Breast implant" e "Silicone Implant Incompatibility Syndrome". A estratégia de busca gerou 95 artigos, dos quais 20 foram incluídos na revisão. São as três as principais teorias sugeridas pelos autores para explicar o desenvolvimento da síndrome: predisposição genética, silicone bleeding e a formação de uma cápsula periprótese. As manifestações clínicas mais frequentemente descritas incluem fadiga crônica, artralgia, mialgia, distúrbios cognitivos e do sono. Não há consenso sobre os achados laboratoriais e os fatores de risco associados, além disso, estudos recentes propõem a ampliação dos critérios diagnósticos inicialmente descritos. O tratamento adequado permanece controverso, envolvendo desde o uso de medicações até o explante da prótese. Apesar dos artigos revisados sugerirem a existência da ASIA relacionada aos IMS, sua fisiopatologia precisa é desconhecida, os sintomas relatados são inespecíficos e o tempo entre a exposição e o surgimento das manifestações é incerto. Por meio dessa revisão sistemática, conclui-se que, até o presente momento, não existem evidências científicas suficientes para estabelecer a causalidade do desenvolvimento da síndrome autoimune induzida por adjuvantes decorrente de implantes mamários de silicone.
Palavras-chave: Implante mamário; Elastômeros de silicone; Adjuvantes imunológicos; Autoimunidade; Revisão sistemática.
INTRODUCTION
Silicone breast implants (SBI) have been used in medical practice since 1962 in reconstructive and aesthetic surgery1. For a long time, silicone was considered a biologically inert and harmless substance2. However, in recent years, the presentation of a series of symptoms of autoimmune diseases common by patients with breast implants has led authors to correlate the symptoms with the presence of the implant. In 1964, Miyoshi had already described this association3 and, more recently, in 2011, Schoenfeld & Agmon-Levin4 described and proposed criteria for what they called adjuvant-induced autoimmune syndrome (ASIA)4.
ASIA involves a group of immune-mediated diseases related to previous exposure to adjuvants. Diseases include squalene-related Gulf War Syndrome; macrophagic myofasciitis, related to aluminum hydroxide; and siliconosis, related to silicone, which is present in breast implants and other materials frequently used in medical practice. The emergence of the syndrome is associated with the interaction between environmental factors, previous exposure to adjuvants, induction of autoimmunity and loss of immune tolerance in genetically predisposed individuals2,4.
The diagnostic criteria for ASIA proposed by Shoenfeld & Agmon-Levin include, as major criteria, exposure to external stimuli, as adjuvants, the subsequent appearance of clinical symptoms of autoimmune diseases involving the musculoskeletal, joint and nervous systems, improvement of symptoms after removal of the causal agent and typical biopsy presentation of the involved organs. And, as minor criteria, the presence of autoantibodies, certain human leukocyte antigens (HLA), involvement of autoimmune diseases and other clinical manifestations1.
OBJECTIVE
Through a systematic review of the medical literature, this work aimed to gather information about ASIA in patients with silicone breast implants, compiling Dice about pathophysiology, symptomatology and treatments currently available.
METHODS
The topic was reviewed systematically to obtain the best available evidence. The PRISMA5 protocol cannot be followed, as many articles relevant to the subject were not systematic reviews or randomized clinical trials.
Articles were obtained by searching PubMed, Cochrane, LILACS and Embase databases. The search descriptors were used in the following systematization: (Autoimmune Syndrome Induced by Adjuvants) AND ((Breast implant) OR (Silicone Implant Incompatibility Syndrome)). The search was not limited by publication date, language, or study design.
Inclusion criteria included studies published in indexed journals that addressed the topic of ASIA associated with silicone breast implants or silicone implant incompatibility syndrome. Exclusion criteria were: (i) Studies dealing with lymphoma or other neoplasms; (ii) Studies in animal models; (iii) Study type: case reports or case series with less than three cases; (iv) Language: study not available in English, Spanish or Portuguese; (v) Study not published or in the pre-publication phase; (vi) ASIA syndrome caused by another adjuvant; (vii) Breast implants of materials other than silicone.
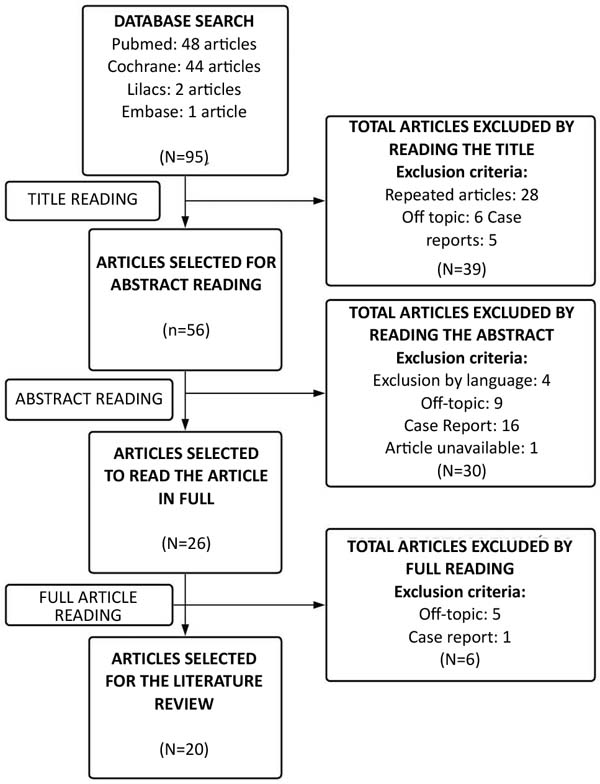
After searching the databases, all articles found were initially screened based on their titles. Studies whose titles permeated the themes of ASIA and breast implants or SIIS were included for analysis, and duplicate articles were excluded. Then, the selected articles had their abstracts read, and those that met the inclusion criteria, and did not fit the exclusion criteria, were kept. Finally, the articles were read in full; the appropriate ones were selected for the literature review. Three independent researchers screened and selected articles; an agreement was necessary to exclude any articles. The search was not limited by the publication date, language or study design, and all articles on the topic were published until March 2021, when the article selection process took place.
The present study does not require approval by the Ethics Committee and application of the Free and Informed Consent Form, as it is a secondary study, which does not involve tests on patients, data obtained directly from patients and tests on animal models.
RESULTS AND DISCUSSION
The search strategy generated 95 articles, 28 of which were repeated. In the end, 20 articles (21%) were selected (Figure 1) based on a database search for the literature review (Annex 1).
Pathophysiology
Adjuvants are substances capable of increasing the specific antigen-immune response; for this, they mimic molecules preserved throughout evolution, binding to receptors and potentiating the activity of antigen-presenting cells3,4.
The silicone implant incompatibility syndrome and the other diseases encompassed by ASIA share a common background: the genetic predisposition of affected individuals to develop autoimmunity after exposure to adjuvants3,6.
The pathogenesis that leads to autoimmunity after SBI implantation is still unclear, but some plausible mechanisms have already been proposed. The expression of HLA-DRB1 and HLA-DQB1 antigens seems to be linked to the onset of autoimmunity in patients with breast implants6. Furthermore, SIIS may be related to the phenomenon of silicone bleeding, in which silicone molecules cross the limits of the implant and can be dispersed throughout the body even with an intact prosthesis7. Bleeding silicone can also transform the foreign body reaction expected in the formation of the periprosthetic capsule, after implant insertion, into a chronic inflammatory process8.
Silicone molecules trigger an inflammatory process, which consists of the capture of particles by macrophages, triggering the production of cytokines and reactive oxygen species (ROS). Subsequent apoptosis of these cells releases the particles, restarting the process. Another mechanism is the production of interleukin (IL)-17, which stimulates intense migration of neutrophils, the secretion of enzymes and ROS. Furthermore, the transport of silicone-containing particles to lymph nodes may result in an adjuvant effect7-9.
In normal individuals, the formation of the periprosthetic capsule depends on the production of tumor necrosis factor α (TNF-α) and tissue growth factor β (TGF-β), produced by macrophages and T lymphocytes. These factors stimulate the multiplication of fibroblasts and extracellular matrix deposition, resulting in capsule formation and subsequent fibrotic reaction. In predisposed individuals, the continuous activation of macrophages and the predominance of T helper lymphocytes 17 concerning regulatory T lymphocytes are associated with the chronicity of inflammatory reactions and autoimmunity8.
Another theory suggests the participation of infectious agents as triggers for the development of pathological immune-mediated responses to adjuvants. In it, the adjuvant effect of microbial molecules, through the non-antigenic activation of the immune system and the expression of several regulatory cytokines, can trigger the disease3.
Clinical manifestations
Typically, chronic fatigue is the most prevalent symptom, affecting up to 98% of patients10,11. The manifestation may be present from awakening and not improve after rest, compromising daily activities1,12. However, there are disagreements in the literature, and a recent study showed a lower prevalence in patients with SBI concerning a control group (18.2% vs. 47.7%, p=0.03)13.
Sleep disturbances are frequent complaints involving both the initiation and maintenance of sleep. This manifestation, which can affect up to 78% of cases10, is associated with cognitive disorders and memory alterations, commonly reported in the syndrome1,12.
Arthritis and arthralgia may be present as early symptoms of the syndrome1,12. Studies differ as to their prevalence, ranging from 31.8% to 91%10,13,14. In most cases, there is morning stiffness lasting more than one hour1,12.
Furthermore, up to 90% of patients may have myalgia or muscle weakness, with electromyography alterations in up to 53% of cases1,12. Again, there are discrepancies between publications; a study in Argentina indicated this symptom as less frequent in patients with SBI than in their control group (18.2% vs. 75%, p<0.0001)13.
Xerostomia and xerophthalmia are other important complaints, affecting 75% of patients1,3,8. 30-50% of patients develop Raynaud’s phenomenon; in some cases, there are changes in nail capillaroscopy1,3,10,12.
Allergic manifestations such as nasal and eye itching, rhinorrhea, sneezing, coughing and skin symptoms are reported in 50-80% of patients1,10,12.
Less frequent symptoms related to ASIA include fever, respiratory tract symptoms, recurrent cystitis, livedo reticularis, alopecia and gastrointestinal tract disorders1,10,12,14.
Some studies suggest a correlation of ASIA with other rheumatological disorders, such as fibromyalgia and rheumatoid arthritis11,13,15, more frequently, but also with lupus, scleroderma, Sjögren, among others14,16.
The average time between exposure to SBI and the manifestation of symptoms is not consensual in the literature, ranging from 4 to 16.1 years10,11,13,17. There are descriptions of cases in which the onset of symptoms occurred in just one year after exposure, and another reaching 42 years10,13,15,17.
Laboratory Findings
The presence of autoantibodies is common in ASIA. Antinuclear factor (ANA) can be found in up to 56% of cases1,3,18. Other antibodies include anti-Ro, anti-La, anti-dsDNA, anti-Scl-70, anticardiolipin, cyclic citrullinated peptide antibody, rheumatoid factor IgM, an anti-neutrophil cytoplasmic antibody can be found, although less frequently1,18.
Specific HLA alleles, such as HLA-DRB1 and HLA-DQB1, constantly related to rheumatologic diseases, are frequently found in ASIA carriers17.
Vitamin D deficiency is described in some studies and may be present in up to 50% of patients with the syndrome1,12,19.
Diagnostic Criteria
In his original work, Shoenfeld suggested using major and minor criteria for diagnosing ASIA (Chart 1).
| Major Criteria |
|---|
| Exposure to an external stimulus (silicone, infection, vaccine) prior to the manifestations Appearance of typical manifestations: |
| o Myalgia, myositis, or muscle weakness |
| o Chronic fatigue, non-restorative sleep, sleep disturbances |
| o Neurological manifestations (especially associated with demyelination) |
| o Cognitive deficit, memory loss |
| o Heartburn, xerostomia |
| Improvement after the removal of the external factor |
| Histological findings of Organs involved organs that suggest autoimmunity |
| Minor Criteria |
| Appearance of autoantibodies or antibodies against the suspected adjuvant. Other clinical manifestations (e.g., irritable bowel syndrome) |
| Specific HLA (e.g., HLA DRB1, HLA DQB1) Involvement of another autoimmune disease |
Risk factors
The risk factors that predispose to the emergence of the syndrome are still not well elucidated in the literature. It is believed that patients with previously documented autoimmune diseases, especially those related to HLA-DRB1 and the PTPN22 gene, and those with a family predisposition to develop autoimmune diseases6,11, are more affected by the syndrome1,11.
Studies suggest that patients with a history of atopy also seem to have a greater predisposition to developing ASIA1,2,11. Previous episodes of an autoimmune reaction to adjuvants, such as those that occurred after immunization with vaccines containing adjuvants2,20, and some environmental factors such as smoking and obesity are cited as possible risk factors1.
Treatment
No drug treatment cures the syndrome, but some medications such as corticosteroids, hydroxychloroquine, minocycline and doxycycline can help reduce symptoms1,12.
In patients who have allergic symptoms, the use of antiallergics can contribute to the improvement of the condition. In those with vitamin D deficiency, vitamin 1 replacement is recommended. Patients who smoke should also be instructed to quit smoking1. Patients with the syndrome who manifest symptoms related to fibromyalgia should be encouraged to practice physical activities1.
The silicone explant can be advised in patients with multiple complaints and refractory to drug treatments. Studies show that 60 to 80% of patients show improvement in symptoms, especially fatigue, arthralgia and myalgia, after removing the breast implant1,6,10,12,14,21. It is believed that patients who do not show improvement in symptoms after removing the silicone implant have the material spread throughout the body1.
Study limitations
The recent description of ASIA added to the lack of consensus on this entity’s existence, making studies on the subject scarce. The search in the databases was not able to include studies with strong scientific evidence, such as clinical trials and meta-analyses. At the same time, the studies included in the review were mostly carried out in specialized immunology and rheumatology centers, which could generate a selection bias and compromise external validity. The long time between implantation and manifestation of symptoms allows the existence of a confounding bias, in which the trigger of autoimmunity could be the exposition to an adjuvant other than SBI. Excluding articles by language may limit access to relevant knowledge.
CONCLUSION
Since silicone breast implants are widely used in plastic surgery, breast augmentation and reconstruction, the autoimmune syndrome induced by adjuvants becomes a topic of great relevance.
The autoimmune character, the wide spectrum of symptoms and the variable time between the silicone implant and the clinical manifestations make the diagnosis of ASIA inaccurate.
In addition, the pathophysiology and risk factors related to the development of the syndrome remain unclear. The history of previous autoimmune diseases was the most prevalent risk factor in the studies reviewed; however, it is not known whether ASIA acts as an aggravating factor or a trigger for the development of autoimmunity symptoms.
The diagnosis of ASIA through the criteria proposed by Shoenfeld lacks consensus and validation in the academic environment, as well as the definitive treatment because even the prosthesis explant was ineffective for all patients.
It is concluded that, despite some evidence, the correlation between silicone breast implants and adjuvant-induced autoimmunity syndrome cannot be confirmed, and further studies with strong scientific evidence are needed.
REFERENCES
1. Cohen Tervaert JW, Colaris MJ, van der Hulst RR. Silicone breast implants and autoimmune rheumatic diseases: myth or reality. Curr Opin Rheumatol. 2017;29(4):348-54.
2. Goren I, Segal G, Shoenfeld Y. Autoimmune/inflammatory syndrome induced by adjuvant (ASIA) evolution after silicone implants. Who is at risk? Clin Rheumatol. 2015;34(10):1661-6.
3. Alijotas-Reig J. Human adjuvant-related syndrome or autoimmune/inflammatory syndrome induced by adjuvants. Where have we come from? Where are we going? A proposal for new diagnostic criteria. Lupus. 2015;24(10):1012-8.
4. Shoenfeld Y, Agmon-Levin N. ‘ASIA’ - autoimmune/inflammatory syndrome induced by adjuvants. J Autoimmun. 2011;36(1):4-8. DOI: 10.1016/j.jaut.2010.07.003
5. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
6. Borba V, Malkova A, Basantsova N, Halpert G, Andreoli L, Tincani A, et al. Classical Examples of the Concept of the ASIA Syndrome. Biomolecules. 2020;10(10):1436.
7. Caravantes-Cortes MI, Roldan-Valadez E, Zwojewski-Martinez RD, Salazar-Ruiz SY, Carballo-Zarate AA. Breast Prosthesis Syndrome: Pathophysiology and Management Algorithm. Aesthetic Plast Surg. 2020;44(5):1423-37. DOI: 10.1007/s00266-020-01663-9
8. Bassetto F, Scarpa C, Vindigni V, Doria A. The periprosthetic capsule and connective tissue diseases: a piece in the puzzle of autoimmune/autoinflammatory syndrome induced by adjuvants. Exp Biol Med (Maywood). 2012;237(10):1117-22.
9. Medina, Ch FM, Calle JA, Ledesma OEG, Echeverry JC. Implantes Mamarios, Eventos Adversos Y Complicaciones Poco Frecuentes: Hallazgos Por Mamografía, Ecografía Y Resonancia Magnética. Rev Colomb Radiol. 2016;27(2):4434-40.
10. Colaris MJL, de Boer M, van der Hulst RR, Cohen Tervaert JW. Two hundreds cases of ASIA syndrome following silicone implants: a comparative study of 30 years and a review of current literature. Immunol Res. 2017;65(1):120-8.
11. Khoo T, Proudman S, Limaye V. Silicone breast implants and depression, fibromyalgia and chronic fatigue syndrome in a rheumatology clinic population. Clin Rheumatol. 2019;38(5):1271-6.
12. Cohen Tervaert JW. Autoinflammatory/autoimmunity syndrome induced by adjuvants (ASIA; Shoenfeld’s syndrome): A new flame. Autoimmun Rev. 2018;17(12):1259-64.
13. Rojas Tessel R, Alonso Lopez D, Buschiazzo E, Juarez R V, Aciar M; Crespo Espindola ME. Prevalence of Rheumatologic Symptoms and Specific Rheumatic Diseases in Patients with History of Breast Implants. Ann Rheum Dis. 2016;75(Suppl 2):1217.
14. Maijers MC, de Blok CJ, Niessen FB, van der Veldt AA, Ritt MJ, Winters HA, et al. Women with silicone breast implants and unexplained systemic symptoms: a descriptive cohort study. Neth J Med. 2013;71(10):534-40.
15. Lastra OLV, Dominguez MdPC, Jara LJ, Ramirez GM. Autoimmune/inflammatory syndrome induced by adjuvants due to silicone breast implant and rheumatic diseases. Ann Rheum Dis. 2019;78(Suppl 2):2111.
16. Cohen Tervaert JW, Kappel RM. Silicone implant incompatibility syndrome (SIIS): a frequent cause of ASIA (Shoenfeld’s syndrome). Immunol Res. 2013;56(2-3):293-8.
17. Soriano A, Butnaru D, Shoenfeld Y. Long-term inflammatory conditions following silicone exposure: the expanding spectrum of the autoimmune/inflammatory syndrome induced by adjuvants (ASIA). Clin Exp Rheumatol. 2014;32(2):151-4.
18. Shoenfeld Y, Maślińska M. Autoimmune (auto-inflammatory) syndrome induced by adjuvants - ASIA. Reumatologia. 2013;51(2):101-7.
19. Colafrancesco S, Agmon-Levin N, Perricone C, Shoenfeld Y. Unraveling the soul of autoimmune diseases: pathogenesis, diagnosis and treatment adding dowels to the puzzle. Immunol Res. 2013;56(2-3):200-5.
20. Meroni PL. Autoimmune or auto-inflammatory syndrome induced by adjuvants (ASIA): old truths and a new syndrome? J Autoimmun. 2011;36(1):1-3. DOI: 10.1016/j.jaut.2010.10.004
21. Pavlov-Dolijanovic S, Vujasinovic Stupar N. Women with silicone breast implants and autoimmune inflammatory syndrome induced by adjuvants: description of three patients and a critical review of the literature. Rheumatol Int. 2017;37(8):1405-11.
Annex 1. Main characteristics of the selected articles.
| Author | Year | Title | Article type | Relevant findings |
|---|---|---|---|---|
| Tervaert, J. W. C. et al. | 2017 | Silicone breast implants and autoimmune rheumatic diseases: Myth or reality | Revision | It associates IMSs with a group of patients with complaints of fatigue, cognitive disorders, arthralgia, myalgia, fever, xerophthalmia and xerostomia. It indicates that silicone molecules can migrate from the implant through the body, inducing a chronic inflammatory process and that the IMS explant results in the improvement of symptoms in most patients. |
| Goren, I. et al. | 2015 | Autoimmune/inflammatory syndrome induced by adjuvant (ASIA) evolution after silicone implants. Who is at risk? | Revision | It relates IMS and autoimmunity, suggesting ways to identify individuals at higher risk for developing silicone-induced ASIA and thus recommending avoiding IMS in some cases (e.g., individuals with a previous diagnosis of autoimmune diseases or genetic predisposition to immune system hyperactivity). |
| Alijotas-Reig, J. | 2015 | Human adjuvant-related syndrome or autoimmune/inflammatory syndrome induced by adjuvants. Where have we come from? Where are we going? A proposal for new diagnostic criteria. | Opinion article | It proposes new diagnostic criteria for ASIA based only on objective clinical and laboratory data to be discussed and validated. |
| Schoenfeld, Y; Agmon-Levin, N. | 2010 | ‘ASIA’ - Autoimmune/inflammatory syndrome induced by adjuvants | Revision | Discusses the role of adjuvants in the pathogenesis of immune-mediated diseases. |
| Borba, V. et al. | 2020 | Classical Examples of the Concept of the ASIA Syndrome. | Revision | It describes the diagnostic criteria proposed by Shoenfeld and the manifestations of autoimmunity that may be present in the syndrome. Studies conducted by the authors themselves are cited, which found antibodies against G protein-coupled receptors of the autonomic nervous system circulating in the serum of patients with ASIA and improvement of symptoms after silicone explantation. |
| Caravantes, C. et al. | 2020 | Breast Prosthesis Syndrome: Pathophysiology and Management Algorithm | Revision | It mentions the pathophysiological mechanisms involved in developing silicone-related autoimmune and inflammatory diseases and their relationship with human genetic variability. |
| Basetto, F. et al. | 2012 | The periprosthetic capsule and connective tissue diseases: A piece in the puzzle of autoimmune/autoinflammatory syndrome induced by adjuvants | Revision | It seeks to understand the immunological mechanisms responsible for the emergence and development of autoimmune diseases in patients with breast implants, focusing on the role of cytokines in susceptible individuals. |
| Medina. F. M. et al. | 2016 | Implantes mamarios, eventos adversos y complicaciones poco frecuentes: hallazgos por mamografía, ecografía y resonancia magnética. | Revision | Summarizes the main complications related to breast implants. It describes the main clinical manifestations of ASIA and possible findings that can be found in imaging studies in patients with silicone implants who manifest the syndrome. |
| Colaris, M. J. L. et al. | 2016 | Two hundreds cases of ASIA syndrome following silicone implants: a comparative study of 30 years and a review of current literature | Case series and Review | It compares two cohort studies with a sample of 100 patients each, with an interval of 30 years between them. It concludes that silicone can be a chronic stimulus for the immune system and that no major changes in the clinical manifestations were reported over the last three decades. |
| Khoo, T. et al. | 2019 | Silicone breast implants and depression, fibromyalgia and chronic fatigue syndrome in a rheumatology clinic population | Control case |
This study analyzed the medical records of patients from a Rheumatology clinic. In the described data, we looked for whether the patients had silicone breast implants and compared them with a control group of patients from the same clinic without implants. Compared to the control group, patients had a higher incidence of fibromyalgia and chronic fatigue. |
| Tervaert, J. W. C. et al. | 2018 | Autoinflammatory/autoimmunity syndrome induced by adjuvants (ASIA; Shoenfeld’s syndrome): A new flame | Revision | The study indicates the main symptoms of ASIA and relates them to the chronic inflammatory process by the foreign body reaction to the implant. It also indicates the pre-existence of allergic diseases as an important risk factor for the development of the syndrome and the silicone explant as a way to alleviate the symptoms. |
| Tessel, R. R. et al. | 2016 | AB0923 Prevalence of Rheumatologic Symptoms and Specific Rheumatic Diseases in Patients with History of Breast Implants. | Control case |
The study aimed to compare a group of patients with breast implants and a control group of patients without an implant. Both groups were being followed up with rheumatologists. Patients with breast implants had a higher incidence of arthritis compared to the control group. |
| Maijers, M. C. et al. | 2014 | Women with silicone breast implants and unexplained systemic symptoms: A descriptive cohort study | Case series | It indicates the main signs and symptoms of ASIA and points out that most women with the syndrome have a history of allergies. It also states that 69% of them have reduced symptoms after explantation, and this option should be considered for the referred patients. |
| Lastra, O. L. V. et al. | 2019 | Autoimmune/inflammatory syndrome induced by adjuvants due to silicone breast implant and rheumatic diseases | Case series | It points to the prevalence of ASIA associated with IMS at 15%. The main associated rheumatologic diseases were systemic sclerosis, fibromyalgia and rheumatoid arthritis. A family history, allergies and smoking association was also observed in patients with the syndrome. |
| Tervaert, J. W. C. et al. | 2013 | Silicone implant incompatibility syndrome (SIIS): A frequent cause of ASIA (Shoenfeld’s syndrome). | Case series | The study provides a brief explanation of the adjuvants and the immunological mechanisms triggered by them. Patients referred to the Maastricht University Medical Center were investigated for the presence of breast implants and followed up. According to the symptoms presented, they were diagnosed with ASIA. |
| Soriano, A. et al. | 2014 | Long-term inflammatory conditions following silicone exposure: The expanding spectrum of the autoimmune/inflammatory syndrome induced by adjuvants (ASIA) | Opinion article | It compiles information on the relationship between silicone and autoimmunity and its probable pathophysiology due to the material’s not completely inert nature. Finally, it discusses the need to assess the predisposition to autoimmune diseases by HLA genotyping and to screen for rheumatologic diseases prior to surgeries for cosmetic purposes. |
| Shoenfeld, Y. et al. | 2013 | Autoimmune (auto-inflammatory) syndrome induced by adjuvants-ASIA. | Revision | The study addresses the different types of adjuvants, the way they interfere with the immune response and the different manifestations they can trigger. These manifestations are described as being part of a single syndrome: ASIA. |
| Colafrancesco, S. et al. | 2013 | Unraveling the soul of autoimmune diseases: Pathogenesis, diagnosis and treatment adding dowels to the puzzle | Opinion article | It discusses the pathogenesis of adjuvant-induced autoimmune diseases, their interactions with genetic components, and immune defects, and points to environmental and hormonal factors as possible triggers. |
| Meroni, P. L. | 2011 | Autoimmune or auto-inflammatory syndrome induced by adjuvants (ASIA): Old truths and a new syndrome? | Revision | |
| Pavlov-Dolijanovic, S.; Stupar, NV | 2017 | Women with silicone breast implants and autoimmune inflammatory syndrome induced by adjuvants: description of three patients and a critical review of the literature | Case series and Review | The article questions whether the silicone molecule is inert due to the wide symptomatology and diagnosis of ASIA in the cases in the article. |
1. Universidade Federal do Paraná, Curitiba, PR, Brazil
CMG Conception and design study, Conceptualization, Formal Analysis, Investigation, Methodology, Project Administration, Realization of operations and/or trials, Writing - Original Draft Preparation, Writing - Review & Editing.
CNS Conception and design study, Conceptualization, Formal Analysis, Investigation, Methodology, Project Administration, Realization of operations and/or trials, Writing - Original Draft Preparation, Writing - Review & Editing.
RMGA Conception and design study, Conceptualization, Formal Analysis, Investigation, Methodology, Project Administration, Realization of operations and/or trials, Writing - Original Draft Preparation, Writing - Review & Editing.
MCCO Final manuscript approval, Supervision.
Corresponding author: Caio Munaretto Giacomazzo R. Padre Camargo, 280, Alto da Glória, Curitiba, PR, Brazil. Zip Code: 80060-240, E-mail: caiomunagiaco@gmail.com
Article received: August 26, 2021.
Article accepted: December 13, 2021.
Conflicts of interest: none.






 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter